Abstract
Introduction
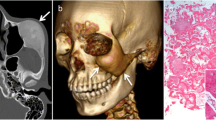
The present study aimed to assess the craniofacial CT imaging features for differentiating between Gorham–Stout disease (GSD) and generalized lymphatic anomaly (GLA).
Methods
Seven patients with GSD and four patients with GLA were included in this study. All patients underwent CT examinations that encompassed the craniofacial bones. The presence, distribution, and type of craniofacial osteolysis were assessed. The clinical symptoms that were associated with craniofacial osteolysis were also reviewed.
Results
Craniofacial osteolysis including cranial osteolysis was seen in four of seven (57 %) patients with GSD and in three of four (75 %) patients with GLA. Facial osteolysis was seen in two (29 %) patients with GSD, but this was not observed in patients with GLA. Among patients with craniofacial osteolysis, those with GSD showed diffuse involvement, whereas those with GLA showed multifocal involvement. The craniofacial osteolysis of GSD could be classified into three patterns: medullary involvement, thinning bone, and disappearing bone. The clinical symptoms of craniofacial osteolysis were observed in all patients with GSD but were not present in patients with GLA.
Conclusion
Craniofacial involvement was observed in both groups. The craniofacial osteolysis of GSD showed diffuse involvement with clinical symptoms, whereas that of GLA showed multifocal involvement without clinical symptoms.





Similar content being viewed by others
References
Wassef M, Blei F, Adams D, Alomari A, Baselga E, Berenstein A, Burrows P, Frieden IJ, Garzon MC, Lopez-Gutierrez JC, Lord DJ, Mitchel S, Powell J, Prendiville J, Vikkula M, Board I, Scientific C (2015) Vascular anomalies classification: recommendations from the international society for the study of vascular anomalies. Pediatrics 136(1):e203–214. doi:10.1542/peds.2014-3673
Pastakia B, Horvath K, Lack EE (1987) Seventeen year follow-up and autopsy findings in a case of massive osteolysis. Skelet Radiol 16(4):291–297
Gorham LW, Stout AP (1955) Massive osteolysis (acute spontaneous absorption of bone, phantom bone, disappearing bone): its relation to hemangiomatosis. J Bone Joint Surg Am 37-A(5):985–1004
Gorham LW, Wright AW, Shultz HH, Maxon FC Jr (1954) Disappearing bones: a rare form of massive osteolysis; report of two cases, one with autopsy findings. Am J Med 17(5):674–682
Johnson PM, Mc CJ (1958) Observations on massive osteolysis: a review of the literature and report of a case. Radiology 71(1):28–42. doi:10.1148/71.1.28
Radhakrishnan K, Rockson SG (2008) Gorham’s disease: an osseous disease of lymphangiogenesis? Ann N Y Acad Sci 1131:203–205. doi:10.1196/annals.1413.022
Dellinger MT, Garg N, Olsen BR (2014) Viewpoints on vessels and vanishing bones in Gorham-Stout disease. Bone 63:47–52. doi:10.1016/j.bone.2014.02.011
Rossler J, Saueressig U, Kayser G, von Winterfeld M, Klement GL (2015) Personalized therapy for generalized lymphatic anomaly/Gorham-Stout disease with a combination of sunitinib and taxol. J Pediatr Hematol Oncol 37(8):e481–485. doi:10.1097/MPH.0000000000000436
Alvarez OA, Kjellin I, Zuppan CW (2004) Thoracic lymphangiomatosis in a child. J Pediatr Hematol Oncol 26(2):136–141
Lala S, Mulliken JB, Alomari AI, Fishman SJ, Kozakewich HP, Chaudry G (2013) Gorham-Stout disease and generalized lymphatic anomaly—clinical, radiologic, and histologic differentiation. Skelet Radiol 42(7):917–924. doi:10.1007/s00256-012-1565-4
Diaz-Ramon C, Fernandez-Latorre F, Revert-Ventura A, Mas-Estelles F, Domenech-Iglesias A, Lazaro-Ventura A (1996) Idiopathic progressive osteolysis of craniofacial bones. Skelet Radiol 25(3):294–297
