Abstract
In carpal tunnel syndrome (CTS), manual therapy interventions (MTI) reduce tissue adhesion and increase wrist mobility. We evaluated the efficacy of a MTI in relieving CTS signs and symptoms. Twenty-two CTS patients (pts) (41 hands) were treated with a MTI, consisting in 6 treatments (2/week for 3 weeks) of soft tissues of wrist and hands and of carpal bones. Pts were assessed for hand sensitivity, paresthesia, hand strength, hand and forearm pain, night awakening; Phalen test, thenar eminence hypotrophy and Boston Carpal Tunnel Questionnaire (BCTQ) Symptom Severity Scale (SSS) and Functional Status Scale (FSS). Median nerve was studied by sensory nerve conduction velocity (SNCV) and distal motor latency (DML). CTS was scored as minimal, mild, medium, severe and extreme. We considered as control group the same pts assessed before treatment: at baseline (T0a) and after 12 weeks (T0b). Pts were evaluated at the end of treatment (T1) and after 24-week (T2) follow-up. At T0b, versus T0a, forearm pain and Phalen test positivity were increased and hand strength reduced (p < 0.05). BCTQ–SSS and BCTQ–FSS scores improved at T1 versus T0b (p < 0.05) with the amelioration maintained at T2. At T1, the number of pts with paresthesia, night awakening, hypoesthesia, Phalen test, hand strength reduction and hand sensitivity was reduced with the lacking of symptoms maintained at T2 (p < 0.05). No changes in SNCV, DML and CTS scoring were shown. MTI improved CTS signs and symptoms, with benefits maintained at follow-up. Thus, it may be valid as a conservative therapy.
Similar content being viewed by others
Introduction
Carpal tunnel syndrome (CTS) is caused by entrapment and compression of the median nerve at wrist, within the carpal tunnel, positioned between the transverse carpal ligament and the carpal bones, and causes sensory (paraesthesias and hypoesthesias) and motor impairment and pain, especially at night, in the area of the hand innervated by the median nerve.
Carpal tunnel syndrome is the most common nerve compression syndrome, with a prevalence rate of 50 cases per 100 subjects in the general population [1], 9.2 % in women and 6 % in men [2, 3], and an incidence rate of up to 276:100.000/year [4]. It may lead to work disability and, thus, to waning productivity [5–7] and is associated with high-cost treatment [8].
Although most cases are idiopathic [9], CTS may be associated with systemic conditions, including rheumatoid or psoriatic arthritis (causing thickening of the articular and peri-tendineal synovium) hypothyroidism, diabetes mellitus, acromegaly, gout and pregnancy [10] that, reducing the size of the carpal tunnel or increasing the volume of its content, could cause compression of the median nerve. CTS may also be caused by local trauma and by overuse and prolonged improper positioning of the hand or wrist, mainly due to occupational causes, such as continuous use of the mouse and highly repetitive or forceful works involving hand and causing wrist vibration [11].
Surgical treatment, performed to reduce the pressure on the median nerve by the complete division of the flexor retinaculum, may be executed with standard open modality, with endoscopic modality or as minimal incision of carpal tunnel. The efficacy of surgical approaches, regardless of the technique, is supported by high-quality evidence [12].
The guidelines of American Academy of Orthopedic Surgeons (AAOS) for the treatment of CTS [12, 13] recommend both conservative and surgical treatments for early CTS without denervation of the median nerve, although they also advise an initial course of conservative treatment. Surgery can be considered in case of nerve denervation or if the patient prefers surgery [12].
A study comparing surgical management of CTS with nonsurgical treatments (including hand therapy and ultrasound) showed that group treated with surgery achieved modestly better outcomes in hand function and symptoms at both 3 and 12 months in respect of the control group [14]. A Cochrane review concluded that surgical treatment is more effective on CTS than splinting, which is the mainstay of conservative treatment, but the evidence for surgical treatment being superior to steroid injections is unclear [15]. Thus, criteria are needed to recognize the best treatment for CTS patients with mild to moderate symptoms and to identify patients who should be treated initially with conservative or surgical treatment.
