Abstract
Background
The decision to perform a total thyroidectomy (TT) for unilateral papillary thyroid microcarcinoma (PTMC) with nodules in the contralateral lobe remains controversial. The aim of this study was to investigate the rate of contralateral carcinomas that are preoperatively misdiagnosed as benign.
Methods
From October 2011 to October 2015, a total of 347 patients with unilateral PTMC and contralateral benign nodules who were treated with a TT at a single institution were enrolled. All patients underwent preoperative fine needle aspiration and ultrasonography (US). Clinicopathological features such as age, sex, laterality, tumor size, central lymph node metastases, capsular invasion, TgAb and TPOAb levels, Hashimoto’s thyroiditis, nodule number in both lobes according to preoperative US, and primary carcinoma number in the final postoperative pathology report were all analyzed to investigate the rate and predictive factors of contralateral carcinoma.
Results
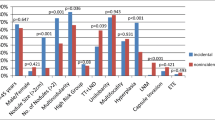
A total of 100 patients (28.9 %) were diagnosed with papillary thyroid carcinoma in the contralateral lobe. A multivariate analysis showed that tumor size, nodule number in the contralateral lobe, and multifocality of the primary tumor were all independent predictive factors of contralateral carcinoma in patients with unilateral PTMC and contralateral benign nodules.
Conclusions
According to our findings, the rate at which contralateral carcinomas are preoperatively misdiagnosed as benign is 28.9 %. A TT is essential for unilateral PTMC with a primary tumor size >5 mm, multifocal primary carcinomas or multifocal benign nodules in the contralateral lobe.

Similar content being viewed by others
References
Leenhardt L, Grosclaude P, Cherie-Challine L (2004) Increased incidence of thyroid carcinoma in France: a true epidemic or thyroid nodule management effects? Report from the French Thyroid Cancer Committee. Thyroid 14:1056–1060
Liu S, Semenciw R, Ugnat AM et al (2001) Increasing thyroid cancer incidence in Canada, 1970–1996: time trends and age-period-cohort effects. Br J Cancer 85:1335–1339
Chen AY, Jemal A, Ward EM (2009) Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer 115:3801–3807
Li N, Du XL, Reitzel LR et al (2013) Impact of enhanced detection on the increase in thyroid cancer incidence in the United States: review of incidence trends by socioeconomic status within the surveillance, epidemiology, and end results registry, 1980–2008. Thyroid 23:103–110
Schonberger J, Marienhagen J, Agha A et al (2007) Papillary microcarcinoma and papillary cancer of the thyroid ≤1 cm: modified definition of the WHO and the therapeutic dilemma. Nuklearmedizin 46:115–120
Randolph GW, Daniels GH (2002) Radioactive iodine lobe ablation as an alternative to completion thyroidectomy for follicular carcinoma of the thyroid. Thyroid 12:989–996
Kiernan CM, Parikh AA, Parks LL et al (2015) Use of radioiodine after thyroid lobectomy in patients with differentiated thyroid cancer: does it change outcomes? J Am Coll Surg 220:617–625
Lei S, Ding Z, Ge J et al (2015) Association between prognostic factors and clinical outcome of well-differentiated thyroid carcinoma: a retrospective 10-year follow-up study. Oncol Lett 10:1749–1754
Koo BS, Lim HS, Lim YC et al (2010) Occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma. Ann Surg Oncol 17:1101–1105
Lee KJ, Cho YJ, Kim JG et al (2013) How many contralateral papillary thyroid carcinomas can be missed? World J Surg 37:780–785
Lee YC, Eun YG, Sohn YM et al (2015) Predictive factors for occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma by preoperative ultrasonographic and pathological features. World J Surg 39:1736–1741
Pitt SC, Sippel RS, Chen H (2009) Contralateral papillary thyroid cancer: does size matter? Am J Surg 197:342–347
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295:2164–2167
Sugitani I, Toda K, Yamada K et al (2010) Three distinctly different kinds of papillary thyroid microcarcinoma should be recognized: our treatment strategies and outcomes. World J Surg 34:1222–1231
Miyauchi A (2016) Clinical trials of active surveillance of papillary microcarcinoma of the thyroid. World J Surg 40:516–522
Oda H, Miyauchi A, Ito Y et al (2016) Incidences of unfavorable events in the management of low-risk papillary microcarcinoma of the thyroid by active surveillance versus immediate surgery. Thyroid 26:150–155
Wang W, Zhao W, Wang H et al (2012) Poorer prognosis and higher prevalence of BRAF (V600E) mutation in synchronous bilateral papillary thyroid carcinoma. Ann Surg Oncol 19:31–36
Frates MC, Benson CB, Doubilet PM et al (2006) Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocrinol Metab 91:3411–3417
Kwong N, Medici M, Angell TE et al (2015) The influence of patient age on thyroid nodule formation, multinodularity, and thyroid cancer risk. J Clin Endocrinol Metab 100:4434–4440
McCarthy RP, Wang M, Jones TD et al (2006) Molecular evidence for the same clonal origin of multifocal papillary thyroid carcinomas. Clin Cancer Res 12:2414–2418
Wang W, Wang H, Teng X et al (2010) Clonal analysis of bilateral, recurrent, and metastatic papillary thyroid carcinomas. Hum Pathol 41:1299–1309
Jovanovic L, Delahunt B, McIver B et al (2010) Distinct genetic changes characterise multifocality and diverse histological subtypes in papillary thyroid carcinoma. Pathology 42:524–533
Hoang JK, Lee WK, Lee M et al (2007) US features of thyroid malignancy: pearls and pitfalls. Radiographics 27:847–860
Ko HM, Jhu IK, Yang SH et al (2003) Clinicopathologic analysis of fine needle aspiration cytology of the thyroid. A review of 1,613 cases and correlation with histopathologic diagnoses. Acta Cytol 47:727–732
Baek HJ, Kim DW, Ryu JH (2015) Association between TNM staging system and histopathological features in patients with papillary thyroid carcinoma. Endocrine 48:589–594
Joo JY, Jin J, Seo ST et al (2015) Recurrence in regional lymph nodes after total thyroidectomy and neck dissection in patients with papillary thyroid cancer. Oral Oncol 51:164–169
Ito Y, Miyauchi A, Inoue H et al (2010) An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg 34:28–35
Osmolski A, Frenkiel Z, Osmolski R (2006) Complications in surgical treatment of thyroid diseases. Otolaryngol Pol 60:165–170
Matsuzu K, Sugino K, Masudo K et al (2014) Thyroid lobectomy for papillary thyroid cancer: long-term follow-up study of 1,088 cases. World J Surg 38:68–79
Donatini G, Castagnet M, Desurmont T et al (2016) Partial thyroidectomy for papillary thyroid microcarcinoma: is completion total thyroidectomy indicated? World J Surg 40:510–515
Rafferty MA, Goldstein DP, Rotstein L et al (2007) Completion thyroidectomy versus total thyroidectomy: is there a difference in complication rates? An analysis of 350 patients. J Am Coll Surg 205:602–607
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Wu, Z.G., Yan, X.Q., Su, R.S. et al. How Many Contralateral Carcinomas in Patients with Unilateral Papillary Thyroid Microcarcinoma are Preoperatively Misdiagnosed as Benign?. World J Surg 41, 129–135 (2017). https://doi.org/10.1007/s00268-016-3701-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3701-0