Abstract
Background
Avoiding mortality is the ultimate goal when managing patients with suspected appendicitis. Previous studies have shown high mortality after negative appendectomy. This national cohort study analyzes short- and long-term mortality after appendectomy in relation to appendectomy diagnosis, age, co-morbidity, surgical method, hospital volume, and time period.
Method
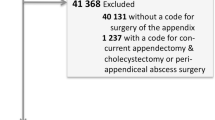
A total of 223,543 appendectomy patients treated from 1987 to 2006 were identified from the Swedish National Patient Register and followed up via the Swedish Cause of Death Register. Analysis of mortality was conducted as Standardized Mortality Ratio (SMR) and by Cox multivariate regression.
Results
Negative appendectomy was followed by a higher mortality in the short term (30-day Standardized Mortality Ratio (SMR30d) 8.95, confidence interval (CI) 6.68–12.61) than after perforated appendicitis (SMR30d 6.39, CI 5.44–7.48), and remained increased for up to 5 years (SMR5yr 1.31, CI 1.16–1.47). Non-perforated appendicitis had a lower than expected long-term mortality (SMR5yr 0.72, CI 0.68–0.76). These differences remained after adjustment for covariates. Laparoscopic appendectomy had similar short-term mortality as open appendectomy but lower than expected long-term morality (SMR5yr 0.70, CI 0.62–0.78). Mortality was decreasing during the study period. Hospital volume had no influence on mortality.
Conclusions
Negative appendectomy is associated with excess short- and long-term mortality that remains after adjustment for known confounders, suggesting an association with underlying undetected morbidity. This motivates an improved preoperative diagnosis to avoid the additional trauma from unnecessary surgical interventions, but further studies are needed to investigate the cause of the increased long-term mortality and if this can be prevented by an improved follow-up of patients with negative appendectomy. Laparoscopic and open appendectomy have similar short-term mortality. The lower long-term mortality after non-perforated appendicitis and laparoscopic appendectomy suggest selection of healthier patients for these interventions. This possibility should be taken into account when comparing mortality after open and laparoscopic appendectomy.
Similar content being viewed by others
References
Velanovich V, Satava R (1992) Balancing the normal appendectomy rate with the perforated appendicitis rate. Implications for quality assurance. Am Surg 58:264–269
Andersson R, Hugander A, Thulin A et al (1992) Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patient and with appendicectomy rate. Eur J Surg 158:37–41
Blomqvist PG, Andersson RE, Granath F et al (2001) Mortality after appendectomy in Sweden, 1987–1996. Ann Surg 233:455–460
Flum DR, Koepsell T (2002) The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg 137:799–804
Faiz O, Clark J, Brown T et al (2008) Traditional and laparoscopic appendectomy in adults. Outcomes in English NHS hospitals between 1996 and 2006. Ann Surg 248:800–806
Andersson MN, Andersson RE (2011) Causes of short-term mortality after appendectomy: a population-based case control study. Ann Surg 254:103–107
Tiwari MM, Reynoso JF, Tsang AW et al (2011) Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg 254:927–932
Guller U, Hervey S, Purves H et al (2004) Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg 239:43–52
Masoomi H, Mills S, Dolich MO et al (2011) Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the nationwide inpatient sample (NIS), 2006–2008. J Gastrointest Surg 15:2226–2231
McMichael AJ (1976) Standardized mortality ratios and the “healthy worker effect”: scratching beneath the surface. J Occup Med 18:165–168
Statistics: Health, Diseases (1998) Causes of death 1996. The National Board of Health and Welfare, Centre for Epidemiology, Stockholm
Andersson R, Hugander A, Thulin A et al (1994) Indications for operation in suspected appendicitis and incidence of perforation. Br Med J 308:107–110
Ludvigsson JF, Andersson E, Ekbom A et al (2011) External review and validation of the Swedish National Inpatient Register. BMC Public Health 11:450
Acknowledgement
This work was supported in part by Futurum—Academy for Healthcare at the Jönköping County Council.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andersson, R.E. Short and Long-Term Mortality After Appendectomy in Sweden 1987 to 2006. Influence of Appendectomy Diagnosis, Sex, Age, Co-morbidity, Surgical Method, Hospital Volume, and Time Period. A National Population-Based Cohort Study. World J Surg 37, 974–981 (2013). https://doi.org/10.1007/s00268-012-1856-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1856-x