Apart from splinting, the options for CTS conservative treatment include local injection of corticosteroids, systemic treatment with corticosteroids, ultrasound, electrotherapy, vitamin B6, vitamin B12 or nonsteroidal anti-inflammatory drugs (NSAIDs) [16].
A single-blind study comparing in 91 patients with CTS a 9-week treatment with NSAIDs, plus nocturnal wrist supports versus a chiropractic treatment (manipulation of the soft tissues and joints of the upper extremities and spine) added to ultrasound over the carpal tunnel and nocturnal wrist supports, shows improvement in perceived comfort and function, nerve conduction and sensation at finger level, with no significant differences between groups in the efficacy of either treatment both at the end of treatment and at a 1-month follow-up [17].
Chiropractic or osteopathic manual interventions (soft tissue treatment and carpal bone mobilization), by alleviating the mechanical compression of the median nerve, may provide some relief of symptoms in patients experiencing CTS [18–20].
A study on cadavers shows that osteopathic manipulation is able to elongate carpal tunnel ligament and suggests how these techniques may be of use in nonsurgical relief of pressure on the median nerve in patients with CTS [21].
Magnetic resonance imaging demonstrates that the antero-posterior and transverse dimensions of the carpal tunnel significantly increased after a course of myofascial release manipulation and self-stretching in a small group of patients affected with CTS, while symptoms and nerve conductions improved [22].
Also median nerve mobilization, potentially reducing the pressure existing within the nerve and improving the blood flow to the nerve, thus favoring its regeneration and healing [23], is useful in improving CTS symptoms [24].
However, the generalization of the findings of the studies conducted in this field is limited by methodological problems, such as the small number of the patients enrolled (some reports consisting in anectodical cases or patients series), the reliability and accuracy of the palpation methods, the technique to assess range of movements, and the lack of a statistical analysis, and high-quality trials assessing the effectiveness and safety of mobilization techniques are needed [25].
Given the results provided on CTS symptoms by manual methods, here we propose a rehabilitation technique based on a manual therapy intervention on wrist and hands soft tissues and on carpal bones, in order to evaluate its efficacy on self-referred symptoms, signs, hand functionality and nerve conduction studies (ElectroNeuroGraphy, ENG) in patients affected with CTS.
Patients and methods
Twenty-two Caucasian patients (19 patients with bilateral disease and 3 with unilateral symptoms (20 women, 2 men); age and symptoms duration, 65.50 ± 8.12 years and 12.0 ± 2.1 months, respectively) with clinic and electrophysiological evidence of CTS were enrolled from the outpatient clinic of the Department of Biomedicine, Division of Rheumatology, University of Florence, and agreed by a written informed consent to participate in the study, approved by our institutional ethics committee. The research reported was undertaken in compliance with the Helsinki Declaration.
Exclusion criteria were as follows: previous carpal tunnel surgery, history suggesting underlying causes of CTS (diabetes mellitus, pregnancy, thyroid disease and acromegaly) and history of other musculoskeletal conditions (osteoarthritis, rheumatoid and psoriatic arthritis, gout and fibromyalgia syndrome).
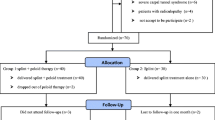
After baseline assessment (T0a), 9 patients (7 affected by bilateral disease and 2 with unilateral disease, all women) were evaluated after 12 weeks (T0b) in order to monitor the natural history of the symptoms before beginning the treatment.
Then, all the enrolled patients were treated for 3 weeks with manual manipulation (2 sessions/week, 10–15 min each), for a total of 6 treatments, all performed by the same operator (MS). Patients were, then, assessed at the end of the treatment (T1) and after a 24-week follow-up. Thus, the study had the total duration of 39 weeks.
The patients were asked to refrain from using wrist splints and from starting any new pharmacological intervention for CTS.
