Abstract
Purpose
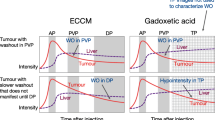
To evaluate Gd-EOB-DTPA-enhanced magnetic resonance (MR) performance during dynamic (DYN) phases, hepatobiliary (HB) phase and diffusion-weighted imaging (DWI) compared with pathological findings in patients undergoing orthotopic liver transplantation (OLT) for hepatocellular carcinoma (HCC) associated with different conditions, such as stage of chronic liver disease, histological grading, nodule size, and occurrence of previous treatments.
Methods
Retrospective analysis of 64 nodules reported as HCC at pathological analysis on 28 explanted livers, examined about 3 months before OLT using a 1.5 T device and 16 channels array after intravenous GD-EOB-DTPA injection. Lesions features and hepatic functional values were recorded for each patient. Two radiologists performed in consensus the analysis of nodules on DYN, HB, and DWI. MR findings were compared with those of pathological anatomy. Diagnostic indicators were calculated for each technique.
Results
DYN and HB showed no statistically significant difference in sensitivity (88% and 98%, respectively), diagnostic accuracy (90.6% and 99.9%), and specificity (both 100%), for all Child-Pugh scores, gradings, sizes, and presence or absence of previous treatments. DWI had a statistically significant lower sensitivity compared to DYN (p = 0.001) and HB (p < 0.0001); its sensitivity was significantly inferior for Child-Pugh Class B nodules than for Child-Pugh Class A ones (p = 0.00005). DWI sensitivity presented a significant increase (p = 0.03) with grading and presence of previous treatments (p = 0.0006). ADC values showed no statistically significant changes with Child-Pugh score, grading and nodules size; statistically significant increase was instead found for treated vs. untreated nodules (p = 0.016).
Conclusions
In a multiparametric HCC MRI assessment, DYN and HB play the leading role, with DWI faring acceptably well for Child-Pugh Class A nodules and treated ones.






Similar content being viewed by others
References
Parkin DM, Bray F, Ferlay J, et al. (2005) Global cancer statistics, 2002. CA Cancer J Clin 55(2):74–108
Stigliano R, Marelli L, Yu D, et al. (2007) Seeding following percutaneous diagnostic and therapeutic approaches for hepatocellular carcinoma. What is the risk and the outcome? Seeding risk for percutaneous approach of HCC. Cancer Treat Rev 33:437–447
Atwell TD, Smith RL, Hesley GK, et al. (2010) Incidence of bleeding after 15,181 percutaneous biopsies and the role of aspirin. AJR Am J Roentgenol 194(3):784–789
Bruix J, Sherman M (2011) American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
Zech CJ, Bartolozzi C, Sage PB, et al. (2013) Consensus report of the Fifth International Forum for Liver MRI. AJR Am J Roentgenol 201:97–107
Jang H-J, Kim TK, Burns PN, et al. (2007) Enhancement patterns of hepatocellular carcinoma at contrast-enhanced US: comparison with histologic differentiation. Radiology 244:898–906
Bolondi L, Gaiani S, Celli N, et al. (2005) Characterization of small nodules in cirrhosis by assessment of vascularity: the problem of hypovascular hepatocellular carcinoma. Hepatology 42:27–34
Huppertz A, Balzer T, Blakeborough A, et al. (2004) Improved detection of focal liver lesions at MR imaging: multicenter comparison of gadoxetic acid-enhanced MR images with intraoperative findings. Radiology 230:266–275
Golfieri R, Grazioli L, Orlando E, et al. (2012) Which is the best MRI marker of malignancy for atypical cirrhotic nodules: hypointensity in hepatobiliary phase alone or combined with other features? Classification after Gd-EOB-DTPA administration. J Magn Reson Imaging 36:648–657
Ahn SS, Mj Kim, Lim SJ, et al. (2010) Added value of gadoxetic acid-enhanced hepatobiliary phase MR imaging in the diagnosis of hepatocellular carcinoma. Radiology 255:459–466
