Abstract
Introduction
Laryngeal nerve monitoring has been increasingly embraced as a mechanism for mitigating the risk of nerve damage during thyroid and parathyroid surgery. Vagal nerve monitoring has recently been introduced as a potentially increased level of nerve integrity scrutiny. We sought to define the risks and benefits of this technology in a prospective analysis of a series of patients undergoing neck endocrine surgery.
Setting
High-volume academic endocrine surgery practice.
Methods
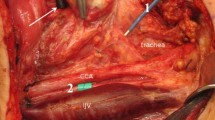
A prospective, non-controlled trial of continuous vagal nerve monitoring (CVNM) in a projected cohort of 20 non-randomly selected patients undergoing thyroid and parathyroid surgery was planned. A commercially available nerve monitoring system with automatic periodic stimulation was utilized for both laryngeal nerve monitoring and CVNM. Demographic data were obtained, and outcome variables included surgical procedures performed, pathology, complications, incremental time required to achieve CVNM, and benefits of monitoring and stimulation.
Results
The patient accrual was aborted after 9 surgeries (12 nerves monitored) because of two serious adverse events (hemodynamic instability and reversible vagal neuropraxia attributable to the monitoring apparatus). No other complications occurred. The time to establish monitoring ranged from 3 to 26 min, with a median of 6 min (representing 2.9–12.2 % of the total surgical procedural time). The stimulation clamp became dislodged 11 times in 5 cases and was replaced in 7 of those instances. Benefits of CVNM included recognition of reduced amplitude and increased nerve latency in two patients.
Conclusions
We report the first evidence that CVNM may cause serious patient harm. This novel approach is invasive and threatens patient safety. Although it may occasionally provide meaningful information, the risk–benefit ratio does not favor widespread adoption.



Similar content being viewed by others
References
Holm TM, Pai SI (2013) The superior laryngeal nerve. In: Miccoli P, Terris DJ, Minuto MN, Seybt MW (eds) Thyroid surgery: preventing and managing complications. Wiley-Blackwell, Oxford
Prioleau WH (1933) Injury of laryngeal branches of vagus nerve in thyroid surgery. South Surg 1:287–292
Lahey FH, Hoover WB (1938) Injuries to the recurrent laryngeal nerve in thyroid operations: their management and avoidance. Ann Surg 108(4):545–562
Randolph GW, Dralle H, International Intraoperative Monitoring Study Group (2011) Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 121(Suppl 1):S1–S16
Snyder SK, Hendricks JC (2005) Intraoperative neurophysiology testing of the recurrent laryngeal nerve: plaudits and pitfalls. Surgery 138(6):1183–1191
Dralle H, Sekulla C, Haerting J, Timmermann W, Neumann HJ, Kruse E, Grond S, Mühlig HP, Richter C, Voss J, Thomusch O, Lippert H, Gastinger I, Brauckhoff M, Gimm O (2004) Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 136(6):1310–1322
Schneider R, Randolph GW, Sekulla C, Phelan E, Thanh PN, Bucher M, Machens A, Dralle H, Lorenz K (2013) Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury. Head Neck 35(11):1591–1598
Seybt MW, Terris DJ (2010) Outpatient thyroidectomy: experience in over 200 patients. Laryngoscope 120(5):959–963
Miccoli P, Berti P, Materazzi G, Massi M, Picone A, Minuto MN (2004) Results of video-assisted parathyroidectomy: single institution’s six-year experience. World J Surg 28(12):1216–1218. doi:10.1007/s00268-004-7638-3
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM, American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(11):1167–1214
McWade MA, Paras C, White LM, Phay JE, Mahadevan-Jansen A, Broome JT (2013) A novel optical approach to intraoperative detection of parathyroid glands. Surgery 154(6):1371–1377
James BC, Nagar S, Tracy M, Kaplan EL, Angelos P, Scherberg NH, Grogan RH (2014) A novel, ultrarapid parathyroid hormone assay to distinguish parathyroid from nonparathyroid tissue. Surgery 156(6):1638–1643
Yarbrough DE, Thompson GB, Kasperbauer JL, Harper CM, Grant CS (2004) Intraoperative electromyographic monitoring of the recurrent laryngeal nerve in reoperative thyroid and parathyroid surgery. Surgery 136(6):1107–1115
Eisele DW (1996) Intraoperative electrophysiologic monitoring of the recurrent laryngeal nerve. Laryngoscope 106(4):443–449
Wu CW, Dionigi G, Chen HC, Chen HY, Lee KW, Lu IC, Chang PY, Hsiao PJ, Ho KY, Chiang FY (2013) Vagal nerve stimulation without dissecting the carotid sheath during intraoperative neuromonitoring of the recurrent laryngeal nerve in thyroid surgery. Head Neck 35(10):1443–1447
Phelan E, Schneider R, Lorenz K, Dralle H, Kamani D, Potenza A, Sritharan N, Shin J, Randolph GW (2014) Continuous vagal IONM prevents recurrent laryngeal nerve paralysis by revealing initial EMG changes of impending neuropraxic injury: a prospective, multicenter study. Laryngoscope 124(6):1498–1505
Ulmer C, Friedrich C, Kohler A, Rieber F, Basar T, Deuschle M, Thon KP, Lamadé W (2011) Impact of continuous intraoperative neuromonitoring on autonomic nervous system during thyroid surgery. Head Neck 33(7):976–984
Kuppersmith RB, Holsinger FC (2011) Robotic thyroid surgery: an initial experience with North American patients. Laryngoscope 121(3):521–526
McCulloch P et al (2009) No surgical innovation without evaluation: the IDEAL recommendations. Lancet 374(9695):1105–1112
Angelos P (2010) The ethical challenges of surgical innovation for patient care. Lancet 376(9746):1046–1047
Hemmerling TM (2008) Monitoring neural function during surgery around the glossopharyngeal, vagus and laryngeal nerves during neck (thyroid, larynx, carotid) and chest procedures. Handbook of clinical neurophysiology, vol. 8. pp 590–606
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terris, D.J., Chaung, K. & Duke, W.S. Continuous Vagal Nerve Monitoring is Dangerous and Should not Routinely be Done During Thyroid Surgery. World J Surg 39, 2471–2476 (2015). https://doi.org/10.1007/s00268-015-3139-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3139-9