Assessment schedule
All the patients were evaluated at enrollment (T0a), at the end of the treatment (T1) and after a follow-up of 24 weeks (T2) by a detailed clinical workup including anamnesis and physical examination; they were administered with the Boston Carpal Tunnel Questionnaire (BCTQ); nerve conduction studies and ENG findings (graded according to Padua et al. [26]) were executed. A group of 9 patients was also assessed after 12 weeks before beginning manipulations (T0b).
The operator who executed clinical workup and administered Boston Carpal Tunnel Questionnaire (MB) was blinded to the findings of Nerve Conduction Studies, and the operator who performed ENG (GDS) was blinded to clinical data.
Clinical workup
All patients underwent a clinical workup assessing the grade of functional and sensitive impairment by clinical history and physical examination. The first focused on symptom onset, hand sensitivity, hypoesthesia, paresthesia, hand strength reduction, pain localization and irradiation (at forearm), and night awakening. At physical examination, Phalen test, sensitivity examination and the presence of hypotrophy or atrophy of the thenar eminence were assessed.
Boston Carpal Tunnel Questionnaire
Every patient filled in the Italian version of Boston Carpal Tunnel Questionnaire (BCTQ), a self-administered tool, assessing the severity of symptoms and the functional status in CTS [27]. BCTQ has good validity, reliability and responsiveness [28], and it is composed of 2 scales, the Symptom Severity Scale (SSS) and the Functional Status Scale (FSS), containing 11 and 8 items, respectively. Each item is rated on a 5-point rating scale.
Nerve conduction studies (ENG)
The neurophysiological studies were carried out using a Synergy EMG Viasys-Care Fusion; an infrared lamp was used to maintain hand skin temperature >31 °C during all the tests.
In our study, the following standard tests were used:
-
median sensory nerve conduction velocity (SNCV) from the third digit to wrist;
-
median distal motor latency (DML) from wrist to thenar eminence (abductor brevis pollicis);
-
ulnar SNVC from fifth digit to wrist;
Normal values are the following: median SNCV from the third digit to wrist >50 m/s, ulnar SNVC from digit to wrist >50, median DML <4 ms.
CTS was scored on the basis of the neurophysiological classification of Padua et al. [26] into 6 classes of severity on the basis of median nerve electrodiagnostic findings:
-
Extreme CTS (EXT): absence of thenar motor and sensory response;
-
Severe CTS (SEV): absence of median sensory response (digit-wrist segment) and abnormal DML;
-
Moderate CTS (MOD): slowing of digit-wrist conduction and abnormal DML;
-
Mild CTS (MILD): slowing of median digit-wrist conduction and normal DML;
-
Minimal CTS (MIN): standard negative hands with abnormal comparative or segmental (<7–8 cm) tests;
-
Negative CTS (NEG): normal findings at all tests (including comparative or segmental tests).
Educational program
Before beginning the treatment, all the patients were educated by a specific educational program (2 weekly sessions of 45 min each) providing them with information about CTS and about a correct behavior to not overload upper limbs, especially hands and wrists, by performing incorrect movements in daily and working activities, potentially invalidating the effects obtained by the intervention.
Manual therapy intervention
In the first session (duration, 10 min), the most thickened tissues of hand palmar surface and wrist and forearm volar side were treated by deep transverse massage (cyriax), in order to improve tissue elasticity by detachment maneuvers performed in the cranio-caudal direction (Fig. 1a).
Manual therapy intervention on CTS. a Deep transverse massage (cyriax) of hand palmar surface and wrist and forearm volar side performed by detachment maneuvers executed in the cranio-caudal direction. b Passive mobilizations of the radio-carpal and radio-ulnar joints, and opening of the palmar surface of metacarpal-phalangeal joints, executed with the hand maintained in traction. c Treatment of the wrist, maintained in traction, with passive flexo-extension and transversal movements. d Treatment of the palmar aponeurosis and of the pollical and the first palmar interosseous with the hand maintained open and extended
In the second and third sessions (duration, 15 min), performed with the hand maintained in traction, passive mobilizations of the radio-carpal and radio-ulnar joints, and opening of the palmar surface of metacarpal–phalangeal joints were added (Fig. 1b).
