Abstract
Objectives
To evaluate the diagnostic performance of the LI-RADS (v2014) on gadoxetate-enhanced MRI prospectively applied in actual practice.
Methods
We retrospectively reviewed the prospectively written radiology reports of 143 treatment-naïve at-risk patients who underwent gadoxetate-enhanced liver MRI from January to December 2014, and identified 202 hepatic observations categorized using the LI-RADS. The diagnostic performances of LI-RADS categories for hepatocellular carcinoma (HCC) and hepatic malignancy were calculated.
Results
Twenty (69.0 %) of 29 LR-4, 73 (97.3 %) of 75 LR-5, and all of five (100 %) LR-5V observations were HCCs. The remaining two (2.7 %) LR-5 observations were combined hepatocellular-cholangiocarcinomas, while 10 (76.9 %) of 13 LR-M observations were HCCs. The sensitivity and specificity of LR-5/5V for HCC were 60.5 % and 97.3 %, respectively. Including LR-M in the diagnostic criteria for HCC increased sensitivity (68.2 %, p = 0.002) but decreased specificity without statistical significance (93.2 %, p = 0.154). LR-5/5V/M yielded sensitivity of 68.9 % and specificity of 100.0 % for hepatic malignancy.
Conclusions
LI-RADS v2014 was successfully applied on gadoxetate-enhanced MRI in clinical practice. LR-5/5V was the most specific diagnostic measure for HCC, but most LR-M observations were HCCs and a considerable portion of non-HCC malignancies were categorized as LR-4 or LR-5.
Key Points
• LR-5/5V provided a highly specific diagnosis for HCC.
• Half of non-HCC malignancies were categorized as LR-4 or LR-5.
• The majority of LR-M observations were finally diagnosed as HCCs.
• More sensitive diagnosis of HCC was feasible with LR-5/5V/M on gadoxetate-enhanced MRI.
• Observations in either LR-5/5V or LR-M categories were definitely malignant.
Similar content being viewed by others
Introduction
The Liver Imaging Reporting and Data System (LI-RADS) has been developed to standardize the diagnostic process by dynamic computed tomography (CT) or magnetic resonance imaging (MRI) in patients at risk for hepatocellular carcinoma (HCC) [1, 2]. By using the LI-RADS for reporting the interpretations of liver MRI examinations, imaging features can be clearly defined, and their significance can be better communicated with other radiologists or clinicians. In the LI-RADS, instead of applying a binary decision (HCC or not HCC) for the interpretation of hepatic observations, the relative probability of a diagnosis is assigned using the 5-point scale, with values ranging from definite benignity (LI-RADS category 1, LR-1) to definite HCC (LR-5). In the latest LI-RADS v2017, if an observation is probably or definitely malignant and is not specific for HCC, LR-M is allocated, and the treatment strategy may change based on the clinical context [2].
The reliability and accuracy of applying the LI-RADS in liver MRI using extracellular contrast materials have been validated in previous studies by the retrospective interpretation of hepatic lesions detected in patients at risk of HCC [3, 4]. The 2014 version of LI-RADS covers the use of hepatobiliary agents in dynamic MRI and includes some hepatobiliary features as ancillary findings [5, 6]. Applicability of LI-RADS v2014 in gadoxetate-enhanced MRI has been assessed recently in retrospective studies [7,8,9], with potential improvement of sensitivity suggested by adding hepatobiliary phase imaging findings in the interpretation [9]. One of these studies showed that some atypical intrahepatic cholangiocarcinomas (CCs) can be falsely categorized into the LR-5 or LR-5V categories [7].
However, to our knowledge, the accuracy of the prospective application of LI-RADS in the interpretation of gadoxetate-enhanced MRI has not been reported. The purpose of this study was to evaluate the diagnostic performance of the LI-RADS on gadoxetate-enhanced MRI prospectively applied in actual practice.
