Abstract
Purpose
Radiopeptide therapy using a somatostatin analogue labelled with a beta emitter such as 90Y/177Lu-DOTATOC is a new therapeutic option in neuroendocrine cancer. Alternative treatments for patients with refractory disease are rare. Here we report the first-in-human experience with 213Bi-DOTATOC targeted alpha therapy (TAT) in patients pretreated with beta emitters.
Methods
Seven patients with progressive advanced neuroendocrine liver metastases refractory to treatment with 90Y/177Lu-DOTATOC were treated with an intraarterial infusion of 213Bi-DOTATOC, and one patient with bone marrow carcinosis was treated with a systemic infusion of 213Bi-DOTATOC. Haematological, kidney and endocrine toxicities were assessed according to CTCAE criteria. Radiological response was assessed with contrast-enhanced MRI and 68Ga-DOTATOC-PET/CT. More than 2 years of follow-up were available in seven patients.
Results
The biodistribution of 213Bi-DOTATOC was evaluable with 440 keV gamma emission scans, and demonstrated specific tumour binding. Enduring responses were observed in all treated patients. Chronic kidney toxicity was moderate. Acute haematotoxicity was even less pronounced than with the preceding beta therapies.
Conclusion
TAT can induce remission of tumours refractory to beta radiation with favourable acute and mid-term toxicity at therapeutic effective doses.
Similar content being viewed by others
Introduction
Well-differentiated neuroendocrine tumours (NETs) demonstrate modest responses to conventional chemotherapy due to their slow proliferation rate [1]. However, the expression of somatostatin receptors by NET enables targeting with high-affinity peptides. When these octreotide analogue peptides are labelled with beta emitters such as 90Y [2] or 177Lu [3] promising anti-tumour effects have been observed. Recently, it has also been demonstrated that an improved tumour to nontumour uptake of radiolabelled DOTATOC is achieved after intraarterial administration in liver metastatic NET patients [4, 5]. However, patients with recurrences are usually refractory to further treatment with beta radiation therapy.
Alpha radiation is characterized by high linear energy transfer causing production of 2,000 – 7,000 ion pairs per micrometre, leading to clustered double-strand DNA breaks resulting in rapid cell death from even a single exposure to a few alpha particles. The short range of alpha particles (50 – 100 μm, i.e. about two or three cell diameters) limits the effective range of treatment but also limits damage to untargeted tissue. In contrast, beta-emitting radionuclides result in fewer than 20 ion pairs per micrometre and commonly cause only single-strand DNA breaks with less lethality and more spillover effects caused by “crossfire” (Fig. 1). It has already been demonstrated that the alpha emitter 213Bi is able to overcome radioresistance to beta emitters in vitro [6]. The alpha emitters 225Ac and 213Bi used to label the somatostatin analogue DOTATOC have demonstrated already promising antitumour effects with a favourable therapeutic range in animal studies [7, 8]. Therefore, it seemed reasonable that peptide targeted alpha therapy (TAT) with 213Bi-DOTATOC delivered directly to metastases via intraarterial administration might offer effective therapy to NET patients who have acquired resistance to other therapies.
Comparison of alpha and beta emitters. a, c After binding of the radionuclide-labelled octreotide analogue DOTATOC to the somatostatin receptor subtype-2 (SSR2), which is overexpressed in NETs, the emitted alpha particle causes high-density ionization effects, resulting mainly in double-strand DNA breaks. In contrast, the beta particles emitted by established radiopharmaceuticals mainly cause repairable single-strand DNA damage. b, d The tissue range of alpha emitters (about 80 μm) is approximately two cell diameters. The mean tissue range of the beta emitter 90Y (3 mm) is approximately 75 cell diameters. Thus, alpha emitters result in less “cross-fire” radiation to surrounding normal tissue
Here we report the first-in-human experience with 213Bi-DOTATOC TAT in patients refractory to nonradioactive octreotide and tandem therapy [9] with 90Y/177Lu-DOTATOC.
Materials and methods
Patients
This was a retrospective study of patients with differentiated neuroendocrine tumours. The diagnosis was confirmed histologically. These patients were not surgical candidates. Systemic standard therapies such as chemotherapy in high-grade or nonradioactive octreotide in low-grade tumours had previously failed to stop tumour growth. Pretreatment also included innovative peptide receptor radiation therapy (PRRT) with octreotide analogues tagged with a beta emitter. When patients showed progression with that treatment (new lesions on PET or progression on CT >30 % within the previous 2 – 6 months) TAT was offered as an alternative therapy. Seven consecutive patients with prognosis-affecting liver metastases arising from a pulmonary (one patient), pancreatic (four patients), enteric (one patient) or unknown primary (one patient) received intraarterial administration into the common hepatic artery between November 2010 and October 2011, and one patient with bone marrow carcinosis arising from neuroendocrine prostate cancer was treated systemically (Table 1, Supplementary Fig. 1). A positive tumour somatostatin receptor expression was validated by 68Ga-DOTATOC PET/CT. After the patients had given written informed consent, salvage therapies (compassionate use) were administered in accordance with the principles of the Helsinki Declaration (paragraph 37 “Unproven Interventions in Clinical Practice”) and our national regulations. The retrospective analyses of our observations were done with the approval of our ethics committee.
Peptide, radionuclides and radiolabelling
DOTATOC (DOTA0-Phe1-Tyr3) octreotide was synthesized as described by Otte et al. [10]. 225Ac was produced by radiochemical extraction from 229Th as described by Apostolidis et al. and Boll et al. [11, 12] and loaded on a 225Ac/213Bi radionuclide generator comprising AG MP-50 cation exchange resin (Bio-Rad) [13]. 213Bi was eluted as BiI4 −/BiI5 2− ion at intervals of 2 – 3 h using 1.4 ml 0.1 M HCl/0.1 M NaI. The eluate was added to a microwave vial containing 350 μl 2 M TRIS buffer, 100 μl 20 % ascorbic acid and 15 μl of 2 mg/ml DOTATOC solution. The reaction mixture was heated to 95 °C for 5 min using a microwave synthesizer (Biotage® Initiator) and subsequently cooled to <50 °C using pressurized air. Quality control was performed by instant thin-layer chromatography (ITLC-SG; Pall Life Sciences) with 0.05 M citric acid, pH 5, as solvent. Under these conditions, unbound 213Bi moves with the solvent front (R f = 1), while 213Bi-DOTATOC remains on the bottom of the strip (R f = 0). Radiochemical purity was determined by measuring the activity of the 440 keV gamma emission of 213Bi on the upper and lower part of the ITLC strip in an automated gamma counter (Berthold) using an energy window of 400 – 500 keV. Radiochemical purity was 99.7 ± 0.3 %. Specific activity was typically 80 MBq /nmol peptide at the time of injection. Injections were performed typically 15 ± 2 min after the end of generator elution. Before injection, sterility of the final formulation was ensured via sterile filtration (Millex-GV, 0.20 μm; Millipore). The decay properties of the 229Th/225Ac/213Bi radionuclide generator system are presented in Supplementary Fig. 2. Decay data are taken from Nucleonica [14] and recent measurements [15–17].