In the following (4th to 6th) sessions (duration, 15 min), a further joint mobilization of the wrist was added to the treatments executed in the previous sessions. The wrist, maintained in traction, was treated with passive flexo-extension and transversal movements in order to improve the range of movement of the joints and the elasticity of flexo-extensor and prono-supinator muscles (Fig. 1c). Also, the palmar aponeurosis and the pollical and the first palmar interosseous muscles were treated, working on the hand that was maintained open and extended (Fig. 1d).
Safety, compliance and satisfaction with the treatment
Safety was evaluated by registering adverse effects not leading and leading to the stop of the treatment (dropouts), and compliance was assessed basing on the number of sessions attended for subject and on the number of patients lost at follow-up.
Participants were asked, at the end of the treatment period, to answer to a question about their overall level of satisfaction for the treatment on the basis of a Visual Analogue Scale (VAS) 0–10, with 0 = no satisfaction and 10 = the highest level of satisfaction.
Statistical analysis
Data are presented as mean ± standard deviation and as number and percentages. Student’s t test for paired data was used to evaluate differences in groups at T0a and T0b. ANOVA for repeated measures, with Bonferroni test for the post hoc analysis, and Fisher’s exact tests, when appropriated, were used to detect effects of treatment at T0a, T1 and T2.
p value was considered significant for values <0.05. Data analysis was performed by using the SPSS statistical package for Windows.
Results
Boston Carpal Tunnel Questionnaire before manual therapy intervention (T0b vs T0a)
Both Symptom Severity Scale (SSS) and Functional Status Scale (FSS) of Boston Carpal Tunnel Questionnaire were unchanged at T0b in respect of T0a (p = NS for all the comparisons at T0b vs T0a) (Table 1).
Hand symptoms before manual therapy intervention (T0b vs T0a)
The prevalence of the symptoms assessed at T0b (evaluated for each hand) was unchanged in respect of T0a for all the items, with the exception of Phalen test, whose positivity resulted significantly higher at T0b in respect of T0a (p = 0.0041) (Table 2).
ENG before manual therapy intervention (T0b vs T0a)
At T0b, in respect of T0a, both SNCV and DML of median nerve were unchanged (p = NS in both cases) (Table 1).
Effects of manual therapy intervention on Boston Carpal Tunnel Questionnaire scores
Boston Carpal Tunnel Questionnaire–Symptom Severity Scale
At the end of the treatment (T1), BCTQ–SSS was improved significantly, as demonstrated by the score reduction at T1 in respect of T0a (p < 0.05).
At follow-up evaluation (T2), the improvement obtained in BCTQ–SSS by manual manipulation was maintained in respect of T0a (p < 0.05) and remained stable in respect of T1 (p = NS) (Table 3).
Boston Carpal Tunnel Questionnaire–Functional Status Scale
At T1, the BCTQ–FSS score was improved significantly at T1 versus T0a (p < 0.05).
At T2, the improvement obtained in the BCTQ–FSS score in respect of T0a was maintained (p < 0.05) and remained stable in respect of T1 (p = NS) (Table 3).
Effects of manual therapy intervention on CTS-related symptoms
At T1, in respect of T0a, the number of patients reporting the presence of paresthesia (p < 0.0001) pain (p = 0.0132), night awakening (p = 0.0002) and hand sensitivity (p = 0.0006) was reduced significantly in respect of T0. Hypoesthesia was reduced at the limits of significance (p = 0.0531).
The number of patients reporting the other symptoms did not change significantly (Table 4).
Effects of manual therapy intervention on ENG
In STC patients, manual treatment of hand did not ameliorate NCS values.
SNCV values, as well as DML, did not change significantly at T1 versus T0a and remained unchanged also at follow-up evaluation (T2) in respect of T1 and T0 (Table 3).
Safety, compliance and satisfaction with the manual therapy intervention
None of the patients dropped out from the study, and no side effect was observed in patients after the application of manual therapy intervention.
