Abstract
Purpose
To assess the additional value of secretin-enhanced MRCP (SMRCP) over conventional MRCP in diagnosing divisum.
Methods
Retrospective HIPAA-compliant and IRB-approved review found 140 patients with SMRCP and ERCP correlation within 6 months of each other. All studies were anonymized and the SMRCP images (SMRCP image set) were separated from 2D and 3D MRCP and axial and coronal T2-weighted images (conventional MRI image set). Each image set on each patient was assigned different and randomized case numbers. Two reviewers (R1 and R2) independently reviewed the image sets for divisum vs. no divisum, complete divisum vs. incomplete divisum, and the certainty of diagnosis (1 = definitely certain, 2 = moderately certain, and 3 = unsure). ERCP findings were taken as gold standard.
Results
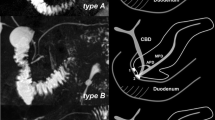
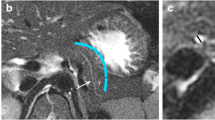
There was no difference in age and gender between the divisum (n = 97, with 13 incomplete divisum) and no divisum (n = 43) groups. In diagnosing divisum anatomy, the sensitivity was higher for SMRCP compared to conventional MRI for R1 (84.5 vs. 72.2, p = 0.02) but not R2 (89.7 vs. 84.4, p = 0.25). The specificity was higher in SMRCP image set compared to conventional MRI (R1: 88.1 vs. 76.2, p = 0.01; R2: 81.4 vs. 65.1, p < 0.001). The mean area under ROC curve was higher for SMRCP image set (R1: 0.86 vs. 0.74, p = 0.01; R2: 0.87 vs. 0.74, p = 0.01). The certainty of diagnosis was higher in SMRCP image set compared to conventional MRI (p = 0.02 for both reviewers). SMRCP was not found to be superior in distinguishing incomplete from complete divisum. The main reasons for erroneous SMRCP diagnosis were the presence of an ansa loop in the main duct and ductal strictures due to chronic pancreatitis.
Conclusion
Even though the reviewers had more sequences (axial and coronal) to evaluate in the non-secretin image set, there was some improvement in diagnosing divisum with SMRCP.







Similar content being viewed by others
References
Fischer M, Hassan A, Sipe BW, et al. (2010) Endoscopic retrograde cholangiopancreatography and manometry findings in 1,241 idiopathic pancreatitis patients. Pancreatology 10(4):444–452
Takuma K, Kamisawa T, Tabata T, Egawa N, Igarashi Y (2010) Pancreatic diseases associated with pancreas divisum. Dig Surg 27(2):144–148
Gonoi W, Akai H, Hagiwara K, et al. (2011) Pancreas divisum as a predisposing factor for chronic and recurrent idiopathic pancreatitis: initial in vivo survey. Gut 60(8):1103–1108
Cotton PB (1980) Congenital anomaly of pancreas divisum as cause of obstructive pain and pancreatitis. Gut 21(2):105–114
Gregg JA (1977) Pancreas divisum: its association with pancreatitis. Am J Surg 134(5):539–543.
Satterfield ST, McCarthy JH, Geenen JE, et al. (1988) Clinical experience in 82 patients with pancreas divisum: preliminary results of manometry and endoscopic therapy. Pancreas 3(3):248–253.
Bertin C, Pelletier AL, Vullierme MP, et al. (2012) Pancreas divisum is not a cause of pancreatitis by itself but acts as a partner of genetic mutations. Am J Gastroenterol 107(2):311–317.
Cavestro GM, Zuppardo RA, Bertolini S, et al. (2010) Connections between genetics and clinical data: Role of MCP-1, CFTR, and SPINK-1 in the setting of acute, acute recurrent, and chronic pancreatitis. Am J Gastroenterol 105(1):199–206
Garg PK, Khajuria R, Kabra M, Shastri SS (2009) Association of SPINK1 gene mutation and CFTR gene polymorphisms in patients with pancreas divisum presenting with idiopathic pancreatitis. J Clin Gastroenterol 43(9):848–852.
Whitcomb DC (2012) Genetics of alcoholic and nonalcoholic pancreatitis. Curr Opin Gastroenterol. 28(5):501–506
Jacob L, Geenen JE, Catalano MF, et al. (1999) Clinical presentation and short-term outcome of endoscopic therapy of patients with symptomatic incomplete pancreas divisum. Gastrointest Endosc 49(1):53–57
Lehman GA, Sherman S (1998) Diagnosis and therapy of pancreas divisum. Gastrointest Endosc Clin N Am 8(1):55–77
Kim MH, Lee SS, Kim CD, et al. (2001) Incomplete pancreas divisum: is it merely a normal anatomic variant without clinical implications? Endoscopy 33(9):778–785
Kamisawa T, Tu Y, Egawa N, Tsuruta K, Okamoto A (2006) Clinical implications of incomplete pancreas divisum. JOP 7(6):625–630
Chey WY, Chang TM (2003) Secretin, 100 years later. J Gastroenterol 38(11):1025–1035.