Materials and methods
Study population
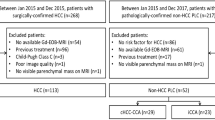
This retrospective cohort study was approved by our institutional review board and the requirement for patient consent was waived. The patients were selected based on the Standards for Reporting Diagnostic Accuracy Studies (STARD) guidelines [10]. From January to December 2014, 1,266 consecutive patients who were at-risk for HCC (HBsAg [+], anti-HCV Ab [+] or liver cirrhosis of any aetiology) and underwent liver dynamic MRI at our institution were potentially eligible (Fig. 1). As LI-RADS v2014 defers to the definition of high-risk population by other guidelines, such as the American Association for the Study of Liver Diseases (AASLD) and European Association for the Study of the Liver (EASL), we used the definitions of AASLD and EASL for selection of at-risk patients for HCC [1, 11, 12]. Of these, 750 patients who were previously treated for HCC were excluded. We also excluded 205 patients whose MRI reports were not written using the LI-RADS (90 patients without any observation necessitating LI-RADS categorization and 115 patients with observations in which LI-RADS was not applied). Forty-three patients with MRIs using extracellular agents were also excluded. Of the remaining 268 patients, 125 patients with observations that underwent nonsurgical treatment without obtaining histopathological diagnosis (85 patients) or with observations that could not be conclusively diagnosed based on the follow-up imaging (40 patients with observations who showed an insufficient diameter increase for threshold growth and who had a follow-up period shorter than 18 months) were also excluded. If there were four or more observations in the same category, we included only the three largest observations to reduce cluster bias. Therefore, 202 hepatic observations with final diagnoses in 143 patients were included in the final analysis. The median age of the 143 patients was 58 years (range, 32–81 years), and the cohort included 120 men with a median age of 58 years (range, 32–81 years) and 23 women with the median age of 64 years (range, 34–81 years). Viral infection was the main cause of liver disease, with hepatitis B virus infection in 110 (76.9 %) patients. A majority (94.4 %) of the patients was of Child-Pugh class A at the time of examination (Table 1).
Participant flow. Among the 1,266 at-risk patients who underwent liver dynamic MRI at our institution in 2014, we excluded 750 patients with prior treatment history for hepatocellular carcinoma (HCC), 205 patients with MRI reports not written using the LI-RADS, 43 patients with MRIs using extracellular agents, and 125 patients with observations with no reference standard. Therefore, 202 hepatic observations with final diagnoses in 143 patients were included in the final analysis (67 benign lesions, 129 HCCs and six non-HCC malignancies). OM other non-HCC malignancy. N in parenthesis represents the number of observations
Reference standards
By reviewing the medical records, the final diagnoses were determined along with the clinical information. If an operation or core-needle biopsy was performed, histopathological diagnosis was used as a reference standard. 125 observations were histopathologically diagnosed by hepatic resection (n = 108), liver transplantation (n = 10) or core-needle biopsy (n = 7) after a mean interval of 35 days from MRI evaluation (range, 1–464 days).
If an observation progressed to LR-5 or LR-5V categories during follow-up, due to new arterial phase hyperenhancement, new washout appearance or threshold growth (an increase of more than 50 % in the diameter within 6 months or over a twofold increase in the diameter during more than 6 months), it was diagnosed as HCC after a mean follow-up duration of 412 days (range, 91–895 days). If there was no increase in the diameter during the 18-month follow-up period or longer, it was considered benign after a mean follow-up duration of 724 days (range, 554–943 days). Therefore, 59 benign lesions and 18 HCCs were diagnosed based on the follow-up imaging.
MR imaging
MRI scans were acquired using the 3.0-T Magnetom Trio Tim (Siemens Medical Solutions, Erlangen, Germany), Intera Achieva or Ingenia (Philips Medical Systems, Best, The Netherlands), or Discovery MR750w (GE Medical Systems, Waukesha, WI, USA) scanners. Axial images were acquired with a field of view of 44 cm × 33 cm or 40 cm × 30 cm depending on the patient’s body size. The protocol included the acquisition of dual-echo T1-weighted gradient-echo images (in- and out-of phases), T1-weighted 3-dimensional (3D) gradient-echo dynamic contrast-enhanced images, navigator-triggered single or multi-shot T2-weighted images, and diffusion-weighted images at b-values of 0, 50, 400 and 800 s/mm2 (Table 2). For the dynamic imaging, T1-weighted 3D gradient-echo images were obtained before and after contrast media administration according to our routine protocol for evaluation of hypervascular focal liver lesion, where 10 ml of gadoxetate disodium (Primovist; Bayer Schering Pharma AG, Berlin, Germany) was injected at a rate of 1 ml/s, followed by 20 ml of 0.9 % saline chaser at the same flow rate (off-label use based on the previous evidences) [13, 14]. The arterial phase scan was started about 3 s after the peak aortic enhancement calculated by the test-bolus technique (Siemens) or after visualization of the abdominal aorta on the bolus-tracking technique (Philips, GE). The portal venous, late portal venous and transitional phases were obtained at 60–70 s, 90–100 s and 120–150 s, respectively, after contrast injection. The hepatobiliary phase was obtained at 20 min after contrast administration.
