Abstract
Objective
To prove that magnetic resonance imaging of foetal anatomy during the active second stage of vaginal delivery is feasible.
Materials and methods
Initially, five pregnant volunteers around the 30th week of gestation were examined in an open MRI. Based on the findings, one vaginal delivery was acquired under real-time imaging. To monitor the birth status during image acquisition, an MR-compatible wireless cardiotocography (CTG) system was built. Single-shot sequence parameters were optimised to compensate motion artefacts during labour.
Results
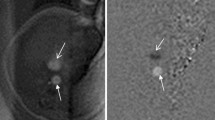
Safety requirements to monitor the birth process under real-time MR imaging were met. High-resolution MR images were acquired immediately before and after delivery. In one patient, TSE single-shot cinematic sequences of the active second stage of labour were obtained. All sequences were adapted to tolerate movement of the mother and infant, as well as residual noise from the CTG. Furthermore, the MR imaging during labour showed only minor image artefacts.
Conclusion
CTG-monitored acquisition of MRI series during the active second stage of delivery is feasible. Image quality should allow various further studies to improve models for birth simulation as well as potential investigation of obstructed labour and obstetric complications.
Key Points
• The active second stage of obstetric delivery can be followed by MRI.
• Wireless cardiotocography allows monitoring of the foetus during MRI.
• It has potential applications in evaluation of late obstetric problems.




Similar content being viewed by others
Abbreviations
- MRI:
-
Magnetic resonance imaging
- bSSFP:
-
Balanced steady-state free precession
- CTG:
-
Cardiotocography
- DAQ:
-
Data acquisition
- FFE:
-
Fast field echo
- FHR:
-
Foetal heart rate
- FM:
-
Foetal monitor
- GUI:
-
Graphical user interface
- GRE:
-
Gradient echo
- toco:
-
Tocodynamometer
- TSE:
-
Turbo spin echo
- US:
-
Ultrasound
References
Gei A, Oto A, Pacheco L, Cassady C (2009) P232 Serial evaluation of maternal descent and fetal head dimensions using MRI during labor: Report of the first case. International Journal of Gynecology & Obstetrics 107:S477–S478
Li X, Kruger JA, Nash MP, Nielsen PMF (2010) Modeling childbirth: elucidating the mechanisms of labor. Wiley Interdisciplinary Reviews: Systems Biology and Medicine 2:460–470
Lien KC, Mooney B, DeLancey JOL, Ashton-Miller JA (2004) Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol 103:31
Kölbl H (2001) Pregnancy, childbirth and the pelvic floor. Zentralbl Gynakol 123:666–671
Preyer O, Hanzal E, Umek W, Laml T (2006) The impact of pregnancy and childbirth on the pelvic floor. Geburtsh Frauenheilk 66:450–454
MacArthur C, Bick DE, Keighley MRB (1997) Faecal incontinence after childbirth. BJOG: An International Journal of Obstetrics & Gynaecology 104:46–50
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI (1993) Anal-sphincter disruption during vaginal delivery. N Engl J Med 329:1905–1911
Peschers UM, Sultan AH, Jundt K, Mayer A, Drinovac V, Dimpfl T (2003) Urinary and anal incontinence after vacuum delivery. Eur J Obstet Gynecol Reprod Biol 110:39–42
Kok RD, de Vries MM, Heerschap A, van den Berg PP (2004) Absence of harmful effects of magnetic resonance exposure at 1.5 T in utero during the third trimester of pregnancy: a follow-up study. Magn Reson Imaging 22:851–854
Myers C, Duncan KR, Gowland PA, Johnson IR, Baker PN (1998) Failure to detect intrauterine growth restriction following in utero exposure to MRI. Br J Radiol 71:549–551
Poutamo J, Partanen K, Vanninen R, Vainio P, Kirkinen P (1998) MRI does not change fetal cardiotocographic parameters. Prenat Diagn 18:1149–1154
Schiffer IB, Schreiber WG, Graf R et al (2003) No influence of magnetic fields on cell cycle progression using conditions relevant for patients during MRI. Bioelectromagnetics 24:241–250
Rodegerdts EA, Grönewäller EF, Kehlbach R et al (2000) In vitro evaluation of teratogenic effects by time varying MR gradient fields on fetal human fibroblasts. J Magn Reson Imaging 12:150–156
Schwenzer NF, Bantleon R, Maurer B et al (2007) In vitro evaluation of magnetic resonance imaging at 3.0 tesla on clonogenic ability, proliferation, and cell cycle in human embryonic lung fibroblasts. Investig Radiol 42:212
Schneider KT, Butterwegge M, Daumer M et al (2006) Use of CTG during pregnancy and childbirth. Z Geburtshilfe Neonatol 210:38–49
(1994) Antepartum fetal surveillance. ACOG Technical Bulletin Number 188—January 1994. Int J Gynaecol Obstet 44:289–294
Schaefers G, Melzer A (2006) Testing methods for MR safety and compatibility of medical devices. Minim Invasive Ther Allied Technol 15:71–75
ASTM Standard F2119–07 (2007) Standard test method for evaluation of MR image artifacts from passive implants. ASTM International
Guettler FV, Heinrich A, Teichgraeber U (2011) Open source MR-susceptibility artifact measurement (SAM). ESMRMB, Leipzig
ASTM Standard F2052-06E1 (2006) Standard Test Method for Measurement of Magnetically Induced Displacement Force on Medical Devices in the Magnetic Resonance Environment. ASTM International
National Electrical Manufacturers Association (NEMA) (2008) NEMA Standards Publication MS 1–2008 Determination of Signal-to-Noise Ratio (SNR) in Diagnostic Magnetic Resonance Imaging. National Electrical Manufacturers Association
ASTM Standard F2503-08 (2008) Standard Practice for Marking Medical Devices and Other Items for Safety in the Magnetic Resonance Environment. ASTM International
Shellock FG, Woods TO, Crues JV (2009) MR labeling information for implants and devices: explanation of terminology. Radiology 253:26
Rinck PA (2001) Magnetic resonance in medicine: the basic textbook of the European magnetic resonance forum. Wiley-Blackwell, Berlin
Bodner-Adler B, Bodner K, Joura E et al (2001) Influence of different maternal birth positions on perineal trauma and neonatal parameters during spontaneous vaginal delivery. Geburtshilfe und Frauenheilkunde 61:766–770
Bodner-Adler B, Bodner K, Kimberger O, Lozanov P, Husslein P, Mayerhofer K (2003) Women's position during labour: influence on maternal and neonatal outcome. Wien Klin Wochenschr 115:720–723
Levine D, Barnes PD, Sher S et al (1998) Fetal fast MR imaging: reproducibility, technical quality, and conspicuity of anatomy. Radiology 206:549–554
Levine D, Hatabu H, Gaa J, Atkinson MW, Edelman RR (1996) Fetal anatomy revealed with fast MR sequences. AJR Am J Roentgenol 167:905–908
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Güttler, F.V., Heinrich, A., Rump, J. et al. Magnetic resonance imaging of the active second stage of labour: Proof of principle. Eur Radiol 22, 2020–2026 (2012). https://doi.org/10.1007/s00330-012-2455-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2455-9