Abstract
Objectives
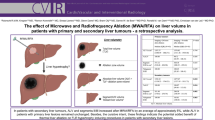
To assess the significance of fat in the radiofrequency ablation (RFA) zone of hepatocellular adenomas (HCA), and its association with tumoral fat and hepatic steatosis.
Methods
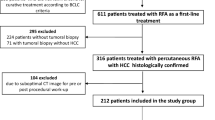
The radiological archive was searched for patients with ablated HCAs and follow-up magnetic resonance imaging between January 2008 and June 2014. Age, sex, risk factors and duration of clinical and imaging follow-up were recorded. Pre-RFA imaging was assessed for tumour size, intra-tumoral fat and steatosis. Post-RFA imaging was reviewed for size, enhancement and intra-ablational fat. Intra-ablational fat was classified as peripheral, central or mixed; the association of these distributions with steatosis and tumoral fat was assessed using Fisher’s exact test.
Results
Sixteen patients with 26 ablated HCAs were included. Fat was present in 23/26 (88 %) ablation zones. Only 1/26 (4 %) showed serial enlargement and enhancement suggestive of residual disease; the enhancing area did not contain fat. All remaining ablations showed involution and/or diminishing fat content without suspicious enhancement (mean follow-up, 27 months; range, 2–84 months). The peripheral and mixed/central patterns of intra-ablational fat were associated with steatosis (P = 0.0005) and tumoral fat (P = 0.0003), respectively.
Conclusion
Fat in the ablation zone of HCAs is a common finding which, in isolation, does not indicate residual tumour.
Key Points
• Fat in the RFA zone of HCAs is a common finding on MRI.
• The distribution of fat is associated with hepatic steatosis and intra-tumoral fat.
• In isolation, intra-ablational fat of treated HCAs does not indicate residual tumour.





Similar content being viewed by others
References
Atwell TD, Brandhagen DJ, Charboneau JW, Nagorney DM, Callstrom MR, Farrell MA (2005) Successful treatment of hepatocellular adenoma with percutaneous radiofrequency ablation. AJR Am J Roentgenol 184:828–831
Stoot JH, Coelen RJ, De Jong MC, Dejong CH (2010) Malignant transformation of hepatocellular adenomas into hepatocellular carcinomas: a systematic review including more than 1600 adenoma cases. HPB (Oxford) 12:509–522
Katabathina VS, Menias CO, Shanbhogue AK, Jagirdar J, Paspulati RM, Prasad SR (2011) Genetics and imaging of hepatocellular adenomas: 2011 update. Radiographics 31:1529–1543
Agrawal S, Agarwal S, Arnason T, Saini S, Belghiti J (2015) Management of hepatocellular adenoma: recent advances. Clin Gastroenterol Hepatol 13:1221–1230
Marrero JA, Ahn J, Rajender Reddy K, American College of Gastroenterology (2014) ACG clinical guideline: the diagnosis and management of focal liver lesions. Am J Gastroenterol 109:1328–1347, quiz 1348
Fujita S, Kushihata F, Herrmann GE et al (2006) Combined hepatic resection and radiofrequency ablation for multiple hepatic adenomas. J Gastroenterol Hepatol 21:1351–1354
Rhim H, Lim HK, Kim YS, Choi D (2008) Percutaneous radiofrequency ablation of hepatocellular adenoma: initial experience in 10 patients. J Gastroenterol Hepatol 23:e422–e427
Rocourt DV, Shiels WE, Hammond S, Besner GE (2006) Contemporary management of benign hepatic adenoma using percutaneous radiofrequency ablation. J Pediatr Surg 41:1149–1152
van Vledder MG, van Aalten SM, Terkivatan T, de Man RA, Leertouwer T, Ijzermans JN (2011) Safety and efficacy of radiofrequency ablation for hepatocellular adenoma. J Vasc Interv Radiol 22:787–793
van der Sluis FJ, Bosch JL, Terkivatan T, de Man RA, Ijzermans JN, Hunink MG (2009) Hepatocellular adenoma: cost-effectiveness of different treatment strategies. Radiology 252:737–746
van Aalten SM, Terkivatan T, van der Linden E, Verheij J, de Man RA, Ijzermans JN (2011) Management of liver adenomatosis by radiofrequency ablation. Dig Surg 28:173–177
Kim YS, Rhim H, Lim HK, Choi D, Lee MW, Park MJ (2011) Coagulation necrosis induced by radiofrequency ablation in the liver: histopathologic and radiologic review of usual to extremely rare changes. Radiographics 31:377–390
Pupulim LF, Hakime A, Barrau V, Abdel-Rehim M, Zappa M, Vilgrain V (2009) Fatty hepatocellular carcinoma: radiofrequency ablation–imaging findings. Radiology 250:940–948
Prasad SR, Wang H, Rosas H et al (2005) Fat-containing lesions of the liver: radiologic-pathologic correlation. Radiographics 25:321–331
Ahmed M, Solbiati L, Brace CL et al (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria–a 10-year update. Radiology 273:241–260
Lee SW, Park SH, Kim KW et al (2007) Unenhanced CT for assessment of macrovesicular hepatic steatosis in living liver donors: comparison of visual grading with liver attenuation index. Radiology 244:479–485
Bahl M, Qayyum A, Westphalen AC et al (2008) Liver steatosis: investigation of opposed-phase T1-weighted liver MR signal intensity loss and visceral fat measurement as biomarkers. Radiology 249:160–166
Mennesson N, Dumortier J, Hervieu V et al (2009) Liver steatosis quantification using magnetic resonance imaging: a prospective comparative study with liver biopsy. J Comput Assist Tomogr 33:672–677
van Werven JR, Marsman HA, Nederveen AJ et al (2010) Assessment of hepatic steatosis in patients undergoing liver resection: comparison of US, CT, T1-weighted dual-echo MR imaging, and point-resolved 1H MR spectroscopy. Radiology 256:159–168
Reeder SB, Sirlin CB (2010) Quantification of liver fat with magnetic resonance imaging. Magn Reson Imaging Clin N Am 18:337–357, ix
Kodama Y, Ng CS, Wu TT et al (2007) Comparison of CT methods for determining the fat content of the liver. AJR Am J Roentgenol 188:1307–1312
Furlan A, van der Windt DJ, Nalesnik MA et al (2008) Multiple hepatic adenomas associated with liver steatosis at CT and MRI: a case-control study. AJR Am J Roentgenol 191:1430–1435
Acknowledgments
The scientific guarantor of this publication is Dr. Mostafa Atri. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. Mr. Mohamed Abdolell, B.Sc. M.Sc. P.Stat. kindly provided statistical advice for this manuscript. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. Methodology: retrospective, cross sectional study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
Boxplot comparing qualitative and semi-quantitative assessments of steatosis. The calculated MR signal fat fraction is plotted according to the subjective grade of steatosis assigned (none/mild, moderate and severe). The mean fat fraction and standard deviation for each group are denoted by the dashed horizontal line and error bars, respectively (JPG 12 kb)
Rights and permissions
About this article
Cite this article
Costa, A.F., Kajal, D., Pereira, A. et al. Should fat in the radiofrequency ablation zone of hepatocellular adenomas raise suspicion for residual tumour?. Eur Radiol 27, 1704–1712 (2017). https://doi.org/10.1007/s00330-016-4496-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4496-y