Abstract
Purpose
To determine whether the diameter of intrahepatic and extrahepatic bile ducts and pancreatic ducts in patients on methadone maintenance therapy is increased when compared with control subjects.
Methods
Between January 1, 2000 and March 15, 2013, a total of 97 patients (mean age 49.9, range 22–79, 65 male, 32 female) were identified who were receiving chronic methadone maintenance therapy (MMT) when they underwent imaging with abdominal MRI or a contrast-enhanced abdominopelvic CT. A group of 97 consecutive non-MMT control patients (mean age 51.4, range 21–86, 45 male, 52 female) who underwent imaging with abdominal MRI or contrast-enhanced abdominopelvic CT were identified. Patients with known pancreaticobiliary pathology that may confound biliary ductal measurements were excluded. Blinded interpretation was performed, documenting the diameters of the intrahepatic and extrahepatic bile ducts and pancreatic ducts. Descriptive statistics were performed.
Results
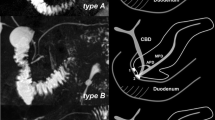
Patients on MMT demonstrated increased bile duct diameter, with an average increase in duct diameter of 2.39 mm for the common bile duct (p < 0.001; 95% CI 1.88–2.90 mm), 1.43 mm for the intrahepatic bile ducts (p < 0.001; 95% CI 1.12–1.74 mm), and 0.90 mm for the pancreatic duct (p < 0.001; 95% CI 0.64–1.16 mm). No statistically significant correlation was found between ductal diameters and the daily dose of methadone.
Conclusion
Patients on methadone maintenance therapy demonstrate significantly increased intra- and extrahepatic bile duct and pancreatic duct diameter when compared with controls. There was no correlation between the dose of methadone and ductal diameter.




Similar content being viewed by others
References
Benjaminov F, Leichtman G, Naftali T, Half EE, Konikoff FM (2013) Effects of age and cholecystectomy on common bile duct diameter as measured by endoscopic ultrasonography. Surg Endosc 27(1):303–307.
Daradkeh S, Tarawneh E, Al-Hadidy A (2005) Factors affecting common bile duct diameter. Hepatogastroenterology. 52(66):1659–1661.
Results from the 2010 National survey on drug use and health: summary of national findings. (2011) Rockville, MD: Substance Abuse and Mental Health Services Administration.
Kolodny A, Courtwright DT, Hwang CS, et al. (2015) The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health 36:559–574.
Zylberberg H, Fontaine H, Correas JM, et al. (2000) Dilated bile duct in patients receiving narcotic substitution: an early report. J Clin Gastroenterol 31(2):159–161.
Hsiao CY, Chen KC, Lee LT, et al. (2015) The reductions in monetary cost and gains in productivity with methadone maintenance treatment: one year follow-up. Psychiatry Res 225(3):673–679.
Sharma SS (2002) Sphincter of Oddi dysfunction in patients addicted to opium: an unrecognized entity. Gastrointest Endosc 55(3):427–430.
Firoozi B, Choung R, Diehl DL (2003) Bile duct dilation with chronic methadone use in asymptomatic patients: ERCP findings in 6 patients. Gastrointest Endosc 58(1):127–130.
Leopold SJ, Grady BP, Lindenburg CE, et al. (2014) Common bile duct dilatation in drug users with chronic hepatitis C is associated with current methadone use. J Addict Med 8(1):53–58.
Zahedi-Nejad N, Narouei S, Fahimy F (2010) Common bile duct (CBD) diameter in opium-addicted men: comparison with non-addict controls. Pol J Radiol 75(3):20–24.
Dedrick DF, Tanner WW, Bushkin FL (1980) Common bile duct pressure during enflurane anesthesia. Effects of morphine and subsequent naloxone. Arch Surg 115(7):820–822.
Radnay PA, Duncalf D, Novakovic M, Lesser ML (1984) Common bile duct pressure changes after fentanyl, morphine, meperidine, butorphanol, and naloxone. Anesth Analg 63(4):441–444.
Krishnamurthy S, Krishnamurthy GT (1996) Cholecystokinin and morphine pharmacological intervention during 99mTc-HIDA cholescintigraphy: a rational approach. Semin Nucl Med 26(1):16–24.
Agrawal MD, Mennitt KW, Zhang H, et al. (2014) Morphine three-dimensional T1 gadoxetate MR cholangiography of potential living related liver donors. J Magn Reson Imaging 39(3):584–589.
Agarwal S, Nag P, Sikora S, et al. (2006) Fentanyl-augmented MRCP. Abdom Imaging 31(5):582–587.
Mo YH, Liang PC, Ho MC, et al. (2009) Morphine- and glucagon-augmented magnetic resonance cholangiopancreatography to evaluate living liver donors. Liver Transpl 15(9):1021–1027.
Kropil P, Erhardt A, Mehnert S, et al. (2010) Image quality and bile duct volumetry in MR cholangiopancreatography augmented with low-dose morphine. AJR Am J Roentgenol 194(2):W171–W175.
Edge MD, Hoteit M, Patel AP, et al. (2007) Clinical significance of main pancreatic duct dilation on computed tomography: single and double duct dilation. World J Gastroenterol 13(11):1701–1705.
Meng Z, Xu YK, Zhang YP (2008) Magnetic resonance cholangiopancreatography of pancreaticobiliary duct dilation due to pancreatic carcinoma and chronic pancreatitis. Nan Fang Yi Ke Da Xue Xue Bao 28(1):113–115.
Sharma SS, Ram S, Maharshi S, et al. (2013) Pancreato-biliary endoscopic ultrasound in opium addicts presenting with abdominal pain. Endosc Ultrasound 2(4):204–207.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None of the authors have any relevant disclosures related to potential conflicts of interest.
Ethical Approval
The institutional review board approved this Health Insurance Portability and Accountability Act (HIPPA)-compliant retrospective study.
Informed consent
The requirement for informed consent was waived.
Rights and permissions
About this article
Cite this article
Bates, D.D.B., Tamayo-Murillo, D., Kussman, S. et al. Biliary and pancreatic ductal dilation in patients on methadone maintenance therapy. Abdom Radiol 42, 884–889 (2017). https://doi.org/10.1007/s00261-016-0946-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0946-x