Devereaux BM, Fein S, Purich E, et al. (2003) A new synthetic porcine secretin for facilitation of cannulation of the dorsal pancreatic duct at ERCP in patients with pancreas divisum: a multicenter, randomized, double-blind comparative study. Gastrointest Endosc 57(6):643–647
Devereaux BM, Lehman GA, Fein S, et al. (2002) Facilitation of pancreatic duct cannulation using a new synthetic porcine secretin. Am J Gastroenterol 97(9):2279–2281
Jowell PS, Branch MS, Fein SH, et al. (2011) Intravenous synthetic secretin reduces the incidence of pancreatitis induced by endoscopic retrograde cholangiopancreatography. Pancreas 40(4):533–539
Nicaise N, Pellet O, Metens T, et al. (1998) Magnetic resonance cholangiopancreatography: interest of IV secretin administration in the evaluation of pancreatic ducts. Eur Radiol 8(1):16–22
Manfredi R, Costamagna G, Brizi MG, et al. (2000) Pancreas divisum and “santorinicele”: diagnosis with dynamic MR cholangiopancreatography with secretin stimulation. Radiology 217(2):403–408
Song MH, Kim MH, Lee SK, Seo DW (2002) The clinical usefulness of secretin-enhanced magnetic resonance pancreatography in patients with pancreas divisum and idiopathic acute pancreatitis. Gastrointest Endosc 55(3):454–455
Hellerhoff KJ, Helmberger H 3rd, Rosch T, et al. (2002) Dynamic MR pancreatography after secretin administration: image quality and diagnostic accuracy. Am J Roentgenol 179(1):121–129
Matos C, Metens T, Deviere J, et al. (2001) Pancreas divisum: evaluation with secretin-enhanced magnetic resonance cholangiopancreatography. GastrointestEndosc 53(7):728–733
Mosler P, Akisik F, Sandrasegaran K, et al. (2012) Accuracy of magnetic resonance cholangiopancreatography in the diagnosis of pancreas divisum. Dig Dis Sci 57(1):170–174
Carnes ML, Romagnuolo J, Cotton PB (2008) Miss rate of pancreas divisum by magnetic resonance cholangiopancreatography in clinical practice. Pancreas 37(2):151–153
Tirkes T, Akisik F, Tann M, Balci NC (2009) Imaging of the pancreas with secretin enhancement. Top Magn Reson Imaging 20(1):19–24
Akisik MF, Sandrasegaran K, Aisen AA, et al. (2006) Dynamic secretin-enhanced MR cholangiopancreatography. Radiographics 26(3):665–677
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86(2):420–428
Delhaye M, Cremer M (1992) Clinical significance of pancreas divisum. Acta Gastroenterol Belg 55(3):306–313
Moffatt DC, Cote GA, Avula H, et al. (2011) Risk factors for ERCP-related complications in patients with pancreas divisum: a retrospective study. Gastrointest Endosc 73(5):963–970.
Kamisawa T, Egawa N, Tu Y, Tsuruta K, Okamoto A (2007) Pancreatographic investigation of embryology of complete and incomplete pancreas divisum. Pancreas 34(1):96–102.
Liao Z, Gao R, Wang W, et al. (2009) A systematic review on endoscopic detection rate, endotherapy, and surgery for pancreas divisum. Endoscopy 41(5):439–444
Bret PM, Reinhold C, Taourel P, et al. (1996) Pancreas divisum: evaluation with MR cholangiopancreatography. Radiology 199(1):99–103
Kamisawa T, Tu Y, Egawa N, et al. (2007) MRCP of congenital pancreaticobiliary malformation. Abdom Imaging 32(1):129–133
Koshinaga T, Fukuzawa M (2000) Pancreatic ductal morphological pattern and dilatation in postoperative abdominal pain in patients with congenital choledochal cyst: an analysis of postoperative pancreatograms. Scand J Gastroenterol 35(12):1324–1329
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sandrasegaran, K., Cote, G.A., Tahir, B. et al. The utility of secretin-enhanced MRCP in diagnosing congenital anomalies. Abdom Imaging 39, 979–987 (2014). https://doi.org/10.1007/s00261-014-0131-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0131-z