Abstract
Purpose
To assess the role and effectiveness of percutaneous arterial embolization (TAE) in patients with hemodynamic instability due to hypovolemic shock secondary to ruptured splanchnic artery pseudoaneurysms (SAPA).
Materials and Methods
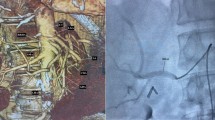
Seventeen patients (11 men, 6 women; mean age, 53 years) with hemodynamic instability (systolic blood pressure <90 mmHg) due to hypovolemic shock secondary to ruptured SAPA were treated by TAE. Clinical files, multidetector row computed tomography angiography, and angiographic examinations along with procedure details were reviewed.
Results
Seventeen SAPAs were present, predominantly located on gastroduodenal or pancreatic arteries (9/17; 53 %). Angiography showed extravasation of contrast medium from SAPA in 15/17 patients (88 %). Technical success rate of TAE was 100 %. TAE was performed using metallic coils in all patients (100 %), in association with gelatin sponge in 5/17 patients (29 %). TAE allowed controlling the bleeding and returning to normal hemodynamic status in 16/17 patients (94 %). In 1/17 patient (6 %), surgery was needed to definitively control the bleeding. The mortality and morbidity rate of TAE at 30 days were 0 and 12 %, respectively. Morbidity consisted in coil migration in 1/17 patient (6 %) and transient serum liver enzyme elevation in 1/17 patient (6 %).
Conclusion
TAE is an effective and safe treatment option for ruptured SAPA in hemodynamically unstable patients, with a success rate of 94 %. Our results suggest that TAE should be the favored option in patients with hemodynamic instability due to ruptured SAPA.


Similar content being viewed by others
References
Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ (2005) Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics 25:S173–S189
Ward WH, Platz TA, Pond KT, Southern FA, Moore EM (2009) Iatrogenic venous pseudoaneurysm: case report and review of the literature. Vascular 17:355–358
Dohan A, Soyer P, Subhani A, Hequet D, Fargeaudou Y, Morel O, Boudiaf M, Gayat E, Barranger E, Le Dref O, Sirol M (2013) Postpartum hemorrhage resulting from pelvic pseudoaneurysm: a retrospective analysis of 588 consecutive cases treated by arterial embolization. Cardiovasc Interv Radiol 36:1247–1255
Soyer P, Fargeaudou Y, Morel O, Boudiaf M, Le Dref O, Rymer R (2008) Severe postpartum haemorrhage from ruptured pseudoaneurysm: successful treatment with transcatheter arterial embolization. Eur Radiol 18:1181–1187
Cordova AC, Sumpio BE (2013) Visceral artery aneurysms and pseudoaneurysms—should they all be managed by endovascular techniques? Ann Vasc Dis 6:687–693
Mokrane FZ, Alba CG, Lebbadi M, Mejdoubi M, Moulabbi M, Lombard F et al (2013) Pseudoaneurism of the cystic artery treated with hyperselective embolisation alone. Diagn Interv Imaging 94:641–643
Boudghene F, L’Hermine C, Bigot JM (1993) Arterial complications of pancreatitis: diagnosis and therapeutic aspects in 104 cases. J Vasc Interv Radiol 4:551–558
Tessier DJ, Stone WM, Fowl RJ, Abbas MA, Andrews JC, Bower TC, Gloviczki P (2003) Clinical features and management of splenic artery pseudoaneurysm: case series and cumulative review of literature. J Vasc Surg 38:969–974
Agrawal GA, Johnson PT, Fishman EK (2007) Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. AJR Am J Roentgenol 188:992–999
Marshall GT, Howell DA, Hansen BL, Amberson SM, Abourjaily GS, Bredenberg CE (1996) Multidisciplinary approach to pseudoaneurysms complicating pancreatic pseudocysts. Impact of pretreatment diagnosis. Arch Surg 131:278–283
Ferrero E, Ferri M, Viazzo A, Robaldo A, Carbonatto P, Pecchio A, Chiecchio A, Nessi F (2011) Visceral artery aneurysms, an experience on 32 cases in a single center: treatment from surgery to multilayer stent. Ann Vasc Surg 25:923–935
Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, Ouriel K (2007) The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg 45:276–283
Udd M, Leppäniemi AK, Bidel S, Keto P, Roth WD, Haapiainen RK (2007) Treatment of bleeding pseudoaneurysms in patients with chronic pancreatitis. World J Surg 31:504–510
Song HH, Won YD, Kim YJ (2010) Transcatheter N-butyl cyanoacrylate embolization of pseudoaneurysms. J Vasc Interv Radiol 21:1508–1511
Cazejust J, Raynal M, Bessoud B, Tubiana JM, Menu Y (2012) Diagnosis and radiological treatment of digestive haemorrhage following supramesocolic surgery. Diagn Interv Imaging 93:e148–e158