Imaging
Staging and restaging procedures included contrast-enhanced CT (CE-CT) and 68Ga-DOTATOC PET/CT. Contrast-enhanced MRI (CE-MRI) using a hepatocyte-specific contrast medium was also performed in patients with liver metastases. In the first year restaging was performed every 3 months, and from the second year every 6 months.
DOTATOC PET/CE-CT
The PET studies were acquired with a Biograph 6 PET/CT scanner (Siemens Medical Systems, Erlangen, Germany). The scanner resolution (according to NEMA2001) was 5.5 – 6.0 mm at full-width half-maximum (FWHM). The transaxial field-of-view (FOV) of 605 mm was covered by a 512 matrix and the axial FOV of 162 mm was covered with 65 slices per bed position. So the reconstructed voxel size was 1.2 × 1.2 × 2.5 mm. Imaging was started 60 ± 10 min after the .intravenous injection of 84 – 196 MBq of 68Ga-DOTATOC. Static emission scans – corrected for dead time, scatter and decay – were acquired from the vertex to the proximal legs, requiring eight bed positions (4 min each). The images were iteratively reconstructed with the ordered subsets expectation maximization algorithm using four iterations with eight subsets and Gaussian filtering of 5 mm FWHM. CE-CT was performed as part of the PET/CT scan. Iodinated contrast medium (Imeron 400; Bracco Diagnostics, Milan, Italy) was injected at a flow rate of 4 ml/s. The liver and abdomen were initially examined without contrast medium (130 keV, 30 mAs, CareDose), followed by an arterial phase (25 s delay) and a portal venous phase (60 s delay). The low-dose CT scan without contrast medium was used for attenuation correction. Slice collimation was 6 × 1.0 mm, pitch factor 1.5, 110 keV, 95 mAs (CareDose), matrix 512 × 512 and rotation time 0.6 s, reconstructed to a slice thickness of 1.25 mm and 0.8-mm increment with a B30 kernel. Secondary raw data were reformatted to a slice thickness of 5 mm with a 2.5-mm increment in the coronal and axial views.
Magnetic resonance imaging
Magnetic resonance examinations were performed on a 1.5-T MR system (Avanto, Siemens Medical Systems, Erlangen, Germany). Unenhanced T1-weighted (gradient echo, TR 192 ms, TE 4.76 ms, 256 × 154 matrix) and T2-weighted (HASTE, TR 801 ms, TE 69 ms, 384 × 213 matrix) fast spin echo axial imaging was performed before diffusion-weighted MRI and Gd-EOB-DTPA (Primovist®; Bayer Schering, Berlin, Germany) administration for CE-MRI. This hepatocyte-specific contrast medium was considered as the standard of reference for tumour delineation [18]. Diffusion-weighted imaging was performed with a breath-hold single shot echo planar sequence (TR 12,200 ms, TE 67 ms, FOV 430 cm, section thickness 5 mm, b values 50, 300 and 600 s/mm2, voxels 3.3 × 3.3 × 5, EPI factor 112). The acquisition of delayed MR data after contrast medium administration started with the intravenous administration of 0.1 mmol/kg body weight of the contrast medium Gd-EOB-DTPA with an infusion rate of 1.5 ml/s followed by a 30-ml saline bolus. Imaging was performed with a T1-weighted VIBE (volumetric interpolated breath-hold examination) with TR 3.41 ms, TE 1.18 ms, slice-thickness 4 mm and matrix 320 × 180, with 72 axial slices and an acquisition time of 20 s for each dataset.
Treatment regimen
Preceding therapy with “cold” octreotide analogue was discontinued for at least 6 weeks to exclude receptor occupancy. For locally intensified liver treatment a 4F catheter (Sidewinder S1; Terumo) was placed in the coeliac artery via transfemoral access using the Seldinger technique with local anaesthesia. Subsequently, a microcatheter (Progreat, Terumo) was inserted coaxially and advanced to the common hepatic artery or proper hepatic artery. In patients with anatomical variation, the largest arterial feeder was cannulated. The catheter was used to administer the 213Bi-DOTATOC. The patient with bone marrow carcinosis received an antecubital infusion of the drug. 213Bi-DOTATOC was given in increasing activities in cycles every 2 months (first cycle, about 1.0 GBq; second cycle, about 1.5 GBq; third cycle, 2 – 4 GBq; fourth cycle, as available from the generator system); cumulative and highest single activities are shown in Table 1. To minimize renal toxicity, 1,000 ml of a nephroprotective solution containing 30 g lysine and 30 g arginine and 500 ml of Gelofusine was administered simultaneously, followed by 1,000 ml of saline as developed for radiopeptide therapy with beta emitters [19].
213Bi-DOTATOC scintigraphy
Within the first 60 min after administration of 213Bi-DOTATOC a planar whole-body scan and SPECT scan of the liver were acquired with a Hawkeye gamma camera (GE Healthcare, Little Chalfont, UK) using the standard high-energy collimator and the 440 keV (± 10 %) gamma emission window. Scan speed was 8 cm/min for the whole-body scan. SPECT was done in the step-and-shoot mode with 120 projections every 3° and a 20-s acquisition time per step. Specific binding of 213Bi-DOTATOC to the target structures was validated by coreading of the 68Ga-DOTATOC PET scan in comparison to the therapeutic gamma emission scans.
