Abstract
Background
We previously established an optimal postoperative drain management rule after liver resection (i.e., drain removal on postoperative day 3 if the drain fluid bilirubin concentration is <3 mg/dl) from the results of 514 drains of 316 consecutive patients. This test set predicts that 274 of 316 patients (87.0 %) will be safely managed without adverse events when drain management is performed without deviation from the rule.
Objective
To validate the feasibility of our rule in recent time period.
Methods
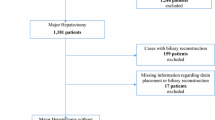
The data from 493 drains of 274 consecutive patients were prospectively collected. Drain fluid volumes, bilirubin levels, and bacteriological cultures were measured on postoperative days (POD) 1, 3, 5, and 7. The drains were removed according to the management rule. The achievement rate of the rule, postoperative adverse events, hospital stay, medical costs, and predictive value for reoperation according to the rule were validated.
Results
The rule was achieved in 255 of 274 (93.1 %) patients. The drain removal time was significantly shorter [3 days (1–30) vs. 7 (2–105), p < 0.01], drain fluid infection was less frequent [4 patients (1.5 %) vs. 58 (18.4 %), p < 0.01], postoperative hospital stay was shorter [11 days (6–73) vs. 16 (9–59), p = 0.04], and medical costs were decreased [1453 USD (968–6859) vs. 1847 (4667–9498), p < 0.01] in the validation set compared with the test set. Five patients who required reoperation were predicted by the drain-based information and treated within 2 days after operation.
Conclusions
Our 3 × 3 rule is clinically feasible and allows for the early removal of the drain tube with minimum infection risk after liver resection.

Similar content being viewed by others
References
Liu CL, Fan ST, Lo CM, Wong Y, Ng IO, Lam CM et al (2004) Abdominal drainage after hepatic resection is contraindicated in patients with chronic liver diseases. Ann Surg 239:194–201
Brooke-Smith M, Figueras J, Ullah S, Rees M, Vauthey JN, Hugh TJ et al (2015) Prospective evaluation of the International Study Group for liver surgery definition of bile leak after a liver resection and the role of routine operative drainage: an international multicentre study. HPB. 17:46–51
Franco D, Karaa A, Meakins JL, Borgonovo G, Smadja C, Grange D (1989) Hepatectomy without abdominal drainage: results of a prospective study in 61 patients. Ann Surg 210:748–750
Belghiti J, Kabbej M, Sauvanet A, Vilgrain V, Panis Y, Fekete F (1993) Drainage after elective hepatic resection: a randomized trial. Ann Surg 218:748–753
Fong Y, Brennan MF, Brown K, Heffernan N, Blumgart LH (1996) Drainage is unnecessary after elective liver resection. Am J Surg 171:158–162
Lu L, Sun HC, Qin LX, Wang L, Ye QH, Ren N et al (2006) Abdominal drainage was unnecessary after hepatectomy using the conventional clamp crushing technique. J Gastrointest Surg. 10:302–308
Sun HC, Qin LX, Lu L, Wang L, Ye QH, Ren N et al (2006) Randomized clinical trial of the effects of abdominal drainage after elective hepatectomy using the crushing clamp method. Br J Surg 93:422–426
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 149:680–688
Rahbari NN, Garden OJ, Padbury R, Maddern G, Koch M, Hugh TJ et al (2011) Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford). 13:528–535
Yamazaki S, Takayama T, Moriguchi M, Mitsuka Y, Okada S, Midorikawa Y et al (2012) Criteria for drain removal following liver resection. Br J Surg 99:1584–1590
Takayama T, Makuuchi M, Kubota K, Harihara Y, Hui AM, Sano K et al (2001) Randomized comparison of ultrasonic vs clamp transection of the liver. Arch Surg 136:922–928
Imamura H, Takayama T, Sugawara Y, Kokudo N, Aoki T, Kaneko J et al (2002) Pringle`s maneuver in living donors. Lancet 360:2049–2050
Yamazaki S, Takayama T, Kimura Y, Moriguchi M, Higaki T, Nakayama H et al (2011) Transfusion criteria for fresh frozen plasma in liver resection: a 3 + 3 cohort expansion study. Arch Surg 146:1293–1299
Hayashi Y, Takayama T, Yamazaki S, Moriguchi M, Ohkubo T, Nakayama H et al (2011) Validation of perioperative steroids administration in liver resection: a randomized controlled trial. Ann Surg 253:50–55
Yamazaki S, Takayama T, Nakamura M, Higaki T, Matsuoka S, Mizuno S et al (2014) Prophylactic impact of endoscopic treatment for esophageal varices in liver resection: a prospective study. J Gastroenterol 49:917–922
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Rahbari NN, Elbers H, Koch M, Kirchberg J, Dutlu M, Mehrabi A et al (2012) Bilirubin level in the drainage fluid is an early and independent predictor of clinically relevant bile leakage after hepatic resection. Surgery 152:821–831
Torzilli G, Olivari N, Del Fabbro D, Gambetti A, Leoni P, Gendarini A et al (2005) Bilirubin level fluctuation in drain discharge after hepatectomies justifies long-term drain maintenance. Hepatogastroenterology 52:1206–1210
Nagano Y, Togo S, Tanaka K, Masui H, Endo I, Sekido H et al (2003) Risk factors and management of bile leakage after hepatic resection. World J Surg 27:695–698
Yamashita Y, Hamatsu T, Rikimaru T, Tanaka S, Shirabe K, Shimada M et al (2001) Bile leakage after hepatic resection. Ann Surg 233:45–50
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mitsuka, Y., Yamazaki, S., Yoshida, N. et al. Prospective Validation of Optimal Drain Management “The 3 × 3 Rule” after Liver Resection. World J Surg 40, 2213–2220 (2016). https://doi.org/10.1007/s00268-016-3523-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3523-0