One of the seven abdominal radiologists with more than 5 years of experience in liver MR imaging interpreted liver MRIs using LI-RADS in actual practice. Clinical information, such as cause of liver disease, and previous imaging studies were available to the readers during the interpretation.
Statistical analysis
The diagnostic accuracy of the LI-RADS categories for HCC and hepatic malignancy was described by the sensitivity, specificity and accuracy with 95 % confidence intervals (CIs). For HCC diagnosis, calculation was performed using LR-5/5V, which was compared with using LR-5/5V and LR-M, and using LR-4 and LR-5/5V, respectively. For the diagnosis of hepatic malignancy, calculation was performed using LR-5/5V and LR-M, which was compared with using LR-4, LR-5/5V and LR-M. A weighted least-squares method was used for the abovementioned comparison of diagnostic measures. A chi-squared test was used for comparison of accuracies between diagnosis of HCC and that of hepatic malignancy using LR-5/5V/M. The Statistical Analysis Software (SAS) version 9.4 (SAS Institute Inc., Cary, NC, USA) was used. Results with p values less than 0.05 were considered statistically significant.
Results
The final diagnoses of 202 observations with reference standards were as follows: 129 HCCs, six other hepatic malignancies (two CCs and four combined HCC-CCs), and 67 benign lesions (Table 3). Among the benign lesions, seven regenerative or dysplastic nodules (one LR-2, four LR-3 and two LR-4), and one haemangioma (LR-2) were confirmed histologically after surgery.
HCCs were diagnosed in none of the 11 (0 %) LR-1, four (14.8 %) of 27 LR-2, 17 (40.5 %) of 42 LR-3, 20 (69.0 %) of 29 LR-4, 73 (97.3 %) of 75 LR-5 (Fig. 2), all of the five (100 %) LR-5V and ten (76.9 %) of 13 LR-M observations. Notably, of the 13 LR-M lesions, only three (23.1 %) were non-HCC malignancies (two CCs and one combined HCC-CC), while the remainder were HCCs (Fig. 3). In addition, three of six (50 %) non-HCC malignancies were categorized as LR-4 or LR-5. Of the four HCCs (14.8 % of LR-2) categorized as LR-2, one was histologically diagnosed on resection 443 days after the MRI, while the other three were clinically diagnosed after a mean follow-up period of 593 days (range, 230–791 days). Of the 17 HCCs (40.5 % of LR-3) assigned as LR-3, five of eight (62.5 %) histologically confirmed HCCs were early HCCs, defined as vaguely nodular, very well differentiated lesions, less than 2 cm in diameter. Nine LR-3 observations were diagnosed as HCCs on imaging obtained after a mean follow-up period of 309 days (range, 91–895 days). Among the eight LR-4 observations diagnosed as benign, two were histologically confirmed to be high-grade dysplastic nodules, while the others showed no change or a decrease in the size during a follow-up period of 18 months or longer. One (3.4 %) of 29 LR-4 observations and two (2.7 %) of 75 LR-5 observations were confirmed to be combined HCC-CCs (Fig. 4).