Pharmacokinetics
Blood samples were taken every 10 min after injection of the first fraction of 213Bi-DOTATOC to assess plasma clearance. Urine was collected for 45 min after injection. Due to the short half-life of 213Bi (46 min), the samples were immediately evaluated by ex-vivo gamma counting (LB 951G; Berthold, Bad Wildbad, Germany).
Toxicity
Acute haematological and chronic kidney toxicity are most relevant in PRRT. Haematological toxicity was documented according to the ECOC common toxicity criteria with blood samples obtained at baseline and 48 h, then every week for the first month after treatment and then every 2 weeks. Creatinine clearance, blood urea nitrogen (BUN), and liver enzymes were determined at least every 2 weeks after therapy. As DOTATOC shows physiological uptake in the pituitary gland and adrenals, we assessed endocrine toxicity with stimulation tests, including thyroid-stimulating hormone after stimulation with thyrotropin-releasing hormone, cortisol after stimulation with synthetic adrenocorticotropic hormone, and follow-up with serum catecholamines and the insulin-like growth factor 1, as recommended [20]. Patients underwent regular clinical examination to check for unexpected side effects. Glomerular filtration rate (GFR) [21] and tubular excretion rate (TER) [22] were assessed with 51Cr-EDTA and 99mTc-MAG3, respectively, at baseline, and 3 and 9 months after therapy.
Results
Pharmacokinetic data
Time–activity curves in blood, as presented in Supplementary Fig. 3, were similar to data reported in the literature for intravenously administered diagnostic somatostatin analogues [23, 24]. Within the first half-life of the radionuclide an average of 15.1 ± 7.7 % (range 0.1 – 35.4 %) was eliminated in the urine. The 440 keV gamma coemission of 213Bi was sufficient to acquire evaluable planar and SPECT scans in patients undergoing therapy at all injected activities. Coreading with the pretherapeutic 68Ga-DOTATOC PET scans validated specific binding at the tumour sites (Fig. 2).
Diagnostic 68Ga-DOTATOC PET scans in NET patients 1, 2 and 6 (a, b, c). d In patient 1 the largest lesion was highly selectively cannulated for intraarterial administration of 213Bi-DOTATOC (top left); 440 keV SPECT scan (bottom left) and whole-body planar (right) scans 45 min after injection demonstrate peak uptake in the target lesion in liver segment 6. e Patient 2 received two therapeutic injections, one into liver segments 5 – 8 (top left) and one into segment 4a/b (top right); 440 keV emission scans (bottom left and right) 045 min after injection show the impact of intraarterial administration for fast tumour targeting and regionally intensified peptide accumulation. f In whole-liver treatment (patient 6) the hepatic biodistribution of 213Bi-DOTATOC is the same as the distribution of 68Ga-DOTATOC, but in comparison to systemic treatment spares the spleen
Clinical course of patients
All patients had presented with a specific clinical challenge when 213Bi-DOTATOC treatment was offered. Patient 1 with multiple liver metastases received intraarterial therapy with 177Lu-DOTATOC. During follow-up, all except one metastasis showed a response. However, the nonresponding lesion showed rapid progression. The segmental branch of the feeding liver artery was catheterized highly selectively to administer 1 GBq of 213Bi-DOTATOC. Subsiding restaging presented partial remission including the previously nonresponding lesion. The staging examination, angiography and restaging are shown in Fig. 2a, d and Supplementary Fig. 4. Subsequently the patient received four additional cycles of 213Bi-DOTATOC to a cumulative administered activity of 16 GBq. Patient 2 presented with highly disseminated metastatic NET in the liver embedded in only small bridges of healthy tissue. With their tissue range of several millimetres, we hypothesized that beta emitters would probably have caused radiation-induced failure of the remaining normal liver parenchyma. 213Bi-DOTATOC was administered in five cycles (19.5 GBq) by intraarterial injection. Liver enzymes returned to normal within 6 weeks and a substantial radiological response was seen (Fig. 3). No acute liver toxicity was observed. At the time of this report, this response had been maintained for 30 months. Myelodysplastic syndrome (MDS) was diagnosed 24 months after TAT, i.e. 5 years after the first PRRT with 90Y-DOTATOC. Six months later, MDS progressed into acute myeloid leukaemia (AML) and the patient died.
Patient 2 with disseminated liver metastases. a–c Initial findings. Coronal (a) and transaxial (b) slices through the liver performed with a hepatocyte-specific contrast medium. Metastases appear as “black holes” against the enhanced normal liver parenchyma. In the diffusion-weighted image (c), metastases show high signal intensities, while normal liver appears dark. d–f After three cycles of 213Bi-DOTATOC to a cumulative dose of 12 GBq, most of the liver parenchyma has recovered to a normal appearance. The images with hepatocyte-specific contrast medium appear homogeneous (d, e), and most of the disseminated diffusion restrictions have diminished (f)
Patient 3 was a 40-year-old woman with a pulmonary carcinoid with hepatic metastases. Pathology of the resected pulmonary specimen revealed moderate to undifferentiated grade II/III disease (Ki-67 30 %). Under carboplatin/etoposide therapy the tumour progressed in the liver. Subsequent locoregional infusion of 90Y-DOTATOC also failed to halt progression. Imaging revealed the acute danger of occlusion of the liver vein and the lower caval vein. Therefore, this patient received, 19.3 GBq 213Bi-DOTATOC divided into five cycles administered through a hepatic artery catheter. A partial response was observed in the liver and the response had been maintained for 34 months at the time of this report (Fig. 4). Patient 4 was referred to our department with hepatic encephalopathy due to extensive liver metastases. After intraarterial administration of 213Bi-DOTATOC to a cumulative dose of 20.8 GBq, the patient was stable for 1 year without a further hepatic event and then extrahepatic progression was diagnosed. Patient 5 failed to respond to conventional somatostatin analogue therapy but demonstrated a partial response in the liver and pancreatic primary tumour to the first three cycles of 90Y-DOTATOC, but then became refractory. Liver metastases (proper hepatic artery) and the primary tumour (gastroduodenal artery) were simultaneously accessible by 213Bi-DOTATOC injection into the common hepatic artery. After receiving 13.3 GBq 213Bi-DOTATOC intraarterially into the shared feeder, complete responses were observed in the liver and the primary, which had been maintained for 28 months at the time of this report (Fig. 5).
