Abstract
Background
Recurrent glioblastoma is associated with a poor overall survival. Antiangiogenic therapy results in a high tumor response rate but has limited impact on survival. Immunotherapy has emerged as an efficient treatment modality for some cancers, and preclinical evidence indicates that anti-VEGF(R) therapy can counterbalance the immunosuppressive tumor microenvironment.
Methods
We collected peripheral blood mononuclear cells (PBMC) of patients with recurrent glioblastoma treated in a randomized phase II clinical trial comparing the effect of axitinib with axitinib plus lomustine and analyzed the immunophenotype of PBMC, the production of cytokines and expression of inhibitory molecules by circulating T cells.
Results
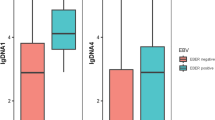
PBMC of 18 patients were collected at baseline and at 6 weeks after initiation of study treatment. Axitinib increased the number of naïve CD8+ T cells and central memory CD4+ and CD8+ T cells and reduced the TIM3 expression on CD4+ and CD8+ T cells. Patients diagnosed with progressive disease on axitinib had a significantly increased number of regulatory T cells and an increased level of PD-1 expression on CD4+ and CD8+ T cells. In addition, reduced numbers of cytokine-producing T cells were found in progressive patients as compared to patients responding to treatment.
Conclusion
Our results suggest that axitinib treatment in patients with recurrent glioblastoma has a favorable impact on immune function. At the time of acquired resistance to axitinib, we documented further enhancement of a preexisting immunosuppression. Further investigations on the role of axitinib as potential combination partner with immunotherapy are necessary.






Similar content being viewed by others
Abbreviations
- 6mPFS:
-
6-Month progression-free survival
- CR:
-
Complete response
- EGFRvIII:
-
Endothelial growth factor receptor variant III
- GBM:
-
Glioblastoma
- LAG3:
-
Lymphocyte-activation gene 3
- ORR:
-
Objective response rate
- PD:
-
Progressive disease
- PDGFR:
-
Platelet-derived growth factor receptor
- PR:
-
Partial response
- SD:
-
Stable disease
- TCM :
-
Central memory T cells
- TEM :
-
Effector memory T cells
- TIM3:
-
T cell immunoglobulin domain and mucin domain 3
- TKI:
-
Tyrosine kinase inhibitor
- Treg :
-
Regulatory T cells
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
References
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Lamborn KR, Chang SM, Prados MD (2004) Prognostic factors for survival of patients with glioblastoma: recursive partitioning analysis. Neuro Oncol 6:227–235
Friedman HS, Prados MD, Wen PY et al (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27:4733–4740
Stupp R, Hegi ME, Gorlia T et al (2014) Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071-22072 study): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol 15:1100–1108
Hutterer M, Nowosielski M, Haybaeck J et al (2014) A single-arm phase II Austrian/German multicenter trial on continuous daily sunitinib in primary glioblastoma at first recurrence (SURGE 01-07). Neuro Oncol 16:92–102
Lee EQ, Kuhn J, Lamborn KR et al (2012) Phase I/II study of sorafenib in combination with temsirolimus for recurrent glioblastoma or gliosarcoma: North American Brain Tumor Consortium study 05-02. Neuro Oncol 14:1511–1518
Batchelor TT, Mulholland P, Neyns B et al (2013) Phase III randomized trial comparing the efficacy of cediranib as monotherapy, and in combination with lomustine, versus lomustine alone in patients with recurrent glioblastoma. J Clin Oncol 31:3212–3218
Neyns B, Duerinck J, Du Four S et al (2014) Randomized phase II study of axitinib versus standard of care in patients with recurrent glioblastoma. ASCO Meet Abstr 32:2018
Duerinck J, Du Four S, Bouttens F, Neyns B (2016) Randomized phase II study of axitinib versus physicians best alternative choice of therapy in patients with recurrent glioblastoma. J Neurooncol. doi:10.1007/s11060-016-2092-2
Taal W, Oosterkamp HM, Walenkamp AME et al (2014) Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (BELOB trial): a randomised controlled phase 2 trial. Lancet Oncol 15:943–953
Huang Y, Goel S, Duda DG et al (2013) Vascular normalization as an emerging strategy to enhance cancer immunotherapy. Cancer Res 73:2943–2948
Du Four S, Maenhout SK, De Pierre K et al (2015) Axitinib increases the infiltration of immune cells and reduces the suppressive capacity of monocytic MDSCs in an intracranial mouse melanoma model. Oncoimmunology 4:e998107. doi:10.1080/2162402X.2014.998107
Jackson CM, Lim M, Drake CG (2014) Immunotherapy for brain cancer: recent progress and future promise. Clin Cancer Res 20:3651–3659. doi:10.1158/1078-0432.CCR-13-2057
Reardon DA, Schuster J, Tran DD et al (2015) ReACT: overall survival from a randomized phase II study of rindopepimut (CDX-110) plus bevacizumab in relapsed glioblastoma. ASCO Meet Abstr 33:2009
Chung AS, Wu X, Zhuang G et al (2013) An interleukin-17-mediated paracrine network promotes tumor resistance to anti-angiogenic therapy. Nat Med 19:1114–1123
Doloff JC, Waxman DJ (2012) VEGF receptor inhibitors block the ability of metronomically dosed cyclophosphamide to activate innate immunity-induced tumor regression. Cancer Res 72:1103–1115
