Abstract
Background
The present qualitative study explores surgeons’ experiences and coping mechanisms with the death of their patients in the context of life-limiting illnesses.
Methods
Nine Australian surgeons participated in in-depth interviews. Thematic analysis of the interview transcriptions allowed for identification of themes and subthemes. Methodological trustworthiness and rigor were preserved at all stages of the research process.
Results
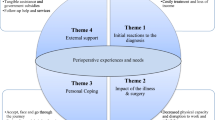
The essence of surgical practice, comprising participants’ descriptions of their identity as surgeons, influenced their experiences and coping mechanisms when dealing with death and dying. The following subthemes were identified: distancing from patients, wanting to fix problems, doing in terms of operating on a patient, prominence of the surgeon’s personal ability, and high personal responsibility for patient outcomes. Giving hope and having a mixed surgical practice were some of the coping mechanisms described by participants.
Discussion
Death and dying are a part of surgical practice, and surgeons face challenges as they care for dying patients. Although participants stated that they felt less affected by dealing with patients dying of life-limiting illnesses than by unexpected deaths, their descriptions of their encounters, reactions, and behaviors, as well as their use of language, suggest that these deaths have a lasting impact. Potential areas for improvement of surgical practice and approaches to teaching about death and dying in surgery are addressed. Furthermore, the results of this study suggest the need to expand research in this area.

Similar content being viewed by others
References
Bradley CT, Brasel KJ (2008) Core competencies in palliative care for surgeons: interpersonal and communication skills. Am J Hosp Palliat Care 24:499–507
Dunn GP, Milch RA (2001) Introduction and historical background of palliative care: where does the surgeon fit in? J Am Coll Surg 193:325–328
Guest RS, Baser R, Li Y et al (2011) Cancer surgeons’ distress and well-being. I: the tension between a culture of productivity and the need for self-care. Ann Surg Oncol 18:1229–1235
Kearney MK, Weininger RB, Vachon MLS et al (2009) Self-care of physicians caring for patients at the end of life: “being connected … a key to my survival”. JAMA 301:1155–1164
Torjuul K, Nordam A, Sorlie V (2005) Ethical challenges in surgery as narrated by practicing surgeons. BMC Med Ethics 6:2
Page DW (2011) Are surgeons capable of introspection? Surg Clin North Am 91:293–304
McGreevy J, Wiebe D (2002) A preliminary measurement of the surgical personality. Am J Surg 184:121–125
Stabile BE (2008) The surgeon: a changing profile. Arch Surg 143:827–831
Cassell J (1986) Dismembering the image of God: surgeons, heroes, wimps and miracles. Anthropol Today 2:13–15
Cassell J (1987) On control, certitude, and the “paranoia” of surgeons. Cult Med Psychiatry 11:229–249
Buchman TG, Cassell J, Ray SE et al (2002) Who should manage the dying patient?: rescue, shame, and the surgical ICU dilemma. J Am Coll Surg 194:665–673
Nuland SB (2001) A surgeon’s reflections on the care of the dying. Surg Oncol Clin N Am 10:1–5
Cintron A, Hamel MB, Davis RB et al (2003) Hospitalization of hospice patients with cancer. J Palliat Med 6:757–768
Kwok AC, Semel ME, Lipsitz SR et al (2011) The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet 378:1408–1413
McCahill LE, Smith DD, Borneman T et al (2003) A prospective evaluation of palliative outcomes for surgery of advanced malignancies. Ann Surg Oncol 10:654–663
Badgwell BD, Smith K, Liu P et al (2009) Indicators of surgery and survival in oncology inpatients requiring surgical evaluation for palliation. Support Care Cancer 17:727–734
Jones OM, John SK, Horseman N et al (2007) Cause and place of death in patients dying with colorectal cancer. Colorectal Dis 9:253–257