Patient 3 with the acute danger of occlusion of both the liver veins and the lower caval vein due to a large lesion in the upper central liver (a, MR image) which was addressed by locoregional DOTATOC therapy administered into the proper hepatic artery (b, digital subtraction angiogram). Intense 68Ga-DOTATOC uptake and uptake of contrast medium for CT was present in the initial staging (c, fused PET/CT image). Only PET-negative, morphologically cystic residuals were found 6 months after therapy (d, fused PET/CT image)
Patient 5 before therapy (a–c) and after three cycles of 213Bi-DOTATOC (d–f) to a dose of 4 GBq. a Beta-resistant residuals in the liver (long arrows) and primary tumour (short arrow) are present in the DOTATOC PET maximum intensity projection image. b CE-CT image with the primary tumour outlined in red. c In the MR image with hepatocyte-specific contrast medium, the liver metastases appear as black cavities against the enhancing normal liver parenchyma. d–f After three cycles of 213Bi-DOTATOC to a dose of 4 GBq, the lesions have diminished on the PET image (d) and CT image (e). Also on the MR image (f), the residual lesion has almost disappeared as shown by the growth of normal hepatocytes demonstrated by the uptake of the hepatocyte-specific contrast medium
Patient 6 presented with multiple progressive bulky liver metastases. Under therapy with 90Y-DOTATOC some parts of the tumour became necrotic but the major mass remained active (Fig. 2c). In escalating doses he received a cumulative dose of 20.6 GBq 213Bi-DOTATOC regionally into the liver artery. The previously hyperarterialized lesions changed to a devascularized mass, which showed stable disease after a follow-up of 31 months at the time of this report. Patient 7 presented with liver and bone metastases, but progressive liver metastases were considered to determine the prognosis. This patient had a history of grade IV haematotoxicity (thrombocytes <25,000/μl) after treatment with 90Y-DOTATOC. After receiving 13.7 GBq 213Bi-DOTATOC into the hepatic artery, substantial partial responses were observed in the liver and also the bone (Fig. 6) with striking disappearance of bone marrow lesions but with only grade II haematotoxicity. The patient had maintained the liver response for 24 months at the time of this report; extrahepatic progression occurred after 15 months.
Patient 7 with an extensive tumour burden in the left liver lobe and multiple lesions in the right lobe, as well as disseminated bone marrow metastases predominantly in the spine and pelvis. These are demonstrated in coronal and sagittal 68Ga-DOTATOC-PET maximum intensity projections (a). As expected, liver metastases showed significant shrinkage after administration of 10.5 GBq of 213Bi-DOTATOC into the common hepatic artery. Additional systemic efficiency resulting from the 213Bi-DOTATOC reaching the systemic circulation after the first pass of the liver was noted after 6 months in that most of the bone marrow metastases had also diminished (b)
Due to the promising “systemic side-response” and the low acute haematotoxicity in patient 7, a systemic treatment consisting of 3.3 GBq of 213Bi-DOTATOC was offered to patient 8, who suffered from diffuse bone infiltration from neuroendocrine prostate cancer. Radiological treatment response in non-solid tumours is not assessable, but despite an advanced tumour spread, including disseminated bone marrow involvement, no relevant acute haematological side effects were observed and the patient was still alive after more than 12 months follow-up at the time of this report (Fig. 7).
Patient with bone marrow carcinosis arising from neuroendocrine prostate cancer. After systemic therapy with 3.3 GBq 213Bi-DOTATOC only grade I thrombopenia (>100.000/μl), grade I neutropenia (neutrophils >2,000/mm3) and grade I total WBC (>3,000/mm3) were observed 2 weeks after therapy and recovered until week 4. Red blood cells, haemoglobin gammaGT and creatinine showed no relevant change within 5 months (circles platelets, triangles haemoglobin, inverted triangles red blood cell count, black squares total white blood cell count, white squares absolute neutrophil count, grey squares absolute lymphocyte count, hexagons creatinine, diamonds gammaGT)
Toxicity
The mean TERs from 99mTc-MAG3 were 251 ml/min, 179 ml/min and 152 ml/min/1.73m2 body surface area at baseline, 1 year after therapy and 2 years after therapy, respectively. The mean GFRs from 51Cr-EDTA were 115 ml/min, 101 ml/min and 83 ml/min at baseline, 1 year after therapy and 2 years after therapy, respectively. Serum creatinine and BUN were unchanged in all but one patient, who had a creatinine value between 1 and 1.5 times the upper limit of normal 2 years after therapy. Due to the small number of patients, we present the individual values for blood cell count, TER, GFR and creatinine in each patient in the Supplementary material (Supplementary Fig. 5). Acute haematological toxicity was low. One patient with a previous history of grade IV thrombopenia with 90Y-DOTATOC therapy developed grade II thrombopenia with 213Bi-DOTATOC. The acute changes in blood were grade 0/I in the other patients. During the long-term follow-up, three patients developed chronic anaemia. In patient 2 MDS/AML was diagnosed consecutively. Erythropoietin levels in the lower normal range were found in patient 3 (grade II anaemia, onset between 12 and 24 months after TAT) and in patient 7 (grade I/II anaemia, onset 12 months after TAT). The beginning of anaemia was correlated with late effects on TER or GFR and not related to the time of treatment. Only patient 3 was symptomatic and showed a favourable response to substitution of erythropoietin (Epoetin Alfa Hexal). Therefore anaemia was interpreted as a side effect on endocrine kidney function rather than on bone marrow function. The other hormones and endocrine stimulation tests (pituitary, thyroid, adrenals, androgens), as described in the Materials and methods section, were neither systematically nor relevantly changed. In patient 3 Graves’ disease was diagnosed 1 year after the last treatment cycle and has to be considered therapy-associated because thyroid cells can also express somatostatin receptors.