Stehle F, Schulz K, Fahldieck C et al (2013) Reduced immunosuppressive properties of axitinib in comparison with other tyrosine kinase inhibitors. J Biol Chem 288:16334–16347
Gattinoni L, Klebanoff CA, Palmer DC et al (2005) Acquisition of full effector function in vitro paradoxically impairs the in vivo antitumor efficacy of adoptively transferred CD8 + T cells. J Clin Invest 115:1616–1626
Klebanoff Christopher, Gattoni Luca, Restifo N (2012) Sorting through subsets: which T cell populations mediate highly effective adoptive immunotherapy? J Immunother 35:651–660
Fourcade J, Sun Z, Pagliano O et al (2012) CD8 + T cells specific for tumor antigens can be rendered dysfunctional by the tumor microenvironment through upregulation of the inhibitory receptors BTLA and PD-1. Cancer Res 72:887–896
Fourcade J, Sun Z, Pagliano O et al (2014) PD-1 and Tim-3 regulate the expansion of tumor antigen-specific CD8 + T cells induced by melanoma vaccines. Cancer Res 74:1045–1055
Clary S, Nagarkatti PS, Nagarkatti M (1990) Immunomodulatory effects of nitrosoureas on the phenotype and functions of T cells in the thymus and periphery. Immunopharmacology 20:153–164
Nguyen LT, Ohashi PS (2015) Clinical blockade of PD1 and LAG3—potential mechanisms of action. Nat Rev Immunol 15:45–56. doi:10.1038/nri3790
Goldberg MV, Drake CG (2011) LAG-3 in cancer immunotherapy. Curr Top Microbiol Immunol 344:269–278
Wei B, Wang L, Zhao X et al (2014) The upregulation of programmed death 1 on peripheral blood T cells of glioma is correlated with disease progression. Tumor Biol 35:2923–2929
Ozao-Choy J, Ma G, Kao J et al (2009) The novel role of Tyrosine Kinase inhibitor in the reversal of immune suppression and modulation of tumor microenvironment for immune-based cancer therapies. Cancer Res 69:2514–2522
Chen ML, Yan BS, Lu WC et al (2014) Sorafenib relieves cell-intrinsic and cell-extrinsic inhibitions of effector T cells in tumor microenvironment to augment antitumor immunity. Int J Cancer 134:319–331
Guislain A, Gadiot J, Kaiser A et al (2015) Sunitinib pretreatment improves tumor—infiltrating lymphocyte expansion by reduction in intratumoral content of myeloid—derived suppressor cells in human renal cell carcinoma. Cancer Immunol Immunother 64:1241–1250
Curiel TJ, Coukos G, Zou L et al (2004) Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 10:942–949
Choi BD, Fecci PE, Sampson JH (2012) Regulatory T cells move in when gliomas say “I DO”. Clin Cancer Res 18:6086–6088
Fecci PE, Mitchell DA, Whitesides JF et al (2006) Increased regulatory T-cell fraction amidst a diminished CD4 compartment explains cellular immune defects in patients with malignant glioma. Cancer Res 66:3294–3302
Thomas AA, Fisher JL, Rahme GJ et al (2015) Regulatory T cells are not a strong predictor of survival for patients with glioblastoma. Neuro Oncol 17:801–809
Wainwright DA, Chang AL, Dey M et al (2014) Durable therapeutic efficacy utilizing combinatorial blockade against IDO, CTLA-4, and PD-L1 in mice with brain tumors. Clin Cancer Res 20:5290–5301
Motz GT, Santoro SP, Wang L-P et al (2014) Tumor endothelium FasL establishes a selective immune barrier promoting tolerance in tumors. Nat Med 20:607–615
Batchelor TT, Reardon DA, de Groot JF et al (2014) Antiangiogenic therapy for glioblastoma: current status and future prospects. Clin Cancer Res 20:5612–5619
Franchimont D (2004) Overview of the actions of glucocorticoids on the immune response: a good model to characterize new pathways of immunosuppression for new treatment strategies. Ann N Y Acad Sci 1024:124–137
Acknowledgments
We would like to acknowledge the patients who consented to participate in this study, their families, and Pfizer Belgium for the provision of axitinib and a research grant for conducting the clinical trial. We would also like to thank the data manager Katrien Van den Bossche and Kathleen Mooren from the University Hospital Brussels (Universitair Ziekenhuis Brussel, UZ Brussel) for their help with the data collection, and Ludwig Van den Hove, PhD, Pfizer Belgium, for his support and critical review of the manuscript. Sarah K Maenhout and Stephanie Du Four are funded by a PhD grant from the Agency for Innovation by Science and Technology in Flanders (IWT). Brenda De Keersmaecker is funded by a research grant Emmanuel van der Schueren from the Flemish League against Cancer (Vlaamse Liga Tegen Kanker, VLK). This work is supported by a grant from the Research Foundation Flanders [Fonds voor Wetenschappelijk Onderzoek (FWO, G023411 N)] to Kris Thielemans and Joeri L Aerts. The FACSAria III cell sorter and the LSR Fortessa were purchased with support from the Hercules Foundation to Kris Thielemans and Joeri L Aerts (Grant UABR/09/002) and the Foundation against Cancer (Stichting Tegen Kanker), respectively. The clinical study was supported by a research grant from Pfizer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Du Four, S., Maenhout, S.K., Benteyn, D. et al. Disease progression in recurrent glioblastoma patients treated with the VEGFR inhibitor axitinib is associated with increased regulatory T cell numbers and T cell exhaustion. Cancer Immunol Immunother 65, 727–740 (2016). https://doi.org/10.1007/s00262-016-1836-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-016-1836-3