Haradome H, Grazioli L, Tinti R, et al. (2011) Additional value of gadoxetic acid-DTPA-enhanced hepatobiliary phase MR imaging in the diagnosis of early-stage hepatocellular carcinoma: comparison with dynamic triple-phase multidetector CT imaging. J Magn Reson Imaging 34:69–78
Taouli B, Koh DM (2010) Diffusion-weighted MR imaging of the liver. Radiology 254:47–66
Parikh T, Drew SJ, Lee VS, et al. (2008) Focal liver lesion detection and characterization with diffusion-weighted MR imaging: comparison with standard breath-hold T2-weighted imaging. Radiology 246:812–822
Bruegel M, Gaa J, Waldt S, et al. (2008) Diagnosis of hepatic metastasis: comparison of respiration-triggered diffusion-weighted echo-planar MRI and five t2-weighted turbo spin-echo sequences. AJR Am J Roentgenol 191:1421–1429
Kele PG, van der Jagt EJ (2010) Diffusion weighted imaging in the liver. World J Gastroenterol 16:1567–1576
Parente DB, Perez RM, Eiras-Araujo A, et al. (2012) MR imaging of hypervascular lesions in the cirrhotic liver: a diagnostic dilemma. Radiographics 32:767–787
Yuan Z, Ye X-D, Dong S, et al. (2010) Role of magnetic resonance diffusion-weighted imaging in evaluating response after chemoembolization of hepatocellular carcinoma. Eur J Radiol 75(1):e9–e14
Mazzaferro V, Bhoori S, Sposito C, et al. (2011) Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transplant 17(Suppl 2):S44–S57
European Association for the Study of the Liver, European Organisation for Research and Treatment of Cancer (2012) EASL–EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56(4):908–943
Bartolozzi C, Battaglia V, Bargellini I, et al. (2013) Contrast-enhanced magnetic resonance imaging of 102 nodules in cirrhosis: correlation with histological findings on explanted livers. Abdom Imaging 38:290–296
Park MJ, Kim YK, Lee MW, et al. (2012) Small hepatocellular carcinomas: improved sensitivity by combining gadoxetic acid-enhanced and diffusion-weighted MR imaging patterns. Radiology 264:761–770
Goshima Kanematsu M, Kondo H, et al. (2008) Evaluating local hepatocellular carcinoma recurrence post-transcatheter arterial chemoembolization: is diffusion-weighted MRI reliable as an indicator? J Magn Reson Imaging 27:834–839
Nasu K, Kuroki Y, Tsukamoto T, et al. (2009) Diffusion-weighted imaging of surgically resected hepatocellular carcinoma: imaging characteristics and relationship among signal intensity, apparent diffusion coefficient and histopathologic grade. AJR Am J Roentgenol 193:438–444
Chen CY, Li CW, Kuo YT, et al. (2006) Early response of hepatocellular carcinoma to transcatheter arterial chemoembolization: choline levels and MR diffusion constants–initial experience. Radiology 239:448–456
Nakanishi M, Chuma M, Hige S, et al. (2012) Relationship between diffusion-weighted magnetic resonance imaging and histological tumor grading of hepatocellular carcinoma. Ann Surg Oncol 19:1302–1309
Saborido PB, Diaz JCM, de los Galanes SJ, et al. (2005) Does preoperative fine needle aspiration-biopsy produce tumor recurrence in patients following liver transplantation for hepatocellular carcinoma? Transplant Proc 37:3874–3877
Caturelli E, Solmi L, Anti M (2004) Ultrasound guided fine needle biopsy of early hepatocellular carcinoma complicating liver cirrhosis: a multicentre study. Gut 53:1356–1362
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faletti, R., Cassinis, M.C., Fonio, P. et al. Multiparametric Gd-EOB-DTPA magnetic resonance in diagnosis of HCC: dynamic study, hepatobiliary phase, and diffusion-weighted imaging compared to histology after orthotopic liver transplantation. Abdom Imaging 40, 46–55 (2015). https://doi.org/10.1007/s00261-014-0180-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0180-3