Discussion
Here we report the first-in-human experience with 213Bi-DOTATOC TAT in NET patients refractory to nonradioactive octreotide and 90Y/177Lu-DOTATOC. It was possible to image the biodistribution of the therapeutic compound with conventional 440 keV scintigraphy scans. Tumour binding was comparable to that in diagnostic SSR imaging with 68Ga-DOTATOC (Fig. 2). Therefore, we concluded that the in vivo stability and pharmacokinetics of 213Bi-DOTATOC are sufficient and comparable to those of DOTATOC labelled with other radionuclides. The clearance patterns of the time–activity curves obtained with ex-vivo gamma-counting of blood and urine samples were similar to previously reported values for intravenously administered diagnostic somatostatin analogues [23, 24]. The time–activity blood values from venous blood samples following intraarterial injection should represent the amount of peptide that has passed the target organ and reached the systemic circulation and should represent a parallel shift to that seen in the time–activity curve following intravenously administration. However, we have previously observed that the relevance of the first-pass effect depends on the tumour burden in the liver and differences between patients are higher for the intraarterial administration route [4]. Sufficient in vivo stability of DOTATOC labelled with the beta emitter has already been reported [2, 10]. In vitro autoradiolysis of 213Bi-DOTATOC is prevented with ascorbic acid. However, in contrast to beta-DOTATOC, the alpha decay might translate into damage to the peptide. Nevertheless, once the alpha particle is emitted, the fate of the peptide is only of limited interest, as tumour targeting is only pivotal as long as the molecule is radioactive.
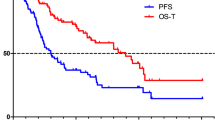
The reported patient cohort was rather heterogeneous, because this was not a clinical trial with prospectively defined inclusion criteria but represented the experience with surrogate treatments offered individually to patients in challenging situations. Due to the limited clinical experience with TAT the first patient was treated with a highly selective administration into the tumour feeding artery of a single rapidly progressive metastasis. In this first patient we were able to demonstrate that it is possible to overcome the resistance to beta treatment without significant acute toxicity. The next three patients were in a life-threatening situation when they received their first cycle of liver-selective TAT. In patient 3 an acute risk of vessel occlusion was resolved successfully (Fig. 4). In long term follow-up the progression-free survival was 36 months. This is a remarkable clinical result. In contrast, the 2-year overall survival of patients with undifferentiated pulmonary carcinoids refractory to etoposide/carboplatin is <20 % if treated with FOLFIRI or topotecan [25]. Patient 4 was scheduled for liver-directed radionuclide therapy after an episode of hepatic encephalopathy. While the liver metastases demonstrated a positive response to the regionally intensified arterial therapy, the patient showed extrahepatic progression. However, due to improved liver function, the experimental TAT was stopped and he was able to receive chemotherapy again which was still effective for his bone metastases.
Patient 5 showed partial remission after the initial cycles of 90Y/177Lu-DOTATOC, but then no further tumour shrinkage of the residual masses was achieved. Due to the favourable acute and mid-term toxicity observed in our first TAT patients, we individually offered TAT to this patient and achieved long-lasting complete remissions in both the primary tumour and liver metastases. Hepatic arterial infusion of TAT was indicated in patient 7 as disseminated liver involvement was considered the leading factor in the overall prognosis. Surprisingly, in addition to the expected liver response, we also found “side-efficacy” to various small bone marrow lesions. As the tumoral accumulation maximum (U max) of intravenously administered DOTATOC is about 70 min after injection (with 80 % of U max reached 45 min after injection), we did not anticipate sufficiently fast tumour targeting and did not expect to achieve a reliable tumour-to-blood dose ratio with a short half-life radionuclide such as 213Bi (45.6 min) [24]. However, after we observed a response of bone marrow lesions in patient 7, we offered systemic TAT to patient 8 with disseminated bone marrow carcinosis in whom PRRT with beta particles was considered contraindicated. While treatment response in non-solid lesions is not evaluable according to RECIST criteria, we are able to report a remarkable low acute haematological toxicity. This is in accordance to the concept of cell selective micro-dosing due to the short path length (about two cell diameters) of an alpha particle, and consistent with the experience with CD33 targeted radionuclide therapy of AML. A 131I-labelled anti-CD33-mAb translated into a myeloablative bone marrow dose [26]. In contrast, with 213Bi-labelled anti-CD33-mAb it was possible to induce a reduction of bone marrow blasts with tolerable haematological toxicity [27].
We found a relevant decline in both TER and GFR in all our patients treated with TAT. In a study evaluating renal toxicity after 90Y-DOTATOC or 177Lu-DOTATATE therapy, of 23 patients who received a median dose of 12.2 GBq 90Y-DOTATOC, 12 showed a creatinine clearance loss of >5 % and 8 a loss of >10 %, and of 5 patients who received a median dose of 23.2 GBq 177Lu-DOTATATE, 3 showed a creatinine clearance loss of >5 % and 2 a loss of >10 % at 1 year. Based on these data, a kidney tolerance threshold of 28 Gy was recommended [28]. In our patients the kidney tolerance dose had already been consumed during the extensive pretreatment with beta-emitting PRRT, and thus a higher grade of kidney impairment was expected. However, during the follow-up of 2 years, none of our patients developed severe kidney failure requiring dialysis. Nevertheless, none of our patients showed pathological renal test results when TAT was started. The toxicity of TAT could be even more severe in patients with renal risk factors or previously damaged kidneys, and therefore we still need to be cautious in the use of TAT in patients with a long life expectancy.
In a preclinical investigation 213Bi-DOTA-PESIN was compared with 177Lu-DOTA-PESIN [29]. No tubular degeneration but rather glomerulopathy was observed with 177Lu-DOTA-PESIN. In contrast, with 213Bi-DOTA-PESIN, tubular degeneration was the leading pathology. Following glomerular filtration, radiolabelled peptides are reabsorbed and trapped in the tubular cells. Due to the short range of alpha particles the authors suggested that mainly tubular cells were irradiated. In contrast, beta particles may reach the radiosensitive glomeruli. Therefore, we monitored kidney function with dedicated 99mTc-MAG3 and 51Cr-EDTA tests for TER and GFR, respectively. With a 40 % decline in TER and a 30 % decline in GFR during a 2-year period in our patients the tubular impairment was only slightly higher than glomerular toxicity. This would support the assumption that some of the toxicity can be attributed to the preceding beta-PRRT. However, it is not legitimate to compare the kidney toxicity of first-line beta-PRRT with the toxicity of alpha-PRRT in pretreated patients and overlap with kidney toxicity from the earlier therapy. After 90Y-DOTATOC treatment kidney failure after a latency period of even 15 months has been reported previously [30].
