Abstract
Purpose
There are many reports about the risk factors for recurrence after lumbar disc surgery.
However, there are none about whether lumbosacral transitional vertebrae (LSTV) are associated with recurrent lumbar disc herniation (LDH). We investigated various risk factors for recurrent LDH after discectomy including LSTV.
Methods
A total of 119 patients who had undergone a discectomy for L4–5 disc herniation were evaluated with a minimum follow-up of two years. Clinical parameters including age, gender, body mass index (BMI), and smoking status, and radiological parameters including type of herniated disc, degree of disc degeneration, LSTV, and sagittal range of motion (SROM) in flexion-extension radiography were evaluated. SROM was measured by the difference of the lordotic angle between the flexion and extension view.
Results
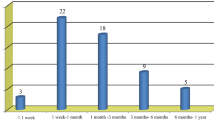
Recurrent disc herniation at L4–5 developed in 21 (17.6%) of the 119 patients. The mean period between primary surgery and recurrence was 17.6 ± 21.1 months. LSTV was found in 11 (52.4%) of the 21 patients who had recurrence and seven (7.1%) of the 98 patients in the non-recurrent group. SROM at L4–5 was 11.68 ± 4.24° in the recurrent group and 9.04 ± 3.65° in the non-recurrent group with a significant difference (p = 0.004). Multiple logistic regression analyses confirmed that LSTV and a larger SROM were significant risk factors for recurrent disc herniation at L4–5.
Conclusions
Lumbosacral transitional vertebrae and a hypermobile disc in flexion-extension radiography were found to be risk factors for recurrent lumbar disc herniation.

Similar content being viewed by others
References
Shin BJ (2014) Risk factors for recurrent lumbar disc herniations. Asian Spine J 8:211–215
Cheng J, Wang H, Zheng W, Li C, Wang J, Zhang Z, Huang B, Zhou Y (2013) Reoperation after lumbar disc surgery in two hundred and seven patients. Int Orthop 37:1511–1517
Suk KS, Lee HM, Moon SH, Kim NH (2001) Recurrent lumbar disc herniation: results of operative management. Spine (Phila Pa 1976) 26:672–676
Cinotti G, Roysam GS, Eisenstein SM, Postacchini F (1998) Ipsilateral recurrent lumbar disc herniation: a prospective, controlled study. J Bone Joint Surg Br 80:825–832
Kim KT, Lee DH, Cho DC, Sung JK, Kim YB (2015) Preoperative risk factors for recurrent lumbar disc herniation in L5-S1. J Spinal Disord Tech 28:E571–E577
Axelsson P, Karlsson BS (2004) Intervertebral mobility in the progressive degenerative process. A radiostereometric analysis. Eur Spine J 13:567–572
Kim KT, Park SW, Kim YB (2008) Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine (Phila Pa 1976) 34:2674–2678
Tang M, Yang XF, Yang SW, Han P, Ma YM, Yu H, Zhu B (2014) Lumbosacral transitional vertebra in a population-based study of 5860 individuals: prevalence and relationship to low back pain. Eur J Radiol 83:1679–1682
Ver Verergauwen S, Parizel PM, Van Breusegem L, Van Goethem JW, Nackaerts Y, Van den Hauwe L, De Schepper AM (1976) Distribution and incidence of degenerative spine changes in patients with a lumbo-sacral transitional vertebra. Eur Spine J 6:168–172
Paajanen H, Erkintalo M, Kuusela T, Dahlstrom S, Kormano M (1989) Magnetic resonance study of disc degeneration in young low-back pain patients. Spine (Phila Pa 1976) 14:982–985
Swartz KR, Trost GR (2003) Recurrent lumbar disc herniation. Neurosurg Focus 15:E10
Castellvi AE, Goldstein LA, Chan DP (1984) Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 9:493–495
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878
Bertolotti M (1917) Contribution to the knowledge of the defects as it relates to regional differences in the spine with regards to the as simulation of L5 and the sacrum. Radiol Med 4:113–114
Quinlan JF, Duke D, Eustace S (2006) Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br 88:1183–1186
Otani K, Konno S, Kikuchi S (2001) Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Joint Surg Br 83:1137–1140
Hashimoto M, Watanabe O, Hirano H (1996) Extraforaminal stenosis in the lumbosacral spine. Efficacy of MR imaging in the coronal plane. Acta Radiol 37:610–613
Wiltse LL, Guyer RD, Spencer CW, Glenn WV, Porter IS (1984) Alar transverse process impingement of the L5 spinal nerve: the far-out syndrome. Spine (Phila Pa 1976) 9:31–41
Elster AD (1989) Bertolotti’s syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976) 14:1373–1377
Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimaki H (2004) Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine (Phila Pa 1976) 29:200–205
Taskaynatan MA, Izci Y, Ozgul A, Hazneci B, Dursun H, Kalyon TA (2005) Clinical significance of congenital lumbosacral malformations in young male population with prolonged low back pain. Spine (Phila Pa 1976) 30:E210–E213
Bron JL, van Royen BJ, Wuisman PI (2007) The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg 73:687–695
Chang X, Chen B, Li HY, Han XB, Zhou Y, Li CQ (2014) The safety and efficacy of minimally invasive discectomy: a meta-analysis of prospective randomized controlled trials. Int Orthop 38:1225–1234
Du J, Tang X, Jing X, Li N, Wang Y, Zhang X (2016) Outcomes of percutaneous endoscopic lumbar discectomy via a translaminar approach, especially for soft, highly down-migrated lumbar disc herniation. Int Orthop 40:1247–1252
Fan G, Han R, Gu X, Zhang H, Guan X, Fan Y, Wang T, He S (2017) Navigation improves the learning curve of transforamimal percutaneous endoscopic lumbar discectomy. Int Orthop 41:323–332
Funding
This work was supported by an INHA University Research Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shin, EH., Cho, KJ., Kim, YT. et al. Risk factors for recurrent lumbar disc herniation after discectomy. International Orthopaedics (SICOT) 43, 963–967 (2019). https://doi.org/10.1007/s00264-018-4201-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4201-7