Abstract
Introduction
The aim of this study is to evaluate the utility of relative cerebral blood volume (rCBV) data from dynamic susceptibility contrast (DSC) perfusion in grading pediatric primary brain tumors.
Methods
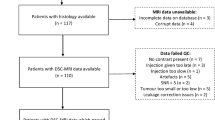
A retrospective blinded review of 63 pediatric brain tumors with DSC perfusion was performed independently by two neuroradiologists. A diagnosis of low- versus high-grade tumor was obtained from conventional imaging alone. Maximum rCBV (rCBVmax) was measured from manual ROI placement for each reviewer and averaged. Whole-tumor CBV data was obtained from a semi-automated approach. Results from all three analyses were compared to WHO grade.
Results
Based on conventional MRI, the two reviewers had a concordance rate of 81 % (k = 0.62). Compared to WHO grade, the concordant cases accurately diagnosed high versus low grade in 82 %. A positive correlation was demonstrated between manual rCBVmax and tumor grade (r = 0.30, P = 0.015). ROC analysis of rCBVmax (area under curve 0.65, 0.52–0.77, P = 0.03) gave a low-high threshold of 1.38 with sensitivity of 92 % (74–99 %), specificity of 40 % (24–57 %), NPV of 88 % (62–98 %), and PPV of 50 % (35–65 %) Using this threshold on 12 discordant tumors between evaluators from conventional imaging yielded correct diagnoses in nine patients. Semi-automated analysis demonstrated statistically significant differences between low- and high-grade tumors for multiple metrics including average rCBV (P = 0.027).
Conclusions
Despite significant positive correlation with tumor grade, rCBV from pediatric brain tumors demonstrates limited specificity, but high NPV in excluding high-grade neoplasms. In selective patients whose conventional imaging is nonspecific, an rCBV threshold may have further diagnostic value.




Similar content being viewed by others
References
Law M, Yang S, Wang H et al (2003) Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. AJNR Am J Neuroradiol 24:1989–1998
Bulakbasi N, Kocaoglu M, Farzaliyev A et al (2005) Assessment of diagnostic accuracy of perfusion MR imaging in primary and metastatic solitary malignant brain tumors. AJNR Am J Neuroradiol 26:2187–2199
Law M, Young R, Babb J et al (2007) Histogram analysis versus region of interest analysis of dynamic susceptibility contrast perfusion MR imaging data in the grading of cerebral gliomas. AJNR Am J Neuroradiol 28:761–766
Shin J, Lee H, Kwun B et al (2002) Using relative cerebral blood flow and volume to evaluate the histopathologic grade of cerebral gliomas: preliminary results. Am J Roentgenol 179:783–789
Law M, Young R, Babb J et al (2006) Comparing perfusion metrics obtained from a single compartment versus pharmacokinetic modeling methods using dynamic susceptibility contrast-enhanced perfusion MR imaging with glioma grade. AJNR Am J Neuroradiol 27:1975–1982
Fan G, Deng Q, Wu Z, Guo Q (2006) Usefulness of diffusion/perfusion-weighted MRI in patients with non-enhancing supratentorial brain gliomas: a valuable tool to predict tumour grading? Br J Radiol 79:652–658
Morita N, Wang S, Chawla S et al (2010) Dynamic susceptibility contrast perfusion weighted imaging in grading of nonenhancing astrocytomas. J Magn Reson Imaging 32(4):803–808
Boxerman J, Schmainda K, Weisskoff R (2006) Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol 27:859–67
Ball W Jr, Holland S (2001) Perfusion imaging in the pediatric patient. Magn Reson Imaging Clin N Am 9:207–230
Yeom K, Mitchell L, Lober R et al (2014) Arterial spin-labeled perfusion of pediatric brain tumors. AJNR Am J Neuroradiol 35(2):395–401. doi:10.3174/ajnr.A3670
Koeller K, Rushing E (2004) From the archives of the AFIP: pilocytic astrocytoma: radiologic-pathologic correlation. Radiographics 24:1693–1708
Brat D, Scheithauer B, Fuller G, Tihan T (2007) Newly codified glial neoplasms of the 2007 WHO classification of tumours of the central nervous system: angiocentric glioma, pilomyxoid astrocytoma and pituicytoma. Brain Pathol 17:319–324
Lev M, Ozsunar Y, Henson J et al (2004) Glial tumor grading and outcome prediction using dynamic spin-echo MR susceptibility mapping compared with conventional contrast-enhanced MR: confounding effect of elevated rCBV of oligodendrogliomas. AJNR Am J Neuroradiol 25:214–221
Xu M, See S, Ng W et al (2005) Comparison of magnetic resonance spectroscopy and perfusion-weighted imaging in presurgical grading of oligodendroglial tumors. Neurosurgery 56:919–926
Kool M, Korshunov A, Remke M et al (2012) Molecular subgroups of medulloblastoma: an international meta-analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, group 3, and group 4 medulloblastomas. Acta Neuropathol 123(4):473–84. doi:10.1007/s00401-012-0958-8
Cha S (2006) Dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging in pediatric patients. Neuroimaging Clin N Am 16(1):137–147
Grand S, Kremer S, Tropres I et al (2007) Perfusion-sensitive MRI of pilocytic astrocytomas: initial results. Neuroradiology 49(7):545–550
Yuh E, Barkovich A, Gupta N (2009) Imaging of ependymomas: MRI and CT. Childs Nerv Syst 25:1203–1213
Sentürk S, Oğuz K, Cila A (2009) Dynamic contrast enhanced susceptibility-weighted perfusion imaging of intracranial tumors: a study using a 3 T MR scanner. Diagn Interv Radiol 15:3–12
Lev MH, Rosen BR (1999) Clinical applications of intracranial perfusion MR imaging. Neuroimaging Clin N Am 9:309–331
Darpolor MM, Molthen RC, Schmainda KM (2011) Multimodality imaging of abnormal vascular perfusion and morphology in preclinical 9L gliosarcoma model. PLoS One 6(1):e16621
Quarles CC, Krouwer HG, Rand SD, Schmainda KM (2005) Dexamethasone normalizes brain tumor hemodynamics as indicated by dynamic susceptibility contrast MRI perfusion parameters. Technol Cancer Res Treat 4(3):245–9
Wilkinson ID, Jellineck DA, Levy D et al (2006) Dexamethasone and enhancing solitary cerebral mass lesions: alterations in perfusion and blood-tumor barrier kinetics shown by magnetic resonance imaging. Neurosurgery 58(4):640–6
Armitage PA, Schwindack C, Bastin ME, Whittle IR (2007) Quantitative assessment of intracranial tumor response to dexamethasone using diffusion, perfusion and permeability magnetic resonance imaging. Magn Reson Imaging 25(3):303–10
Bastin ME, Carpenter TK, Armitage PA et al (2006) Effects of dexamethasone on cerebral perfusion and water diffusion in patients with high-grade glioma. AJNR Am J Neuroradiol 27(2):402–8
Ethical standards and patient consent
We declare that this manuscript does not contain clinical studies or identifiable patient data, and therefore, the Institutional Review Board of Indiana University waived consent.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ho, C.Y., Cardinal, J.S., Kamer, A.P. et al. Relative cerebral blood volume from dynamic susceptibility contrast perfusion in the grading of pediatric primary brain tumors. Neuroradiology 57, 299–306 (2015). https://doi.org/10.1007/s00234-014-1478-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1478-0