For a long time alpha emitters have been considered the perfect fit for Ehrlich’s “magic bullet” approach to cell-selective cancer therapy [31]. The advantage of alpha over beta radiation in therapeutic nuclear medicine has already been demonstrated in preclinical studies [6]. Octreotide analogues labelled with alpha particle emitters have also shown a reasonable therapeutic range in animals [7, 8]. However, until now the limited availability of these radioisotopes has been a key challenge for the transfer to clinical use. To date, the required 225Ac to build a high-activity generator system to provide sufficient 213Bi for clinical use has only been possible by combining the maximum activity currently available from the three producers, i.e. Oak Ridge National Laboratory (Oak Ridge, TN), the Institute for Transuranium Elements (Karlsruhe, Germany) and the Institute for Physics and Power Engineering (Obninsk, Russia). However, the recent development of accelerator-driven processes that allow production of the mother nuclide for 225Ac/213Bi generators in practically unlimited amounts may overcome these supply limitations in the near future [32, 33].
Recently the use of 223Ra, another alpha-emitting radionuclide and an inherent bone seeker, has led to improved survival in patients suffering from bone metastases of prostate cancer [34]. However, the stable linkage of divalent 223Ra(II) to antibodies or other carrier molecules has not been successful. We introduced the chelatable, alpha-emitting radionuclide 213Bi to clinical PRRT targeting the somatostatin receptors of NET patients. The chelate molecule DOTA (1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid) has already been linked to a variety of tumour-targeting molecules, and therefore our approach could be easily transferable to other targeted therapies in oncology.
In the first preclinical phase of our study, we had to develop suitable labelling conditions for 213Bi-DOTATOC. Finally, a reliable protocol for the synthesis of clinical doses of 213Bi-DOTATOC was successfully established (see Materials and methods section). The 225Ac/213Bi generator system developed at the Institute for Transuranium Elements was demonstrated to be able to reliably provide single doses of up to 2 GBq 213Bi-DOTATOC per injection. Labelling yields of 213Bi-DOTATOC reliably exceeded 99 %.
While the clinical application of alpha emitters promises advantages due to the short path length and the high linear energy transfer of the emitted particle (Fig. 1), there are also some challenges associated with the available nuclides. The main route (98 %) of 213Bi decay involves an initial beta decay with 435 keV mean energy immediately (delay 3.7 μs) followed by the therapeutic alpha decay to 209Pb which is a beta emitter with 198 keV mean energy (half-life 3.2 h) and decays to quasistable 209Bi (Supplementary Fig. 2). While the beta emissions contribute only about 8 % to the absorbed tissue dose [35], the bremsstrahlung following the beta decay compromise the inherent imaging abilities of 213Bi that is based on the emission of 440 keV gamma ray with an emission probability of 26 % per decay. Due to the recoil of the alpha particle, 209Pb (3.2 h) is expected to leave the DOTA chelate and eventually even the target tissue to redistribute to nontarget organs, thus translating into high background noise.
The short half-life of 213Bi (45.6 min) is also challenging in regard to the limited temporal resolution of conventional scintigraphy. In addition, the spatial resolution of a gamma camera is insufficient to provide reliable microdosimetry. In a post-mortem autoradiography evaluation of a subject exposed to the alpha emitter 232Th, microscopic “hot spots” with doses up to 50-fold higher than those assuming a homogeneous organ biodistribution were found [36]. Therefore the 440 keV gamma images of 213Bi-DOTATOC are not sufficient for imaging-based dosimetry. However, the value of pretherapeutic dosimetry is still a controversial debate for radioiodine therapy and even 124I-PET-based treatment regimens have not been shown to be superior to the use of standard activities [37]. Therefore, dose finding in our patients was done in a similar empirical manner to the procedure used for the establishment of new chemotherapeutics with escalating activity fractions until dose-limiting toxicity was observed.
Another challenge for blood and bone marrow dosimetry is the redistribution of the unstable, beta-emitting decay product 209Pb, which might partially leave the tumour tissue. Free Pb is known to accumulate in erythrocytes which can translate to a perfusion-dependent increase in bone marrow radiation [38]. However, the decay chain of clinically used 223Ra and 224Ra includes the formation of 211Pb (half-life 36.1 min) or 212Pb (half-life 10.6 h), which should show redistribution patterns similar to that of 209Pb, and is followed by an additional alpha emission in the succeeding decay schema. Nevertheless, they are not associated with remarkable bone marrow toxicity [34, 38]. In contrast, the energy transfer from the beta radiation of 209Pb might be considered almost negligible, and also the long period to onset of anaemia observed in the follow-up of patients receiving TAT contradicts the thesis of directly related red blood cell or bone marrow toxicity. However, it would be of particular interest to develop dosimetry tools that might enable absorbed doses to be modelled and probabilities predicted for response and toxicity prior to TAT.
Haematological and kidney toxicity are the limiting factors in the use of 90Y/177Lu-DOTATOC. With 213Bi-DOTATOC acute haematological toxicity was moderate even in a patient with disseminated bone marrow involvement (Fig. 7). This is in accordance with the observations of the ALSYMPCA trial. The haematological toxicity of the bone-seeking alpha emitter 223Ra was not significantly higher than that of placebo [34]. In contrast, bone seekers labelled with a beta emitter can cause a relevant rate of grade-III thrombocytopenia and leucopenia [39]. MDS/AML was observed in one patient 2 years after initiation of TAT. However, this patient was heavily pretreated with 16 GBq 90Y-DOTATOC and 24 GBq 177Lu-DOTATOC in multiple cycles starting 5 years before the onset of MDS. MDS/AML has been found in 4.2 % of patients treated with 90Y-Zevalin during long-term follow-up with a mean latency of 4.8 years [40]. This is also in accordance with single case reports of MDS/AML from beta-PRRT centres in Rotterdam and Bonn [3, 41]. Therefore, the MDS/AML that occurred in our patient matches well the typical latency period for a 90Y-related secondary malignancy.
