Abstract
The authors describe three anatomic variations, circumaortic, retroaortic left renal vein, and retropelvic tributary of the renal vein, in Japanese cadavers. The incidences and the clinical significances of these variations are discussed with a detailed review of the literature. The median incidences of circumaortic left renal vein (CLRV) were 7.0 % in cadavers examined and 1.8 % in clinical subjects examined. The detection of CLRV in CT/MDCT or angiography was relatively difficult compared with that by cadaver dissection. The median incidences of retroaortic left renal vein (RLRV) were 1.7 % in cadavers examined and 2.2 % in clinical subjects examined. The detection of RLRV was lower in operations, and relatively easy by ultrasonography. The incidence of retropelvic tributary of the renal vein ranged from 30.0 to 46.4 %, which is very frequent. Moreover, the incidences of communicating veins between the left renal vein and retroperitoneal veins ranged from 30.0 to 84.2 % in cadaver dissections and from 34.0 to 75.8 % in clinical reports.
Similar content being viewed by others
Introduction
The anatomy of the left renal vein (LRV) is more complicated than that of the right because of its complex embryogenesis and the collocative relationship with the abdominal aorta and the superior mesenteric artery. The LRV is normally anterior, and travels to the right side in front of the aorta. Developmental venous anomalies of the LRV occur as circumaortic or retroaortic LRV [27]. Many reports have indicated the clinical significance of retroaortic LRV (RLRV) or circumaortic left renal vein (CLRV) (also called “circumaortic venous ring”, or “renal collar”), e.g., in postpartum renal vein thrombosis with RLRV [41], gross hematuria, or microscopic hematuria attributed to RLRV with renal vein hypertension [12, 23], associated with the posterior nutcracker phenomenon or syndrome [8, 23, 32]. Furthermore, the LRV is normally located in the retroperitoneal space, in front of the renal artery. A retropelvic tributary (RPT) of the renal vein, also called the posterior primary tributary [35, 36], the posterior renal vein [30] or the supernumerary renal vein [30] is a common variation of the LRV; knowledge of the incidence and imaging features of the venous tributary is very important to avoid malpractice or hazardous results.
Although the anatomical variations, CLRV, RLRV, and RPT, have been well reported, statistical findings and analysis of their incidences are conflicting or limited in the literature. In this paper, three cadaver cases with anatomical variations of the LRV are described with special reference to a detailed review of the literature and meta-analysis in terms of either clinical reports or cadaver dissections.
Materials and methods
During routine gross dissection in the laboratory of the Anatomy Department of Tokyo Medical University in 2006–2007, three cases of anatomic variations of the LRV, CLRV, RLRV, and RPT were encountered.
Results
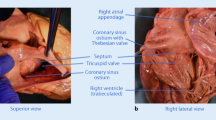
CLRV occurred in a 96-year-old Japanese male. The LRV split into two limbs of unequal caliber, which passed either in front of or behind the abdominal aorta to drain into a single inferior vena cava (IVC). The upper ventral limb received the left suprarenal vein and opened into the IVC at a normal level. The tenuity below the dorsal limb passed obliquely and downwards in the posterior aspect of the aorta to join the IVC 4.5 cm below the upper trunk (Fig. 1a).
Photograph of the CLRV (arrows in a), RLRV (b) and RPT (asterisk in c). The arrows (in c) showed the communicating veins between the RPT and lumbar and ascending lumbar veins. alr accessory left renal a.; ao aorta; ct celiac trunk; ivc inferior vena cava; im inferior mesenteric a.; lk left kidney; lov left ovarian v.; lr left renal a.; lrv left renal v.; lsrg left suprarenal gland; lsrv left suprarenal v.; lu left ureter; rk right kidney; rov right ovarian v.; rr right renal a.; rrv right renal v.; sm superior mesenteric a.
RLRV occurred in an 81-year-old Japanese female. The LRV, after receiving the suprarenal and ovarian veins, passed behind the aorta to join the IVC at the level between the second and third lumbar vertebrae (Fig. 1b).