The compliance was high, as all patients participated in all the sessions and no patient was lost at follow-up.
The overall satisfaction from the treatment, explored by a VAS based question, was high (9.4 ± 1.3).
Discussion
In this study, the effect of a manual therapy intervention on CTS symptoms and hand function was evaluated. Patients improved significantly in hand symptoms and function, as assessed by BCTQ and by the reductions in the prevalence of paresthesias, hand pain and sensitivity, and night awakening. The improvements obtained by the intervention were maintained at the follow-up. The treatment did not improve Nerve Conduction Studies nor change neurophysiological grading of CTS.
In the subjects assessed also after 12 weeks in respect of baseline, before beginning manipulations, the prevalence of Phalen test positivity increased, but no other modification in symptoms, BCTQ scores and Nerve Conduction Studies was shown.
Our study shows that the manual therapy intervention used in our study, as safe and efficacious, could be taken into account as an alternative treatment to surgical release of the carpal tunnel, which, although regarded as the definitive treatment for CTS, more than as a first-line therapy, generally is used after the failure of conservative treatments or in patients with moderate to severe symptom [12, 13].
As underlined by AAOS guidelines, the complete division of the flexor retinaculum executed with open surgery and endoscopic surgery as well as with minimal incision of carpal tunnel is effective for treating CTS [12, 13].
Comparing open and endoscopic release of carpal tunnel, the latter was favored in residual pain at 12 weeks postoperatively, return to work time and wound-related complications. Open release was favored when reversible nerve damage was the outcome measure. No difference in the techniques was shown in symptom severity or functional status at 52 weeks, complications and infections [29–31].
Minimal incision, when compared to open release, was favored in symptom severity, functional status and scar tenderness. When compared to endoscopic release, it was favored when pain at 2 or 4 weeks was the outcome measure [29–31].
According to AAOS guidelines, in carpal tunnel release, skin nerve preservation and epineurotomy should not be routinely used, while the evidences for flexor retinaculum lengthening, internal neurolysis, tenosynovectomy and ulnar bursa preservation are inconclusive [12, 13].
Although effective, complications in carpal tunnel surgical release may occur in 1–2 % [10]. The failure rate ranges from 15 to 20 % [32], and patients who failed primary surgical interventions (up to 12 %) may require a secondary surgery [33, 34]. Persistent symptoms after a secondary surgery range from 25 to 95 % [35].
Conservative management is a first-step treatment, to be preferred for early and supposedly transient cases of CTS, such as those associated with pregnancy or short-term overuse. In other cases, it might be used for reducing symptoms while awaiting surgery [36]. The substantial proportion of patients obtaining no or incomplete relief by conservative management needs surgical intervention.
It should be underlined that in CTS associated with endocrine conditions, such as hypothyroidism, diabetes mellitus, acromegaly or rheumatic affections, such as rheumatoid or psoriatic arthritis and gout, CTS management should be associated with the treatment for the underlying disease [10].
The few randomized clinical trials comparing surgical interventions to conservative medical management indicate that, generally, symptom severity and functional status improve more with surgery than with nonoperative therapy [37, 38], although a randomized trial showed that CTS patients treated with surgery achieved only modestly better outcomes in hand function and symptoms in respect of the control group treated with nonsurgical therapy [14].
However, despite the positive clinical outcomes of surgical interventions, it is recommended to try conservative management of CTS before surgery [13, 39].
A Cochrane review about nonsurgical treatment for CTS shows significant short-term benefit from carpal bone mobilization, oral steroids, splinting, ultrasound and yoga, while other nonsurgical treatments do not produce significant benefit [40].
In the previous studies, different manual interventions (based on soft tissue, carpal bone and median nerve treatment and mobilization) were shown to reduce symptoms in patients experiencing CTS [17–20, 22–24].
In an open trial conducted on a small cohort of patients affected with CTS, soft tissue mobilization (administered 3 times a week for 2 weeks) improved symptoms, assessed by Boston Carpal Tunnel Questionnaire, but not ENG [41].