Mosca PJ, Blazer DG 3rd, Wheeler JL (2011) When a chance to cut is not a chance to cure: a future for palliative surgery? Ann Surg Oncol 18:3235–3239
Guest RS, Baser R, Li Y et al (2011) Cancer surgeons’ distress and well-being. II: modifiable factors and the potential for organizational interventions. Ann Surg Oncol 18:1236–1242
Campbell DA Jr, Sonnad SS, Eckhauser FE et al (2001) Burnout among American surgeons. Surgery 130:696–702
Benson S, Sammour T, Neuhaus SJ et al (2009) Burnout in Australasian younger fellows. ANZ J Surg 79:590–597
Shanafelt TD, Balch CM, Bechamps G et al (2010) Burnout and medical errors among American surgeons. Ann Surg 251:995–1000
Shanafelt TD, Balch CM, Dyrbye L et al (2011) Special report: suicidal ideation among American surgeons. Arch Surg 146:54–62
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3:77–101
Tracy SJ (2010) Qualitative quality: eight “big-tent” criteria for excellent qualitative research. Qual Inq 16:837–851
QSR International (2008) NVivo 8 [computer software]. QSR International, Doncaster
Shanafelt T (2008) A career in surgical oncology: finding meaning, balance, and personal satisfaction. Ann Surg Oncol 15:400–406
Page DW (2003) Blood, sweat and tears: are surgeons prepared for the challenges of self-reflection? J Palliat Med 6:625–627
Girgis A, Sanson-Fisher RW, McCarthy WH (1997) Communicating with patients: surgeons’ perceptions of their skills and need for training. ANZ J Surg 67:775–780
Burton MV, Parker RW (1997) Psychological aspects of cancer surgery: surgeons’ attitudes and opinions. Psychooncology 6:47–64
Barnett MM (2002) Effect of breaking bad news on patients’ perceptions of doctors. J R Soc Med 95:343–347
McLafferty RB, Williams RG, Lambert AD (2006) Surgeon communication behaviors that lead patients to not recommend the surgeon to family members or friends: analysis and impact. Surgery 140:616–622
Hack TF, Degner LF, Parker PA (2005) The communication goals and needs of cancer patients: a review. Psychooncology 14:831–845
Prigerson HG (1992) Socialization to dying: social determinants of death acknowledgement and treatment among terminally ill geriatric patients. J Health Soc Behav 33:378–395
Trice ED, Prigerson HG (2009) Communication in end-stage cancer: review of the literature and future research. J Health Commun 14(Suppl 1):95–108
Martin DS (1968) The role of the surgeon in the prospect of death from cancer. CA Cancer J Clin 18:264–267
Whitney SN, McCullough LB, Fruge E et al (2008) Beyond breaking bad news: the roles of hope and hopefulness. Cancer 113:442–445
Mack JW, Wolfe J, Cook EF et al (2007) Hope and prognostic disclosure. J Clin Oncol 25:5636–5642
Barclay JS, Blackhall LJ, Tulsky JA (2007) Communication strategies and cultural issues in the delivery of bad news. J Palliat Med 10:958–977
van Vliet L, Francke AL, Tomson S et al (2011) When cure is no option: how explicit and hopeful should information be given? A qualitative study in breast cancer. Patient Educ Couns 90(3):315–322
Hagerty RG, Butow PN, Ellis PM et al (2005) Communicating with realism and hope: incurable cancer patients’ views on the disclosure of prognosis. J Clin Oncol 23:1278–1288
Morse JM (1995) The significance of saturation. Qual Health Res 5:147–149
Acknowledgments
The authors are grateful to all surgeons who agreed to be interviewed for their willingness to participate in the study and recount their personal and professional experiences.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zambrano, S.C., Chur-Hansen, A. & Crawford, G.B. How Do Surgeons Experience and Cope with the Death and Dying of Their Patients? A Qualitative Study in the Context of Life-limiting Illnesses. World J Surg 37, 935–944 (2013). https://doi.org/10.1007/s00268-013-1948-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-1948-2