With a follow-up period of 3 years, no myeloproliferative disorders were found in patients who had received the bone-seeking alpha emitter 223Ra [34]. Nevertheless, alpha emitters produce a high rate of double-strand DNA breaks and might be associated with a higher number of secondary neoplasias. Therefore, thorough long-term follow-up will be pivotal once TAT is evaluated in prospective clinical trials for first-line or second-line therapy, especially in patients with a good prognosis. Our reported experience is not sufficient to conclude that alpha-emitting radiopharmaceuticals are superior to beta-emitting radiopharmaceuticals in general. For the reported patients, the duration of tumour control with the preceding 90Y/177Lu-DOTATOC therapy was up to 3 years (Table 1), and the follow-up in patients receiving TAT was only 2 years at the time of this report. However, we successfully demonstrated the feasibility of overcoming beta resistance with alpha emitters as an additional treatment line.
Conclusion
All patients reported in this investigation were in different challenging situations when receiving TAT with 213Bi-DOTATOC. TAT was shown to be able to overcome resistance against beta radiation and resulted in a high number of long-lasting anti--tumour responses. 213Bi-DOTATOC was associated with moderate acute haematological toxicity, even in a patient with highly disseminated bone marrow involvement. Chronic kidney impairment remained in the acceptable range, and no other organ toxicity was observed. Bringing together the possibility of producing the alpha emitter 213Bi in sufficient quantities to support universal clinical application in combination with chelate-conjugated targeting molecules, our results with TAT might open new avenues in therapeutic nuclear medicine.
References
Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008;9:61–72.
Waldherr C, Pless M, Maecke HR, Haldemann A, Mueller-Brand J. The clinical value of [90Y-DOTA]-D-Phe1-Tyr3-octreotide (90Y-DOTATOC) in the treatment of neuroendocrine tumours: a clinical phase II study. Ann Oncol. 2001;12(7):941–5.
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, Essen M, Kooij PP, et al. Treatment with the radiolabeled somatostatin analog [177Lu-DOTA0, Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol. 2008;26:2124–30.
Kratochwil C, Giesel FL, López-Benítez R, Schimpfky N, Kunze K, Esenhut M, et al. Intraindividual comparison of selective arterial versus venous 68Ga-DOTATOC PET/CT in patients with gastroenteropancreatic neuroendocrine tumors. Clin Cancer Res. 2010;16(10):2899–905.
Kratochwil C, López-Benítez R, Mier W, Haufe S, Isermann B, Kauszor U, et al. Hepatic arterial infusion enhances DOTATOC radiopeptide therapy in patients with neuroendocrine liver metastases. Endocr Relat Cancer. 2011;18(5):595–602.
Friesen C, Glatting G, Koop B, Schwarz K, Morgenstern A, Apostolidis C, et al. Breaking chemoresistance and radioresistance with [213Bi]anti-CD45 antibodies in leukemia cells. Cancer Res. 2007;67:1950–8.
Norenberg JP, Krenning BJ, Konings IR, Kusewitt DF, Nayak TK, Tl A, et al. 213Bi-[DOTA0, Tyr3]octreotide peptide receptor radionuclide therapy of pancreatic tumors in a preclinical animal model. Clin Cancer Res. 2006;12:897–903.
Miederer M, Henriksen G, Alke A, Mossbruger I, Quantanilla-Martinez L. Preclinical evaluation of the alpha-particle generator nuclide 225Ac for somatostatin receptor radiotherapy of neuroendocrine tumors. Clin Cancer Res. 2008;14:3555–61.
Kunikowska J, Królicki L, Hubalewska-Dydejczyk A, Mikołajczak R, Sowa-Staszczak A, Pawlak D. Clinical results of radionuclide therapy of neuroendocrine tumours with 90Y-DOTATATE and tandem 90Y/177Lu-DOTATATE: which is a better therapy option? Eur J Nucl Med Mol Imaging. 2011;38(10):1788–97.
Otte A, Mueller-Brand J, Dellas S, Nitzsche EU, Herrmann R, Maecke HR. Yttrium-90-labelled somatostatin-analogue for cancer treatment. Lancet. 1998;351:417–8.
Apostolidis C, Molinet R, Rasmussen G, Morgenstern A. Production of Ac-225 from Th-229 for targeted alpha therapy. Anal Chem. 2005;77:6288–91.
Boll RA, Malkemus D, Mirzadeh S. Production of actinium-225 for alpha particle mediated radioimmunotherapy. Appl Radiat Isot. 2005;62(5):667–79.
Morgenstern A, Bruchertseifer F, Apostolidis C. Bismuth-213 and actinium-225 generator performance and evolving therapeutic applications of two generator-derived alpha-emitting radioisotopes. Curr Radiopharm. 2012;5:221–7.
Nucleonica – Web driven nuclear science. European Commission, Joint Research Centre, Institute for Transuranium Elements; 2007. http://www.nucleonica.net/index.aspx. Accessed 16 July 2014.
Pommé S, Marouli M, Suliman G, Dikmen H, Van Ammel R, Jobbágy V, et al. Measurement of the 225Ac half-life. Appl Radiat Isot. 2012;70:2608–14.
Suliman G, Pommé S, Marouli M, Van Ammel R, Stroh H, Jobbágy V, et al. Half-lives of 221Fr, 217At, 213Bi, 213Po and 209Pb from the 225Ac decay series. Appl Radiat Isot. 2013;77:32–7.
Marouli M, Suliman G, Pommé S, Ammel RV, Jobbágy V, Stroh H, et al. Decay data measurements on 213Bi using recoil atoms. Appl Radiat Isot. 2013;74C:123–7.
Giesel FL, Kratochwil C, Mehndiratta A, Wulfert S, Moltz JH, Zechmann CM, et al. Comparison of neuroendocrine tumor detection and characterization using DOTATOC-PET in correlation with contrast enhanced CT and delayed contrast enhanced MRI. Eur J Radiol. 2012;81(10):2820–5.
Rolleman EJ, Valkema R, de Jong M, Kooij PP, Krenning EP. Safe and effective inhibition of renal uptake of radiolabelled octreotide by a combination of lysine and arginine. Eur J Nucl Med Mol Imaging. 2003;30:9–15.
Teunissen JJ, Krenning EP, de Jong FH, de Rijke YB, Feelders RA, van Anken MO, et al. Effects of therapy with [177Lu-DOTA0, Tyr3]octreotate on endocrine function. Eur J Nucl Med Mol Imaging. 2009;36:1758–66.