Axial T1-weighted gadoxetate-enhanced 3D gradient-echo MR images in a 77-year-old man with chronic hepatitis B. a-d A 42-mm hypointense nodule is seen on the precontrast image (a) in the lateral surface of the hepatic segment V, showing hyperenhancement on the arterial phase (b), a washout and capsule appearance on the portal venous phase (c), and hypointensity on the hepatobiliary phase (d). A LI-RADS category 5 was assigned preoperatively. Surgical resection confirmed the diagnosis of hepatocellular carcinoma
Axial T1-weighted gadoxetate-enhanced 3D gradient-echo MR images in a 65-year-old man with C-viral liver cirrhosis. a-d A 35-mm hypointense nodule with infiltrative margins is seen on the precontrast image (a) in the hepatic segment VII, showing a peripheral rim-like hyperenhancement on the arterial phase (b), partial washout on the portal venous phase (c), and hypointensity on the hepatobiliary phase image (d). A LI-RADS category M was assigned, but surgical resection revealed the diagnosis of hepatocellular carcinoma
Axial T1-weighted gadoxetate-enhanced 3D gradient-echo MR images in a 32-year-old man with chronic hepatitis B. a-d A 24-mm hypointense nodule is seen on the precontrast image (a) in the lateral surface of the hepatic segment VIII, showing hyperenhancement on the arterial phase (b), a washout appearance on the portal venous phase (c), and hypointensity on the hepatobiliary phase (d). A LI-RADS category 5 was assigned. Surgical resection revealed a combined hepatocellular and cholangiocarcinoma
The sensitivity and specificity for HCC diagnosis using LR-5/5V were 60.5 % (95 % CI, 52.0–68.9) and 97.3 % (95 % CI, 93.5–99.9), respectively. Including LR-M in the diagnostic criteria for HCC increased sensitivity (68.2 % vs. 60.5 %, p = 0.002) but decreased specificity without statistical significance (93.2 % vs. 97.3 %, p = 0.154) in comparison to using LR-5/5V only (Table 4). Including LR-4 in the diagnostic criteria for HCC increased sensitivity (76.0 % vs. 60.5 %, p < 0.001) but decreased specificity (84.9 % vs. 97.3 %, p = 0.003) in comparison to using LR-5/5V only.
Using LR-5/5V and LR-M for the diagnosis of hepatic malignancy yielded sensitivity of 68.9 % (95 % CI, 61.1–76.7) and specificity of 100.0 % (95 % CI, 100.0–100.0). Adding LR-4 to LR-5/5V/M for the diagnosis of hepatic malignancy increased sensitivity (84.4 % vs. 68.9 %, p < 0.001) but decreased specificity (88.1 % vs. 100.0 %, p = 0.005).
Discussion
Our study shows that LI-RADS v2014 has been successfully applied in gadoxetate-enhanced MRI for the evaluation of patients at risk for HCC in clinical practice. LR-5/5V was the most specific diagnostic measure for HCC. However, a considerable portion of non-HCC malignancies were categorized as LR-4 or LR-5 and most of LR-M observations were confirmed as HCCs, demonstrating the difficulty of perfectly specific diagnosis of HCC using LI-RADS v2014.
The sensitivity and specificity of the LR-5/5V categories for the diagnosis of HCC were comparable with the results of a study by Darnell et al. [4] using an extracellular contrast material, and the sensitivity showed a trend of improvement (sensitivity, 60.5 % vs. 42.3 %; specificity, 97.3 % vs. 98.2 %). This might be attributable to the additional use of hepatobiliary phase imaging, as indicated in the study by Chen et al. [9], in which the sensitivity was observed to increase by approximately 10 % when the hepatobiliary phase images were added. The sensitivity also tended to be higher than that seen in another study applying the LI-RADS retrospectively (60.5 % vs. 48.9 %) [8], which may be due to the inclusion of observations with tumour invading veins and no limitation on the size of observations in our study. However, the sensitivity of LR-5/5V was lower than that of LR-5/5V/M in this study since 7.8 % of HCCs were categorized into LR-M and consisted a majority (76.9 %) of LR-M observations.
The specificity using LR-4 and LR-5/5V for HCC diagnosis was lower in our study than that observed in the previous study (84.9 % vs. 96.4 %) [4], possibly due to a larger proportion of benign LR-4 observations included in the present study (28 % vs. 4 %). In addition, it was common in our series to treat LR-4 observations by transarterial embolization or other kinds of locoregional therapy. If these observations had not been excluded, the proportion of HCC might have been higher in LR-4 observations.
Notably, three (50 %) combined HCC-CCs among six non-HCC malignancies were assigned to the LR-4 or LR-5 categories in our study. Difficulties in the preoperative diagnosis of combined HCC-CC using imaging have been well described [15, 16]. A previous study suggested that consideration of ancillary features might improve the diagnosis of combined HCC-CCs as most of them showed at least one ancillary feature favouring non-HCC malignancies [17]. However, our results have shown that consideration of the ancillary features might also increase the rate of false categorization of HCCs into the LR-M category. We believe that this was not related with the use of gadoxetate, since evaluation of the ancillary features was not specific to the contrast material.