Frankel DG, Lewin JS, Cohen B (1997) Massive osteolysis of the skull base. Pediatr Radiol 27(3):265–267. doi:10.1007/s002470050120
Lo CP, Chen CY, Chin SC, Juan CJ, Hsueh CJ, Chen A (2004) Disappearing calvarium in Gorham disease: MR imaging characteristics with pathologic correlation. AJNR Am J Neuroradiol 25(3):415–418
Raghuveer HP, Jayalekshmy R (2009) Gorham’s massive osteolysis of the mandible—a progressive radiographic presentation. Dentomaxillofac Radiol 38(5):292–295. doi:10.1259/dmfr/73198793
Perschbacher SE, Perschbacher KA, Pharoah MJ, Bradley G, Lee L, Yu E (2010) Gorham’s disease of the maxilla: a case report. Dentomaxillofac Radiol 39(2):119–123. doi:10.1259/dmfr/52099930
Adler F, Gupta N, Hess CP, Dowd CF, Dillon WP (2011) Intraosseous CSF fistula in a patient with Gorham disease resulting in intracranial hypotension. AJNR Am J Neuroradiol 32(11):E198–200. doi:10.3174/ajnr.A2413
Reddy S, Jatti D (2012) Gorham’s disease: a report of a case with mandibular involvement in a 10-year follow-up study. Dentomaxillofac Radiol 41(6):520–524. doi:10.1259/dmfr/93696387
Brouillard P, Boon L, Vikkula M (2014) Genetics of lymphatic anomalies. J Clin Invest 124(3):898–904. doi:10.1172/JCI71614
Kotecha R, Mascarenhas L, Jackson HA, Venkatramani R (2012) Radiological features of Gorham’s disease. Clin Radiol 67(8):782–788. doi:10.1016/j.crad.2012.01.009
Ozeki M, Fujino A, Matsuoka K, Nosaka S, Kuroda T, Fukao T (2016) Clinical features and prognosis of generalized lymphatic anomaly, kaposiform lymphangiomatosis, and Gorham-Stout disease. Pediatr Blood Cancer 63(5):832–838. doi:10.1002/pbc.25914
Heritier S, Le Merrer M, Jaubert F, Bigorre M, Gillibert-Yvert M, de Courtivron B, Ziade M, Bertrand Y, Carrie C, Chastagner P, Bost-Bru C, Leonard JC, Ouache M, Boccon-Gibod L, Mary P, de Blic J, Pin I, Wendling D, Revillon Y, Houdoin V, Forin V, Lepointe HD, Languepin J, Wagnon J, Epaud R, Fauroux B, Donadieu J (2010) Retrospective French nationwide survey of childhood aggressive vascular anomalies of bone, 1988–2009. Orphanet J Rare Dis 5:3. doi:10.1186/1750-1172-5-3
Hassanein AH, Mulliken JB, Fishman SJ, Quatrano NA, Zurakowski D, Greene AK (2012) Lymphatic malformation: risk of progression during childhood and adolescence. J Craniofac Surg 23(1):149–152. doi:10.1097/SCS.0b013e3182413ea8
Liu Y, Zhong DR, Zhou PR, Lv F, Ma DD, Xia WB, Jiang Y, Wang O, Xing XP, Li M (2014) Gorham-Stout disease: radiological, histological, and clinical features of 12 cases and review of literature. Clin Rheumatol. doi:10.1007/s10067-014-2780-2
Campbell J, Almond HG, Johnson R (1975) Massive osteolysis of the humerus with spontaneous recovery. J Bone Joint Surg (Br) 57(2):238–240
Hu P, Yuan XG, Hu XY, Shen FR, Wang JA (2013) Gorham-Stout syndrome in mainland China: a case series of 67 patients and review of the literature. J Zhejiang Univ Sci B 14(8):729–735. doi:10.1631/jzus.B1200308
Joshi M, Phansalkar DS (2015) Simple lymphangioma to generalized lymphatic anomaly: role of imaging in disclosure of a rare and morbid disease. Case Rep Radiol 2015:603859. doi:10.1155/2015/603859
ACR–ASNR–SPR (2011) Practice parameter for the performance of computed tomography (CT) of the extracranial head and neck. Resolution 33, Amended 2014 (Resolution 39):1–11
Patel DV (2005) Gorham’s disease or massive osteolysis. Clin Med Res 3(2):65–74
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that all human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Conflict of interest
We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kato, H., Ozeki, M., Fukao, T. et al. Craniofacial CT findings of Gorham–Stout disease and generalized lymphatic anomaly. Neuroradiology 58, 801–806 (2016). https://doi.org/10.1007/s00234-016-1691-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-016-1691-0