RPT occurred in a 69-year-old Japanese female. The main trunk of the LRV received the ovarian and the suprarenal veins, and ran transversely in front of the aorta to empty into the IVC at the usual level. Besides the main trunk, an additional renal vein was located below the LRV and behind the renal pelvis and artery and joined the LRV via a thicker connecting trunk (Fig. 1c).
In all of the three cases, there were anastomosis between the CLRV/RLRV/RPT and the ascending lumbar veins and/or the second and third lumbar veins, in particular, the PRT presented complex anastomosis with the lumbar veins (Fig. 1a–c).
Discussion
In this study, three different anatomical variations of the LRV identified in cadaver dissection, the CLRV, RLRV, and RPT, were described.
The incidences of CLRV and RLRV in cadaver dissection and clinical observation (MDCT scan, MRI, angiography, surgical series) are shown in Tables 1 and 2, respectively. Case reports or studies with a small sample size (<100 subjects or samples) have not been included in Tables 1 and 2.
According to our statistics, the incidences of CLRV ranged from 0.6 to 17.0 % in cadaver dissection, and from 0.1 to 10.0 % in clinical reports (Tables 1, 2). The median incidences of CLRV were 7.0 % (200/2,839) in cadavers examined (Table 1) and 1.8 % (287/16,221) in clinical subjects examined (Table 2). This shows that CLRV is one of the most common congenital venous variations. The median incidence of CLRV in clinical reports was markedly lower than that with cadaver dissection. This might indicate that the detection of CLRV in CT/MDCT or angiography was relatively difficult compared with that in cadaver dissection. Among these findings, the detection of CLRV in angiography (10 %, [25]) was relatively easy compared with that in CT/MDCT (0.1 %, [14]; 0.3 %, [36]).
On the other hand, the incidences of isolated RLRV ranged from 0.5 to 3.5 % in cadaver dissection, and from 0.4 to 9.3 % in clinical reports (Tables 1, 2). The median incidences of RLRV were 1.7 % (52/2,999) in cadavers examined (Table 1) and 2.2 % (354/16,046) in clinical subjects examined (Table 2). This shows that the incidence of RLRV was not significantly different in cadaver dissection and clinical reports, although it was a little higher in cadaver dissection. However, rate of detection of RLRV in operations was the lowest (0.4 %, [7]; 0.5 %, [36], but relatively easy by ultrasonography (9.3 %, [18]).
The incidence of RPT is shown in Table 3. It was previously identified in 30.0 % [28], 30.4 % [30], and 46.4 % [35] of cases in cadaver dissection. This is very frequent.
Furthermore, the incidences of the communicating veins between the LRV and retroperitoneal veins, e.g., lumbar, ascending lumbar, capsular, and hemiazygos veins, are shown in Table 4. This was identified to range from 30.0 to 84.2 % in cadaver dissections (median of 68.7 %) and from 34.0 to 75.8 % in clinical reports (median of 57.5 %) (Table 4). Both had very high incidences of RPT, which were higher in cadaver dissection.
Moreover, most commonly, the location of the communicating vein was the second lumbar vein, but frequently the third lumbar vein, and, on occasion, both the second and the third lumbar veins [3, 4, 42]. As for our present cases, they usually involve communicating veins in the dorsal limb of the CLRV, or the RLRV, and/or the RPT, which receives easily drainage of the lumbar, vertebral, capsular, and hemiazygos systemic veins [4, 5, 24].
In summary, the veins in question, referred to as CLRV or RLRV, are not rare variations. In addition, the RPT showed high incidence and, thus, perhaps should not be called congenital variations (or aberrant veins, supernumerary veins), but rather usual features. The relatively high frequency of CLRV, RLRV, or the RPT and branches communicating with the retroperitoneal veins makes them one of the most common types of congenital variation. An understanding of this is essential in cases of renal transplantation, renal surgery, uroradiology, gonadal color Doppler imaging, surgery of aneurysm of abdominal aorta, and gonadal surgery.