However, these studies are limited by different methodological biases, such as the small number of patients, the reliability and accuracy of the palpation methods, the tool to assess range of movements and the lack of statistics.
A recent Cochrane review states that mobilization interventions in CTS have a low-quality evidence and that high-quality randomized controlled trials assessing their efficacy are needed [24].
A study compared, in 2 groups of patients with CTS, instrument–assisted soft tissue mobilization and manual soft tissue mobilization, both supplemented with stretching and strengthening home exercises. The results showed improvements in nerve conduction latencies, strength and motion of the wrist, subjective evaluations and patient satisfaction in both groups, all maintained at a 3-month follow-up: however, no difference between groups was shown [42].
In our study, manual therapy intervention is of great efficacy in relieving CTS-related symptoms, such as paresthesia, pain, night awakening and hand sensitivity, and in reducing the scores of Symptom Severity Scale and Functional Status Scale of Boston Carpal Tunnel Questionnaire, a validated measure, also suggested by guidelines [13], for the self-assessment of symptoms in patients affected with CTS.
The treatment was also safe and satisfactory for the patients, given the lack of any adverse effects and dropout and the high levels of overall satisfaction reported at the end of the intervention by the patients.
The increased prevalence of Phalen test positivity in the group of subjects assessed also after 12 weeks in respect of baseline before beginning treatment shows that the symptoms in our patients were worsening and indicates that the further improvement obtained after treatment both on symptoms and on Boston Carpal Tunnel Questionnaire cannot be related to a spontaneous amelioration of disease course.
However, according to our data, the manual therapy intervention used in the study, although efficacious in relieving symptoms, failed in improving neurophysiological parameters. The results are not unexpected and, potentially, may be related also to the brief treatment period and to the lacking of a home-based program of exercises, useful in implementing and in maintaining the effects of manual interventions [42].
However, abnormal sensory nerve conduction velocity and distal motor latencies of the median nerve do not generally improve with the use of nonsurgical interventions, as already shown for other different conservative treatments [43, 44].
It is to underline that also the studies assessing the effects of manual therapies on CTS provide only scant and not definitive data about their effects on ENG. In fact, nerve conduction studies were assessed in not all the studies performed and, in the majority of them, statistical evaluation was not calculated due to the small number of patients enrolled. Moreover, due to the difference in the manual therapy used and in their time of administration, no definitive conclusion may be drawn on the efficacy of these interventions on neurophysiological recording [17–20, 22, 41, 42].
For what concerns surgery, although retrospective studies reported postsurgical improvements in abnormal motor and sensory latencies of the median nerve, patients treated with surgery generally have slower latency values than patients nonsurgically treated and their values rarely return to normal values after intervention [45, 46]. Thus, the effects of various treatments on abnormal nerve conduction findings in CTS await further clarification from prospective research studies.
Our study has some limitations such as the limited number of patients, the lacking of a control group and the short period of follow-up.
Thus, controlled studies on a larger cohort of patients evaluated after a longer follow-up period are advocated to confirm our findings and to verify whether the technique could be of help in improving SNCS and DML in patients affected by CTS.
However, from our findings, manual therapy intervention emerges as a valid and efficacious nonsurgical treatment for CTS patient, by reducing symptoms (paresthesia, pain, night awakening, hypoesthesia and hand sensitivity) and improving hand function, thus resulting potentially useful in patients, also in those waiting for or not accepting surgery or in critical patients (with comorbidities and/or in polytherapy).
