Abstract
Introduction
To evaluate the five year clinical and radiographic outcome of unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation for cervical compressive myelopathy.
Methods
From August 2009 to June 2010, 56 patients with cervical compressive myelopathy underwent unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation with a mean age of 64.8 years. Clinical results were investigated including Japanese Orthopedic Association (JOA) scores, Neck Dysfunction Index (NDI), occurrences of complications and neurological deterioration. Radiographic results including cervical alignments, cervical range of motion (ROM), spinal canal enlargement and spinal cord decompression were assessed on X-ray, three-dimensional CT and MRI.
Results
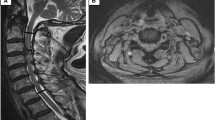
The mean follow-up period was 59.2 months (range 53∼64 months), and all patients achieved osseous fusion at hinge side at an average of 6.8 months after operation. The average cost from admission to discharge is $9817.9. Compared to previous all-level fixation, the cost decreased nearly 40 %. During the follow-up, all patients showed a significant improvement in the JOA score and NDI score. A 23.2 % incidence of axial neck pain were also observed; Significant enlargement of the spinal canal and spinal cord drift was achieved and well maintained, overall cervical ROM decreased by 27.1 % (mean 12.9° loss) at the final follow-up and cervical lordosis decreased slightly in all patients without statistic difference. No instrumentation failure or lamina reclosure was observed in our study. Comparing mini-plate segments and suture segments, the mean AP diameter and Pavlov’s ratio at the final follow-up showed no statistic difference, only open angle at the final follow-up showed significant decrease.
Conclusions
Unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation is a safe, effective and economical surgical method for cervical compressive myelopathy and the five year result is satisfactory.






Similar content being viewed by others
References
Jiang JL, Li XL, Zhou XG, Lin H, Dong J (2012) Plate-only open-door laminoplasty with fusion for treatment of multilevel degenerative cervical disease. J Clin Neurosci 19(6):804–809
Suri A, Chabbra RP, Mehta VS, Gaikwad S, Pandey RM (2003) Effect of intramedullary signal changes on the surgical outcome of patients with cervical spondylotic myelopathy. Spine J 3(1):33–45
Chiba K, Ogawa Y, Ishii K et al (2006) Long-term results of expansive open-door laminoplasty for cervical myelopathy-average 14-year follow-up study. Spine 31(26):2998–3005
Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y (1983) Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 8(7):693–699
Hyun SJ, Rhim SC, Roh SW, Kang SH, Riew KD (2009) The time course of range of motion loss after cervical laminoplasty: a prospective study with minimum two-year follow-up. Spine 34(11):1134–1139
Tanaka N, Nakanishi K, Fujimoto Y et al (2008) Expansive laminoplasty for cervical myelopathy with interconnected porous calcium hydroxyapatite ceramic spacers: comparison with autogenous bone spacers. J Spinal Disord Tech 21(8):547–552
Yu HL, Xiang LB, Liu J, Chen Y, Yu M, Cao Y (2010) Laminoplasty using Twinfix suture anchors to maintain cervical canal expansion. Eur Spine J 19(10):1795–1798
Ono A, Yokoyama T, Numasawa T, Wada K, Toh S (2007) Dural damage due to a loosened hydroxyapatite intraspinous spacer after spinous process-splitting laminoplasty. Report of two cases. J Neurosurg Spine 7(2):230–235
Kanemura A, Doita M, Iguchi T, Kasahara K, Kurosaka M, Sumi M (2008) Delayed dural laceration by hydroxyapatite spacer causing tetraparesis following double-door laminoplasty. J Neurosurg Spine 8(2):121–128
Rhee JM, Register B, Hamasaki T, Franklin B (2010) Plate-only open door laminoplasty maintains stable spinal canal expansion with high rates of hinge union and no plate failures. Spine 36(1):9–14
Jiang LJ, Chen WS, Chen Q, Xu K, Wu Q, Li F (2012) Clinical application of a new plate fixation system in open-door laminoplasty. Orthopedics 35(2):225–231
Matsuzaki H, Hoshino M, Kiuchi T, Toriyama S (1989) Expansive laminoplasty for the second cervical vertebra. Spine 14(11):1198–1203
Takeshita K, Murakami M, Kobayashi A, Nakamura C (2001) Relationship between cervical curvature index (Ishihara) and cervical spine angle (C2—7). J Orthop Sci 6(3):223–226
Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K (2002) Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg 96(2 Suppl):180–189
Kawaguchi Y, Kanamori M, Ishihara H et al (2003) Minimum 10-year follow-up after an bloc cervical laminoplasty. Clin Orthop 411:129–139
Wang HQ, Mak KC, Samartzis D et al (2011) “Spring-back” closure associated with open-door cervical laminoplasty. Spine J 11(9):832–838
Lee DH, Park SA, Kim NH et al (2011) Laminar closure after classic Hirabayashi open-door Laminoplasty. Spine 36(25):1634–1640
Seichi A, Hoshino Y, Kimura A et al (2011) Neurological complications of cervical laminoplasty for patients with ossification of the posterior longitudinal ligament-a multi-institutional retrospective study. Spine 36(15):998–1003
Satomi K, Nishu Y, Kohno T, Hirabayashi K (1994) Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine 19(5):507–510
Cheng Z, Chen W, Yan S, Li W, Qian S (2015) Expansive open-door cervical laminoplasty: in situ reconstruction of extensor muscle insertion on the C2 spinous process combined with titanium miniplates internal fixation. Medicine 94(28):1–6
Hosono N, Yonenobu K, Ono K (1996) Neck and shoulder pain after laminoplasty. A noticeable complication. Spine 21(17):1969–1973
Wang ZF, Chen GD, Xue F, Sheng XW, Yang HL, Qian J (2014) All levels versus alternate levels plate fixation in expansive open door cervical laminoplasty. Indian J Orthop 48(6):582–586
Acknowledgments
We wish to thank all those who generously agreed to be interviewed for this research.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Ln., Wang, L., Song, Ym. et al. Clinical and radiographic outcome of unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation for cervical compressive myelopathy: a five-year follow-up study. International Orthopaedics (SICOT) 40, 1267–1274 (2016). https://doi.org/10.1007/s00264-016-3194-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3194-3