References
Ahlberg NE, Bartley O, Chidekel N et al (1967) An anatomical and roentgenographic study of the communications of the renal vein in patients with and without renal carcinoma. Scand J Urol Nephrol 1:43–51
Aljabri B, MacDonald PS, Satin R et al (2001) Incidence of major venous and renal anomalies relevant to aortoiliac surgery as demonstrated by computed tomography. Ann Vasc Surg 15:615–618
Anson BJ, Cauldwell EW (1947) The pararenal vascular system a study of 425 anatomical specimens. Q Bull Northwest Univ Med Sch 21:320–328
Anson BJ, Cauldwell EW, Pick JW et al (1948) The anatomy of the pararenal system of veins, with comments on the renal arteries. J Urol 60:714–737
Anson BJ, Daseler EH (1961) Common variations in renal anatomy affecting blood supply, form and topography. Surg Gynecol Obst 112:439–449
Baniel J, Foster RS, Donohue JP (1995) Surgical anatomy of the lumbar vessels: implications for retroperitoneal surgery. J Urol 153:1422–1425
Costa HC, Moreira RJ, Fukunaga P et al (2011) Anatomic variations in vascular and collecting systems of kidneys from deceased donors. Transplant Proc 43:61–63
Cuéllar i Calàbria H, Quiroga Gómez S et al (2005) Nutcracker or left renal vein compression phenomenon: multidetector computed tomography findings and clinical significance. Eur Radiol 15:1745–1751
Davis RA, Milloy FJ, Anson BJ (1958) Lumbar, renal and associated parietal and visceral veins based upon a study of 100 specimens. Surg Gynecol Obstet 107:1–22
Davis CJ Jr, Lundberg GD (1968) Retroaortic left renal vein, a relatively frequent anomaly. Am J Clin Pathol 50:700–703
Dilli A, Ayaz UY, Karabacak OR et al (2012) Study of the left renal variations by means of magnetic resonance imaging. Surg Radiol Anat 34:267–270
Gibo M, Onitsuka H (1998) Retroaortic left renal vein with renal vein hypertension causing hematuria. Clin Imaging 22:422–424
Gillot C (1978) The left renal vein: anatomical study, angiographic aspects and surgical approach. Anat Clin 1:135–156
Hoeltl W, Hruby W, Aharinejad S (1990) Renal vein anatomy and its implications for retroperitoneal surgery. J Urol 143:1108–1114
Holden A, Smith A, Dukes P et al (2005) Assessment of 100 live potential renal donors for laparoscopic nephrectomy with multi-detector row helical CT. Radiology 237:973–980
Izumiyama M, Horiguchi M (1997) Two cases of the retroaortic left renal vein and a morphogenetic consideration of the anomalous vein. Acta Anat Nippon 72:535–543 (in Japanese)
Karaman B, Koplay M, Ozturk E et al (2007) Retroaortic left renal vein: multidetector computed tomography angiography findings and its clinical importance. Acta Radiol 48:355–360
Karazincir S, Balci A, Görür S et al (2007) Incidence of the retroaortic left renal vein in patients with varicocele. J Ultrasound Med 26:601–604
Kawamoto S, Lawler LP, Fishman EK (2005) Evaluation of the renal venous system on late arterial and venous phase images with MDCT angiography in potential living laparoscopic renal donors. AJR Am J Roentgenol 184:539–545
Koc Z, Ulusan S, Oguzkurt L (2007) Association of left renal vein variations and pelvic varices in abdominal MDCT. Eur Radiol 17:1267–1274
Koc Z, Ulusan S, Oguzkurt L et al (2007) Venous variants and anomalies on routine abdominal multi-detector row CT. Eur J Radiol 61:267–278
Kulkarni S, Emre S, Arvelakis A et al (2011) Multidetector CT angiography in living donor renal transplantation: accuracy and discrepancies in right venous anatomy. Clin Transplant 25:77–82