References
De Krom MC, Knipschild PG, Kester AD et al (1992) Carpal tunnel syndrome, prevalence in the general population. J Clin Epidemiol 45:373–376
Ashworth N (2010) Carpal tunnel syndrome. Available from: http://www.emedicine.com/pmr/topic21.htm. Accessed on 28 May 2010
Fuller D (2012) Carpal tunnel syndrome. Available from: http://www.emedicine.com/orthoped/topic455.htm. Accessed on 14 Jul 2012
Mondelli M, Giannini F, Giacchi M (2002) Carpal tunnel syndrome incidence in a general population. Neurology 58:289–294
Katz JN, Lew RA, Bessette L et al (1998) Prevalence and predictors of longterm work disability due to carpal tunnel syndrome. Am J Ind Med 33:543–550
Feuerstein M, Miller VL, Burrell LM, Berger R (1998) Occupational upper extremity disorders in the federal workforce. Prevalence, health care expenditures, and patterns of work disability. J Occup Environ Med 40:546–555
Latinovic R, Gulliford MC, Hughes RA (2006) Incidence of common compressive neuropathies in primary care. J Neurol Neurosurg Psychiatry 77:263–265
Hanrahan LP, Higgins D, Anderson H, Smith M (1993) Wisconsin occupational carpal tunnel syndrome surveillance: the incidence of surgically treated cases. Wis Med J 92:685–689
Marshall S (2001) Carpal tunnel syndrome. Clin Evid 5:717–728
Spinner RJ, Bachman JW, Amadio PC (1989) The many faces of carpal tunnel syndrome. Mayo Clin Proc 64:829–836
Tanaka S, Wild DK, Cameron LL, Freund E (1997) Association of occupational and non-occupational risk factors with the prevalence of self reported carpal tunnel syndrome in a national survey of the working population. Am J Ind Med 32:550–556
Keith MW, Masear V, Amadio PC et al (2009) Treatment of carpal tunnel syndrome. J Am Acad Orthop Surg 17:397–405
American Academy of Orthopaedic Surgeons Work Group Panel (2012) Clinical practice guideline on the treatment of carpal tunnel syndrome. Available at: www.aaos.org/research/guidelines/CTStreatmentguide.asp. Accessed on 14 Jul 2012
Jarvik JG, Comstock BA, Kliot M et al (2009) Surgery versus non-surgical therapy for carpal tunnel syndrome: a randomised parallel-group trial. Lancet 374:1074–1081
Verdugo RJ, Salinas RA, Castillo JL, Cea JG (2008) Surgical versus non-surgical treatment for carpal tunnel syndrome. Cochrane Database Syst Rev, Issue 4. Art. No.: CD001552
Harter BT Jr, McKiernan JE Jr, Kirzinger SS, Archer FW, Peters CK, Harter KC (1993) Carpal tunnel syndrome: surgical and non-surgical treatment. J Hand Surg 18A:734–739
Davis PT, Hulbert JR, Kassak KM, Meyer JJ (1998) Comparative efficacy of conservative medical and chiropractic treatment or carpal tunnel syndrome: a randomized clinical trial. J Manipulative Physiol Ther 21:317–326
Sucher BM (1994) Palpatory diagnosis and manipulative management of carpal tunnel syndrome. J Am Osteopath Assoc 94:647–663
Bonebrake AR (1994) A treatment for carpal tunnel syndrome: results of follow-up study. J Manipulative Physiol Ther 17:565–567
Valente R, Gibson H (1994) Chiropractic manipulation in carpal tunnel syndrome. J Manipulative Physiol Ther 17:246–249
Sucher BM, Hinrichs RN (1998) Manipulative treatment of carpal tunnel syndrome: biomechanical and osteopathic intervention to increase the length of the transverse carpal ligament. J Am Osteopath Assoc 98:679–686
Sucher BM (1993) Myofascial manipulative release of carpal tunnel syndrome: documentation with magnetic resonance imaging. J Am Osteopath Assoc 93:1273–1278
Butler D (1991) Mobilization of the nervous system, 1st edn. Churchill Livingstone, Melbourne
Tal-Akabi A, Rushton A (2000) An investigation to compare the effectiveness of carpal bone mobilisation and neurodynamic mobilisation as methods of treatment for carpal tunnel syndrome. Man Ther 5:214–222