In this study, we have observed that the majority of observations in the LR-M category turned out to be HCCs. Therefore, LR-5/5V/M showed a significantly higher sensitivity for HCC than LR-5/5V without significantly compromising the specificity. In a patient population with a much higher prevalence of HCC than that of non-HCC malignancy as in our series, using only LR-5/5V for HCC diagnosis, albeit most specific, may lead to narrowing of treatment option for patients with HCC categorized into the LR-M category. In Eastern Asia, with the highest incidence of HCC [18], highly sensitive diagnosis of HCC is considered important for early detection of HCC even at the expense of an ‘acceptable’ decrease in specificity [19]. A new diagnostic measure for HCC in observations 2 cm or smaller has been proposed in order to increase sensitivity on gadoxetate-enhanced MRI without significantly sacrificing specificity [20]. In this regard, the diagnostic measure of LR-5/5V/M may be useful for significantly improving the sensitivity of HCC on gadoxetate-enhanced MRI while maintaining the specificity in an acceptable range.
An LR-M category has been devised to distinguish probably (or definitely in v2017 [2]) malignant observations that are not specific for HCC [6]. Therefore, we have evaluated the diagnostic performance of probably or definitely malignant categories (LR-4/5/5V/M and LR-5/5V/M) for hepatic malignancy. LR-5/5V/M yielded specificity of 100.0 % for hepatic malignancy, indicating that observations in LR-5/5V or LR-M categories were definitely malignant. LR-M observations in this study can be interpreted as ‘definitely malignant, not necessarily HCC’.
There are some limitations to our study. First, we excluded the examinations in which the LI-RADS were not prospectively applied at the initial interpretation. However, we believe that there was no serious selection bias because non-application of the LI-RADS in those cases was simply due to individual preferences of the radiologists. Second, HCCs diagnosed by follow-up imaging had long time intervals between the initial and final examinations, therefore the clinically diagnosed HCCs may include initially benign observations that evolved afterward. However, these observations behaved more aggressively than the observations that were stable during follow-up. We intended to minimize selection bias by not excluding these observations in the analysis. Third, definitely or probably benign observations were reported with the radiologists’ discretion; hence, the numbers of LR-1 and LR-2 observations were lower than actual numbers of benign lesions. Fourth, the latest 2017 version of LI-RADS was not applied to these patients as we intended to investigate the outcome of our prospective reading. Finally, this was a single-centre study and we could not investigate interobserver or intraobserver variability. However, we believe that our data, which pools the categorization results by several readers during actual MRI interpretation, can better reflect the clinical practice and may be broadly applied.
In conclusion, LI-RADS v2014 has been successfully applied in clinical practice with gadoxetate-enhanced MRI for patients at risk for HCC. LR-5/5V was the most specific diagnostic measure for HCC, but most of LR-M observations were confirmed as HCCs and a considerable portion of non-HCC malignancies were categorized as LR-4 or LR-5.