Bergert H, Hinterseher I, Kersting S, Leonhoadt J, Bloomenthel A, Saeger HD et al (2005) Management and outcome of haemorrhage due to arterial pseudoaneurysms in pancreatitis. Surgery 137:323–328
Lau KY, Wong TP, Wong WW, Chan JK, Kan WK, Chan YF, Lee AS (2005) Transcatheter embolisation of visceral pseudoaneurysms—technical difficulties and modification of embolisation technique. Eur J Vasc Endovasc Surg 30:133–136
Loffroy R, Rao P, Ota S, De Lin M, Kwak BK, Krause D, Geschwind JF (2010) Packing technique for endovascular coil embolisation of peripheral arterial pseudo-aneurysms with preservation of the parent artery: safety, efficacy and outcomes. Eur J Vasc Endovasc Surg 40:209–215
Soyer P, Desgrippes A, Vallée JN, Rymer R (2000) Intrarenal pseudoaneurysm after percutaneous nephrostolithotomy: endovascular treatment with N-butyl-2-cyanoacrylate. Eur Radiol 10:1358
Tinto HR, Di Primio M, Tselikas L, Rico AP, Pellerin O, Pagny JY, Sapoval M (2014) Selective arterial embolization of life-threatening renal hemorrhage in four patients after partial nephrectomy. Diagn Interv Imaging. doi:10.1016/j.diii.2014.02.005
Goupil J, Fohlen A, Linard M, Vinatier L, Cuillier F, Collignon B, Storey J (2010) Ruptured uterine artery pseudo-aneurysm treated by embolization for post-partum bleeding: about 2 cases. J Gynecol Obstet Biol Reprod 39:325–330
Butori N, Coulange L, Filipuzzi L, Krausé D, Loffroy R (2009) Pseudoaneurysm of the uterine artery after cesarean delivery: management with superselective arterial embolization. Obstet Gynecol 113:540–543
Kobayashi L, Costantini TW, Coimbra R (2012) Hypovolemic shock resuscitation. Surg Clin North Am 92:1403–1423
Horton KM, Fishman EK (2003) Multidetector row and 3D CT of the mesenteric vasculature: normal anatomy and pathology. Semin Ultrasound CT MR 24:353–363
Liu PS, Platt JF (2014) CT angiography in the abdomen: a pictorial review and update. Abdom Imaging 39:196–214
Vimalraj V, Kannan DG, Sukumar R, Rajendran S, Jeswanth S, Jyotibasu D, Ravichandran P, Balachandar TG, Surendran R (2009) Haemosuccus pancreaticus: diagnostic and therapeutic challenges. HPB (Oxford) 11:345–350
Dohan A, Dautry R, Le Dref O, Soyer P (2014) Avoiding radiation in management of post-partum hemorrhage: CT angiography is not a good idea. Eur J Obstet Gynecol Reprod Biol. doi:10.1016/j.ejogrb.2014.03.022
Pilleul F, Forest J, Beuf O (2006) Magnetic resonance angiography of splanchnic artery aneurysms and pseudoaneurysms. J Radiol 87:127–1231
Chadha M, Ahuja C (2009) Visceral artery aneurysms: diagnosis and percutaneous management. Semin Interv Radiol 26:196–206
Fargeaudou Y, Le Dref O, Soyer P, Rao P, Boudiaf M, Sirol M, Dahan H, Hamzi L, Rymer R (2009) Life-threatening intra-abdominal hemorrhage from left superior colonic artery pseudoaneurysm after percutaneous renal biopsy: successful treatment with superselective arterial embolization. Clin Imaging 33:474–477
Yamakado K, Nakatsuka A, Tanaka N, Takano K, Matsumura K, Takeda K (2000) Transcatheter arterial embolization of ruptured pseudoaneurysms with coils and n-butyl cyanoacrylate. J Vasc Interv Radiol 11:66–72
Vainas T, Klompenhouwer E, Duijm L, Tielbeek X, Teijink J (2012) Endovascular treatment of a hepatic artery pseudoaneurysm associated with gastrointestinal tract bleeding. J Vasc Surg 55:1145–1149
Conflict of interest
Anthony Dohan, Clarisse Eveno, Raphael Dautry, Youcef Guerrache, Marine Camus, Mourad Boudiaf, Etienne Gayat, Olivier Le Dref, Marc Sirol, Philippe Soyer declare that they have no conflicts of interest.
Statement of Informed Consent
“Informed consent was obtained from all individual participants included in the study.”
Statement of Human Rights
“All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Author information
Authors and Affiliations
Corresponding author
Additional information
Splanchnic artery pseudoaneurysms are safely and effectively treated by arterial embolization in hemodynamically unstable patients.
Rights and permissions
About this article
Cite this article
Dohan, A., Eveno, C., Dautry, R. et al. Role and Effectiveness of Percutaneous Arterial Embolization in Hemodynamically Unstable Patients with Ruptured Splanchnic Artery Pseudoaneurysms. Cardiovasc Intervent Radiol 38, 862–870 (2015). https://doi.org/10.1007/s00270-014-1002-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-014-1002-2