Abstract
Objective
To assess the outcome of conservative treatment of severe critical limb ischemia (CLI) classified as Rutherford 5/6.
Background
The preferred therapy for CLI is either endovascular revascularization or bypass surgery. With a growing aged population with more serious comorbidities, these therapies are not always a viable option. Primary amputation leads to decreased mobility and a reduced quality of life. There is a lack of literature regarding the outcome of conservative therapy.
Methods
Hospital charts were reviewed of all patients who were diagnosed with Rutherford classification 5–6 and received conservative treatment and lacked interventional options. Outcome measures were mortality, complete wound closure, and limb salvage rate.
Results
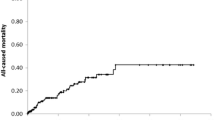
38 patients were included with a median age of 80 years (range 57–97). The amputation rate during follow-up was 16 %. In 58 % of patients, complete wound closure was achieved. All-cause mortality was 58 % with a 2-year survivability rate of 55 %.
Conclusions
Conservative management in our selected patients with CLI results in a moderate rate of wound closure and acceptable amputation rates albeit with a high mortality rate. For patients not eligible for endovascular revascularization or bypass surgery, conservative treatment could be a viable option besides primary limb amputation.

Similar content being viewed by others
References
Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG et al (2007) Inter-society consensus for the management of peripheral arterial disease (TASC II). Eur J Vasc Endovasc Surg 33(Suppl 1):S1–S75
Hankey GJ (2005) Vascular disease of the heart, brain and limbs: new insights into a looming epidemic. Lancet 366(9499):1753–1754
Pomposelli FB, Kansal N, Hamdan AD, Belfield A, Sheahan M, Campbell DR et al (2003) A decade of experience with dorsalis pedis artery bypass: analysis of outcome in more than 1000 cases. J Vasc Surg 37(2):307–315
Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes JF et al (2005) Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 366(9501):1925–1934
de Leur K, van Zeeland ML, Ho GH, de Groot HG, Veen EJ, van der Laan L (2012) Treatment for critical lower limb ischemia in elderly patients. World J Surg 36(12):2937–2943. doi:10.1007/s00268-012-1758-y
Andraeni D (1991) Second European Consensus Document on chronic critical leg ischemia. Circulation, 84(Suppl 4):1–26
Hiatt WR (2001) Medical treatment of peripheral arterial disease and claudication. N Engl J Med 344(21):1608–1621
Teraa M, Sprengers RW, van der Graaf Y, Peters CE, Moll FL, Verhaar MC (2013) Autologous bone marrow-derived cell therapy in patients with critical limb ischemia: a meta-analysis of randomized controlled clinical trials. Ann Surg 258(6):922–929
Fitz-Henry J (2011) The ASA classification and peri-operative risk. Ann R Coll Surg Engl 93(3):185–187
World Health Organisation Pain Ladder .http://www.who.int/cancer/palliative/painladder/en/. Accessed 8 Feb 2015
Marston WA, Davies SW, Armstrong B, Farber MA, Mendes RC, Fulton JJ et al (2006) Natural history of limbs with arterial insufficiency and chronic ulceration treated without revascularization. J Vasc Surg 44(1):108–114
Wolcott RD, Rhoads DD (2008) A study of biofilm-based wound management in subjects with critical limb ischaemia. J Wound Care 17(4):145–8, 50–2, 54–5
Ruangsetakit C, Chinsakchai K, Mahawongkajit P, Wongwanit C, Mutirangura P (2010) Transcutaneous oxygen tension: a useful predictor of ulcer healing in critical limb ischaemia. J Wound Care 19(5):202–206
Nehler MR, Hiatt WR, Taylor LM Jr (2003) Is revascularization and limb salvage always the best treatment for critical limb ischemia? J Vasc Surg 37(3):704–708
Lepantalo M, Matzke S (1996) Outcome of unreconstructed chronic critical leg ischaemia. Eur J Vasc Endovasc Surg 11(2):153–157
Bosma J, Vahl A, Wisselink W (2013) Systematic review on health-related quality of life after revascularization and primary amputation in patients with critical limb ischemia. Ann Vasc Surg 27(8):1105–1114
Acknowledgments
We would like to thank our specialized wound care practitioners for their help with delivering the necessary data.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomas, A.R., Raats, J.W., Lensvelt, M.M.A. et al. Conservative Treatment in Selected Patients with Severe Critical Limb Ischemia. World J Surg 39, 2090–2095 (2015). https://doi.org/10.1007/s00268-015-3069-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3069-6