Abstract
Background
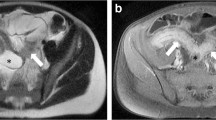
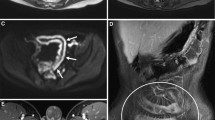
Pediatric inflammatory bowel disease frequently affects the colon. MR enterography is used to assess the small bowel but it also depicts the colon.
Objective
To compare the accuracy of MR enterography and direct visualization at endoscopy in assessing the colon in pediatric inflammatory bowel disease.
Materials and methods
We included children with inflammatory bowel disease who had undergone both MR enterography and endoscopy, and we restrospectively assessed the imaging and endoscopic findings. We scored the colonic appearance at MR using a total colon score. We then compared scores for the whole colon and for its individual segments with endoscopy and histology.
Results
We included 15 children. An elevated MR colonic segmental score predicted the presence of active inflammation on biopsy with a specificity of 90% (95% confidence interval [CI] 79.5–96.2%) and sensitivity of 60% (CI 40.6–77.3%); this compares reasonably with the predictive values for findings at colonoscopy — specificity 85% (CI 73.4—92.9%) and sensitivity 53.3% (CI 34.3%–71.6%). Accuracy did not change significantly with increasing bowel distension.
Conclusion
MR-derived scores had comparable accuracy to those derived during visualization at colonoscopy for detecting biopsy-proven inflammation in our patient group. MR enterography might prove useful in guiding biopsy or monitoring treatment response. Collapse of a colonic segment did not impair assessment of inflammation.



Similar content being viewed by others
References
Shim JO, Seo JK (2014) Very early-onset inflammatory bowel disease (IBD) in infancy is a different disease entity from adult-onset IBD; one form of interleukin-10 receptor mutations. J Hum Genet 59:337–341
Prenzel F, Uhlig HH (2009) Frequency of indeterminate colitis in children and adults with IBD — a metaanalysis. J Crohns Colitis 3:277–281
Mamula P, Telega GW, Markowitz JE et al (2002) Inflammatory bowel disease in children 5 years of age and younger. Am J Gastroenterol 97:2005–2010
Heyman MB, Kirschner BS, Gold BD et al (2005) Children with early-onset inflammatory bowel disease (IBD): analysis of a pediatric IBD consortium registry. J Pediatr 146:35–40
Pigneur B, Escher J, Elawad M et al (2013) Phenotypic characterization of very early-onset IBD due to mutations in the IL10, IL10 receptor alpha or beta gene: a survey of the GENIUS Working Group. Inflamm Bowel Dis 19:2820–2828
Levine A, Koletzko S, Turner D et al (2014) ESPGHAN revised Porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 58:795–806
Sempere GA, Martinez Sanjuan V, Medina Chulia E et al (2005) MRI evaluation of inflammatory activity in Crohn’s disease. AJR Am J Roentgenol 184:1829–1835
Maccioni F, Al Ansari N, Mazzamurro F et al (2014) Detection of Crohn disease lesions of the small and large bowel in pediatric patients: diagnostic value of MR enterography versus reference examinations. AJR Am J Roentgenol 203:W533–W542
Hafeez R, Punwani S, Pendse D et al (2011) Derivation of a T2-weighted MRI total colonic inflammation score (TCIS) for assessment of patients with severe acute inflammatory colitis — a preliminary study. Eur Radiol 21:366–377
Makanyanga JC, Pendsé D, Dikaios N et al (2014) Evaluation of Crohn’s disease activity: initial validation of a magnetic resonance enterography global score (MEGS) against faecal calprotectin. Eur Radiol 24:277–287
Taylor SA, Halligan S, Goh V et al (2003) Optimizing colonic distention for multi-detector row CT colonography: effect of hyoscine butylbromide and rectal balloon catheter. Radiology 229:99–108
Schreyer AG, Rath HC, Kikinis R et al (2005) Comparison of magnetic resonance imaging colonography with conventional colonoscopy for the assessment of intestinal inflammation in patients with inflammatory bowel disease: a feasibility study. Gut 54:250–256
Ajaj W, Pelster G, Treichel U et al (2003) Dark lumen magnetic resonance colonography: comparison with conventional colonoscopy for the detection of colorectal pathology. Gut 52:1738–1743
Rimola J, Ordás I, Rodriguez S et al (2011) Magnetic resonance imaging for evaluation of Crohn’s disease: validation of parameters of severity and quantitative index of activity. Inflamm Bowel Dis 17:1759–1176
Horsthuis K, Bipat S, Bennink RJ et al (2008) Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology 247:64–79
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Barber, J.L., Lozinsky, A.C., Kiparissi, F. et al. Detecting inflammation in the unprepared pediatric colon — how reliable is magnetic resonance enterography?. Pediatr Radiol 46, 646–652 (2016). https://doi.org/10.1007/s00247-015-3538-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3538-y