Lee S, Kim W, Kang KP et al (2007) Microscopic hematuria and the posterior nutcracker phenomenon. Kidney Int 72:1037
Li G, Dong J, Lu JS et al (2011) Anatomical variation of the posterior lumbar tributaries of the left renal vein in retroperitoneoscopic left living donor nephrectomy. Int J Urol 18:503–509
Lien HH, Kolbenstvedt A (1977) Phlebographic appearances of the left renal and left testicular veins. Acta Radiol Diagn 18:321–333
Lin CH, Steinberg AP, Ramani AP et al (2004) Laparoscopic live donor nephrectomy in the presence of circumaortic or retroaortic left renal vein. J Urol 171:44–46
Martinez-Almagro A, Almenar Garcia V, Martinez Sanjuan V et al (1992) Retroaortic left renal vein: a report of six cases. Surg Radiol Anat 14:361–366
Merklin RJ, Mitchels NA (1958) The variant renal and suprarenal blood supply with data on the inferior phrenic, ureteral and gonadal arteries: a statistical analysis based on 185 dissections and review of the literature. J Int Coll Surg 29:41–76
Natsis K, Tsitouridis I, Totlis T et al (2008) Proposal for classification of the circumaortic renal collar’s morphology. Am Surg 74:1190–1194
Okamoto K (1990) The posterior renal vein (new definition), together with its morphological significance. Okajimas Folia Anat Jpn 67:203–217
Pick JW, Anson BJ (1940) The renal vascular pedicle. An anatomical study of 430 body halves. J Urol 44:411–434
Rassi I, Khabbaz Z, Chelala D et al (2010) A new variant of the posterior nutcracker phenomenon. J Vasc Surg 51:1279
Reis RH, Esenther G (1959) Variations in the pattern of renal vessels and their relation to the type of posterior vena cava in man. Am J Anat 104:295–318
Royster TS, Lacey L, Marks RA (1974) Abdominal aortic surgery and the left renal vein. Am J Surg 127:552–554
Satyapal KS (1995) Classification of the drainage patterns of the renal veins. J Anat 186:329–333
Satyapal KS, Kalideen JM, Haffejee AA et al (1999) Left renal vein variations. Surg Radiol Anat 21:77–81
Seib GA (1934) The azygos system of veins in American whites and American negros, including observations on the inferior caval venous system. Am J Phys Anthrop 19:39–159
Shindo S, Kubota K, Kojima A et al (2000) Anomalies of inferior vena cava and left renal vein: risks in aortic surgery. Ann Vasc Surg 14:393–396
Srinivasan R (1979) The left renal vein. Mt Sinai J Med 46:559–563
Trigaux JP, Vandroogenbroek S, De Wispelaere JF et al (1998) Congenital anomalies of the inferior vena cava and left renal vein: evaluation with spiral CT. J Vasc Interv Radiol 9:339–345
Washecka R, Hulnick DH, Catanese A et al (1987) Postpartum renal vein thrombosis with left retroaortic renal vein. Urology 29:548–551
Yao Y, Okada Y, Yamato M et al (2003) Communicating vein between the left renal vein and left ascending lumber vein: incidence and significance on abdominal CT. Radiat Med 21:252–257
Yoshinaga K, Kawai K, Kodama K (2000) An anatomical study of the retroaortic left renal vein. Okajimas Folia Anat Jpn 77:47–52
Acknowledgments
We wish to thank Mr. Yoshitake Shiraishi for his technical assistance with the photographs.
Conflict of interest
We declare that we have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yi, SQ., Ueno, Y., Naito, M. et al. The three most common variations of the left renal vein: a review and meta-analysis. Surg Radiol Anat 34, 799–804 (2012). https://doi.org/10.1007/s00276-012-0968-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-012-0968-1