Page MJ, O’Connor D, Pitt V, Massy-Westropp N (2012) Exercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database Syst Rev 6:CD009899
Padua L, Lo Monaco M, Padua R et al (1997) Neurophysiological classification of carpal tunnel syndrome: assessment of 600 symptomatic hands. Ital J Neurol Sci 18:145–150
Padua R, Padua L, Romanini E et al (1998) Versione italiana del Boston Carpal Tunnel Questionnaire. Giornale italiano di ortopedia e traumatologia 24:121–129
de Carvalho Leite JC, Jerosch-Herold C, Song F (2006) A systematic review of the psychometric properties of the Boston Carpal Tunnel Questionnaire. BMC Musculoskelet Disord 7:78
Scholten RJ, Gerritsen AA, Uitdehaag BM, van GD, de Vet HC, Bouter LM (2004) Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev CD003905
Thoma A, Veltri K, Haines T, Duku E (2004) A meta-analysis of randomized controlled trials comparing endoscopic and open carpal tunnel decompression. Plast Reconstr Surg 114:1137–1146
Shi Q, MacDermid JC (2011) Is surgical intervention more effective than non-surgical treatment for carpal tunnel syndrome? A systematic review. J Orthop Surg Res 11(6):17
Katz RT (1994) Carpal tunnel syndrome: a practical review. Am Fam Physician 49:1371–1379
Botte MJ, von Schroeder HP, Abrams RA, Gellman H (1996) Recurrent carpal tunnel syndrome. Hand Clin 12:731–743
Tung TH, Mackinnon SE (2001) Secondary carpal tunnel surgery. Plast Reconstr Surg 107:1830–1843 (quiz 1844,1933)
Steyers CM (2002) Recurrent carpal tunnel syndrome. Hand Clin 18:339–345
Ono S, Clapham PJ, Chung KC (2010) Optimal management of carpal tunnel syndrome. Int J Gen Med 30(3):255–261
Gerritsen AA, de Vet HC, Scholten RJ, Bertelsmann FW, de Krom MC, Bouter LM (2002) Splinting vs surgery in the treatment of carpal tunnel syndrome: a randomized controlled trial. JAMA 11(288):1245–1251
Katz JN, Keller RB, Simmons BP, Rogers WD, Bessette L, Fossel AH, Mooney NA (1998) Maine Carpal Tunnel Study: outcomes of operative and non operative therapy for carpal tunnel syndrome in a community-based cohort. J Hand Surg Am 23:697–710
Practice parameter for carpal tunnel syndrome (summary statement) (1993) Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurolog 43:2406–2409
O’Connor D, Marshall S, Massy-Westropp N (2003) Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev 1:CD003219
George JW, Tepe R, Busold D, Keuss S, Prather H, Skaggs CD (2006) The effects of active release technique on carpal tunnel patients: a pilot study. J Chiropr Med 5:119–122
Burke J, Buchberger DJ, Carey-Loghmani MT, Dougherty PE, Greco DS, Dishman JD (2007) A pilot study comparing two manual therapy interventions for carpal tunnel syndrome. J Manipulative Physiol Ther 30:50–61
Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR (1998) Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA 280:1601–1603
Manente G, Torrieri F, Di Blasio F, Staniscia T, Romano F, Uncini A (2001) An innovative hand brace for carpal tunnel syndrome: a randomized controlled trial. Muscle Nerve 24:1020–1025
Harter BT Jr, McKiernan JE Jr, Kirzinger SS, Archer FW, Peters CK, Harter KC (1993) Carpal tunnel syndrome: surgical and nonsurgical treatment. J Hand Surg Am 18:734–739
Finestone HM, Woodbury GM, Collavini T, Marchuk Y, Maryniak O (1996) Severe carpal tunnel syndrome: clinical and electrodiagnostic outcome of surgical and conservative treatment. Muscle Nerve 19:237–239
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maddali Bongi, S., Signorini, M., Bassetti, M. et al. A manual therapy intervention improves symptoms in patients with carpal tunnel syndrome: a pilot study. Rheumatol Int 33, 1233–1241 (2013). https://doi.org/10.1007/s00296-012-2507-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-012-2507-0