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- LI-RADS:
-
Liver Imaging Reporting and Data System
- LR:
-
LI-RADS category
- MRI:
-
Magnetic resonance imaging
References
Mitchell DG, Bruix J, Sherman M, Sirlin CB (2015) LI-RADS (Liver Imaging Reporting and Data System): summary, discussion, and consensus of the LI-RADS Management Working Group and future directions. Hepatology 61:1056–1065
American College of Radiology (2017) Liver Imaging reporting and data system version 2017. Available via http://www.acr.org/Quality-Safety/Resources/LIRADS. Accessed 1 Jul 2017
Petruzzi N, Mitchell D, Guglielmo F, O'Kane P, Deshmukh S, Roth C, Shortt C, Balfour S, Parker L (2013) Hepatocellular carcinoma likelihood on MRI exams: evaluation of a standardized categorization system. Acad Radiol 20:694–698
Darnell A, Forner A, Rimola J, Reig M, Garcia-Criado A, Ayuso C, Bruix J (2015) Liver Imaging Reporting and Data System with MR Imaging: Evaluation in nodules 20 mm or smaller detected in cirrhosis at screening US. Radiology 275:698–707
Hope TA, Fowler KJ, Sirlin CB, Costa EA, Yee J, Yeh BM, Heiken JP (2015) Hepatobiliary agents and their role in LI-RADS. Abdom Imaging 40:613–625
American College of Radiology (2014) Liver imaging reporting and data system version 2014. Available via http://www.acr.org/Quality-Safety/Resources/LIRADS. Accessed 19 Nov 2016
Joo I, Lee JM, Lee SM, Lee JS, Park JY, Han JK (2016) Diagnostic accuracy of liver imaging reporting and data system (LI-RADS) v2014 for intrahepatic mass-forming cholangiocarcinomas in patients with chronic liver disease on gadoxetic acid-enhanced MRI. J Magn Reson Imaging 44:1330–1338
Choi SH, Byun JH, Kim SY, Lee SJ, Won HJ, Shin YM, Kim PN (2016) Liver Imaging Reporting and Data System v2014 with gadoxetate disodium-enhanced magnetic resonance imaging: Validation of LI-RADS category 4 and 5 criteria. Investig Radiol 51:483–490
Chen N, Motosugi U, Morisaka H, Ichikawa S, Sano K, Ichikawa T, Matsuda M, Fujii H, Onishi H (2016) Added value of a gadoxetic acid-enhanced hepatocyte-phase image to the LI-RADS system for diagnosing hepatocellular carcinoma. Magn Reson Med Sci 15:49–59
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, Lijmer JG, Moher D, Rennie D, de Vet HC, Kressel HY, Rifai N, Golub RM, Altman DG, Hooft L, Korevaar DA, Cohen JF (2015) STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. Radiology 277:826–832
Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Feuerlein S, Boll DT, Gupta RT, Ringe KI, Marin D, Merkle EM (2011) Gadoxetate disodium–enhanced hepatic MRI: dose-dependent contrast dynamics of hepatic parenchyma and portal vein. AJR Am J Roentgenol 196:W18–W24
Vogl TJ, Kümmel S, Hammerstingl R, Schellenbeck M, Schumacher G, Balzer T, Schwarz W, Müller PK, Bechstein WO, Mack MG, Söllner O, Felix R (1996) Liver tumors: comparison of MR imaging with Gd-EOB-DTPA and Gd-DTPA. Radiology 200:59–67
Wells ML, Venkatesh SK, Chandan VS, Fidler JL, Fletcher JG, Johnson GB, Hough DM, Roberts LR (2015) Biphenotypic hepatic tumors: imaging findings and review of literature. Abdom Imaging 40:2293–2305
Fowler KJ, Sheybani A, Parker RA 3rd, Doherty S, Brunt ME, Chapman WC, Menias CO (2013) Combined hepatocellular and cholangiocarcinoma (biphenotypic) tumors: imaging features and diagnostic accuracy of contrast-enhanced CT and MRI. AJR Am J Roentgenol 201:332–339
Potretzke TA, Tan BR, Doyle MB, Brunt EM, Heiken JP, Fowler KJ (2016) Imaging features of biphenotypic primary liver carcinoma (hepatocholangiocarcinoma) and the potential to mimic hepatocellular carcinoma: LI-RADS analysis of CT and MRI features in 81 cases. AJR Am J Roentgenol 207:25–31
International Agency for Research on Cancer (2013) GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon. Available via http://globocan.iarc.fr. Accessed 6 Aug 2017
Korean Society of Abdominal Radiology (2017) Diagnosis of hepatocellular carcinoma with gadoxetic acid-enhanced MRI: 2016 consensus recommendations of the Korean Society of Abdominal Radiology. Korean J Radiol 18:427–443
Choi SH, Byun JH, Lim YS, Yu E, Lee SJ, Kim SY, Won HJ, Shin YM, Kim PN (2016) Diagnostic criteria for hepatocellular carcinoma 3 cm with hepatocyte-specific contrast-enhanced magnetic resonance imaging. J Hepatol 64:1099–1107
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Myeong-Jin Kim.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Ha Yan Kim, M.S. in statistics, kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Rights and permissions
About this article
Cite this article
Kim, YY., An, C., Kim, S. et al. Diagnostic accuracy of prospective application of the Liver Imaging Reporting and Data System (LI-RADS) in gadoxetate-enhanced MRI. Eur Radiol 28, 2038–2046 (2018). https://doi.org/10.1007/s00330-017-5188-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5188-y