Abstract
Background
According to the Louisville Statement, laparoscopic major hepatectomy is a heterogeneous category that includes “traditional” trisectionectomies/hemi-hepatectomies and the technically challenging resection of segments 4a, 7, and 8. The aims of this study were to assess differences in clinical outcomes between laparoscopic “traditional” major hepatectomy and resection of “difficult-to-access” posterosuperior segments and to define whether the current classification is clinically valid or needs revision.
Methods
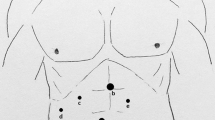
We reviewed a prospectively collected single-center database of 390 patients undergoing pure laparoscopic liver resection. A total of 156 patients who had undergone laparoscopic major hepatectomy according to the Louisville Statement were divided into two subcategories: laparoscopic “traditional” major hepatectomy (LTMH), including hemi-hepatectomies and trisegmentectomies, and laparoscopic “posterosuperior” major hepatectomy (LPMH), including resection of posterosuperior segments 4a, 7, and 8. LTMH and LPMH subgroups were compared with respect to demographics, intraoperative variables, and postoperative outcomes.
Results
LTMH was performed in 127 patients (81 %) and LPMH in 29 (19 %). Operation time was a median 330 min for LTMH and 210 min for LPMH (p < 0.0001). Blood loss was a median 500 ml for LTMH and 300 ml for LPMH (p = 0.005). Conversion rate was 9 % for LTMH and nil for LPMH (p = 0.219). In all, 28 patients (22 %) developed postoperative complications after LTMH and 5 (17 %) after LPMH (p = 0.801). Mortality rate was 1.6 % after LTMH and nil after LPMH. Hospital stay was a median 5 days after LTMH and 4 days after LPMH (p = 0.026).
Conclusions
The creation of two subcategories of laparoscopic major hepatectomy seems appropriate to reflect differences in intraoperative and postoperative outcomes between LTMH and LPMH.
Similar content being viewed by others
References
Buell JF, Cherqui D, Geller DA et al (2009) The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg 250:825–830
Tzanis D, Shivathirthan N, Laurent A et al (2013) European experience of laparoscopic major hepatectomy. J Hepatobiliary Pancreat Sci 20:120–124
Croome KP, Yamashita MH (2010) Laparoscopic vs open hepatic resection for benign and malignant tumors: an updated meta-analysis. Arch Surg 145:1109–1118
Nguyen KT, Marsh JW, Tsung A et al (2011) Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg 146:348–356
Abu Hilal M, Di Fabio F, Abu Salameh M et al (2012) Oncological efficiency analysis of laparoscopic liver resection for primary and metastatic cancer: a single-center UK experience. Arch Surg 147:42–48
Abu Hilal M, Di Fabio F, Syed S et al (2013) Assessment of the financial implications for laparoscopic liver surgery: a single-center UK cost analysis for minor and major hepatectomy. Surg Endosc 27:2542–2550
Vanounou T, Steel JL, Nguyen KT et al (2010) Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol 17:998–1009
Polignano FM, Quyn AJ, de Figueiredo RS et al (2008) Laparoscopic versus open liver segmentectomy: prospective, case-matched, intention-to-treat analysis of clinical outcomes and cost effectiveness. Surg Endosc 22:2564–2570
Bhojani FD, Fox A, Pitzul K et al (2012) Clinical and economic comparison of laparoscopic to open liver resections using a 2-to-1 matched pair analysis: an institutional experience. J Am Coll Surg 214:184–195
Dagher I, O’Rourke N, Geller DA et al (2009) Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg 250:856–860
Balzan S, Belghiti J, Farges O et al (2005) The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242:824–828
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Strasberg SM (2005) Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 12:351–355
Pearce NW, Di Fabio F, Teng MJ et al (2011) Laparoscopic right hepatectomy: a challenging, but feasible, safe and efficient procedure. Am J Surg 202:e52–e58
Pearce NW, Di Fabio F, Abu Hilal M (2011) Laparoscopic left hepatectomy with extraparenchymal inflow control. J Am Coll Surg 213:e23–e27
Abu Hilal M, Underwood T, Zuccaro M et al (2010) Short- and medium-term results of totally laparoscopic resection for colorectal liver metastases. Br J Surg 97:927–933
Lin NC, Nitta H, Wakabayashi G (2013) Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. Ann Surg 257:205–213
Costi R, Capelluto E, Sperduto N et al (2003) Laparoscopic right posterior hepatic bisegmentectomy (segments VII–VIII). Surg Endosc 17:162
Cho JY, Han HS, Yoon YS et al (2008) Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 144:32–38
Cheng KC, Yeung YP, Hui J et al (2011) Multimedia manuscript: laparoscopic resection of hepatocellular carcinoma at segment 7: the posterior approach to anatomic resection. Surg Endosc 25:3437
Kazaryan AM, Røsok BI, Marangos IP et al (2011) Comparative evaluation of laparoscopic liver resection for posterosuperior and anterolateral segments. Surg Endosc 25:3881–3889
Ishizawa T, Gumbs AA, Kokudo N et al (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256:959–964
Troisi RI, Montalti R, Van Limmen JG et al (2014) Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB (Oxford) 16:75–82
Herman P, Krüger JA, Perini MV et al (2013) Laparoscopic hepatic posterior sectionectomy: a hand-assisted approach. Ann Surg Oncol 20:1266
Cardinal JS, Reddy SK, Tsung A et al (2013) Laparoscopic major hepatectomy: pure laparoscopic approach versus hand-assisted technique. J Hepatobiliary Pancreat Sci 20:114–119
Troisi RI, Patriti A, Montalti R et al (2013) Robot assistance in liver surgery: a real advantage over a fully laparoscopic approach? Results of a comparative bi-institutional analysis. Int J Med Robot 9:160–166
Casciola L, Patriti A, Ceccarelli G et al (2011) Robot-assisted parenchymal-sparing liver surgery including lesions located in the posterosuperior segments. Surg Endosc 25:3815–3824
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Di Fabio, F., Samim, M., Di Gioia, P. et al. Laparoscopic Major Hepatectomies: Clinical Outcomes and Classification. World J Surg 38, 3169–3174 (2014). https://doi.org/10.1007/s00268-014-2724-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2724-7