Piepsz A, Colarinha P, Gordon I, Hahn K, Olivier P, Sixt R, et al. Guidelines for glomerular filtration rate determination in children. Paediatric Committee of the European Association of Nuclear Medicine. Eur J Nucl Med. 2001;28:BP31–6.
Werner E, Blasl C, Reiners C. Reproducibility of technetium-99m-MAG3 clearance using the Bubeck method. J Nucl Med. 1998;39(6):1066–9.
Pettinato C, Sarnelli A, Di Donna M, Civollani S, Nanni C, Montini G, et al. 68Ga-DOTANOC: biodistribution and dosimetry in patients affected by neuroendocrine tumors. Eur J Nucl Med Mol Imaging. 2008;35(1):72–9.
Hofmann M, Maecke H, Börner R, Weckesser E, Schoffski P, et al. Biokinetics and imaging with the somatostatin receptor PET radioligand 68Ga-DOTATOC: preliminary data. Eur J Nucl Med. 2001;28(12):1751–7.
Hentic O, Hammel P, Couvelard A, Rebours V, Zappa M, Palazzo M, et al. FOLFIRI regimen: an effective second-line chemotherapy after failure of etoposide-platinum combination in patients with neuroendocrine carcinomas grade 3. Endocr Relat Cancer. 2012;19(6):751–7.
Schwartz MA, Lovett DR, Redner A, Finn RD, Graham MC, Divgi CR, et al. Dose-escalation trial of M195 labeled with iodine 131 for cytoreduction and marrow ablation in relapsed or refractory myeloid leukemias. J Clin Oncol. 1993;11(2):294–303.
Jurcic JG, Larson SM, Sgouros G, McDevitt MR, Finn RD, Divgi CR, et al. Targeted alpha particle immunotherapy for myeloid leukemia. Blood. 2002;100(4):1233–9.
Bodei L, Cremonesi M, Ferrari M, Pacifici M, Grana CM, Bartolomei M, et al. Long-term evaluation of renal toxicity after peptide receptor radionuclide therapy with 90Y-DOTATOC and 177Lu-DOTATATE: the role of associated risk factors. Eur J Nucl Med Mol Imaging. 2008;35(10):1847–56.
Wild D, Frischknecht M, Zhang H, Morgenstern A, Bruchertseifer F, Boisclair J, et al. Alpha- versus beta-particle radiopeptide therapy in a human prostate cancer model (213Bi-DOTA-PESIN and 213Bi-AMBA versus 177Lu-DOTA-PESIN). Cancer Res. 2011;71(3):1009–18.
Cybulla M, Weiner SM, Otte A. End-stage renal disease after treatment with 90Y-DOTATOC. Eur J Nucl Med. 2001;28(10):1552–4.
Strebhardt K, Ullrich A. Paul Ehrlich’s magic bullet concept: 100 years of progress. Nat Rev Cancer. 2008;8(6):473–80.
Apostolidis C, Molinet R, McGinley J, Abbas K, Möllenbeck J, Morgenstern A. Cyclotron production of Ac-225 for targeted alpha therapy. Appl Radiat Isot. 2005;62(3):383–7.
Weidner JW, Mashnik SG, John KD, Ballard B, Birnbaum ER, Bitteker LJ, et al. 225Ac and 223Ra production via 800 MeV proton irradiation of natural thorium targets. Appl Radiat Isot. 2012;70(11):2590–5.
Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fossa SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213–23.
Sgouros G, Roeske JC, McDevitt MR, Palm S, Allen BJ, Fisher DR, et al. MIRD Pamphlet No. 22 (abridged): radiobiology and dosimetry of alpha-particle emitters for targeted radionuclide therapy. J Nucl Med. 2010;51(2):311–28.
Dagle GE, Moen EP, Adee RR, Hui TE, James AC, Filipy RE, et al. Microdistribution and microdosimetry of thorium deposited in the liver. Health Phys. 1992;63(1):41–5.
De Klerk JM, Oyen WJ. The continuous debate in literature about the usage of iodine-131 dosing for the ablation of thyroid remnants and metastases. Minerva Endocrinol. 2009;34(1):57–69.
Wick RR, Nekolla EA, Gaubitz M, Schulte TL. Increased risk of myeloid leukaemia in patients with ankylosing spondylitis following treatment with radium-224. Rheumatology (Oxford). 2008;47(6):855–9.
Sartor O, Reid RH, Bushnell DL, Quick DP, Ell PJ. Safety and efficacy of repeat administration of samarium Sm-153 lexidronam to patients with metastatic bone pain. Cancer. 2007;109(3):637–43.
Morschhauser F, Radford J, Van Hoof A, Botto B, Rohatiner AZ, Salles G, et al. 90Yttrium-ibritumomab tiuxetan consolidation of first remission in advanced-stage follicular non-Hodgkin lymphoma: updated results after a median follow-up of 7.3 years from the International, Randomized, Phase III First-LineIndolent trial. J Clin Oncol. 2013;31(16):1977–83.
Sabet A, Ezziddin K, Pape UF, Ahmadzadehfar H, Mayer K, Poopel T, et al. Long-term hematotoxicity after peptide receptor radionuclide therapy with 177Lu-octreotate. J Nucl Med. 2013;54(11):1857–61.
Acknowledgments
The authors are indebted to the US Department of Energy’s, Office of Nuclear Physics, Isotope Development and Production for Research and Applications Program for providing a portion of 225Ac which was used in these studies. We also thank the involved Interventional Radiologists (especially Ruben Lopez who did most of the interventions) for placing the intra-arterial catheter.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The first two authors C. Kratochwil and F.L. Giesel contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
(PDF 90 kb)
Supplementary Figure 2
(PDF 141 kb)
Supplementary Figure 3
(PDF 171 kb)
Supplementary Figure 4
(PDF 173 kb)
Supplementary Figure 5
(PDF 134 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kratochwil, C., Giesel, F.L., Bruchertseifer, F. et al. 213Bi-DOTATOC receptor-targeted alpha-radionuclide therapy induces remission in neuroendocrine tumours refractory to beta radiation: a first-in-human experience. Eur J Nucl Med Mol Imaging 41, 2106–2119 (2014). https://doi.org/10.1007/s00259-014-2857-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2857-9