Abstract
Introduction
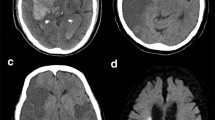
Patients receiving intravenous thrombolysis with recombinant tissue plasminogen activator (IVT) for ischemic stroke are monitored in an intensive care unit (ICU) or a comparable unit capable of ICU interventions due to the high frequency of standardized neurological exams and vital sign checks. The present study evaluates quantitative infarct volume on early post-IVT MRI as a predictor of critical care needs and aims to identify patients who may not require resource intense monitoring.
Methods
We identified 46 patients who underwent MRI within 6 h of IVT. Infarct volume was measured using semiautomated software. Logistic regression and receiver operating characteristics (ROC) analysis were used to determine factors associated with ICU needs.
Results
Infarct volume was an independent predictor of ICU need after adjusting for age, sex, race, systolic blood pressure, NIH Stroke Scale (NIHSS), and coronary artery disease (odds ratio 1.031 per cm3 increase in volume, 95 % confidence interval [CI] 1.004–1.058, p = 0.024). The ROC curve with infarct volume alone achieved an area under the curve (AUC) of 0.766 (95 % CI 0.605–0.927), while the AUC was 0.906 (95 % CI 0.814–0.998) after adjusting for race, systolic blood pressure, and NIHSS. Maximum Youden index calculations identified an optimal infarct volume cut point of 6.8 cm3 (sensitivity 75.0 %, specificity 76.7 %). Infarct volume greater than 3 cm3 predicted need for critical care interventions with 81.3 % sensitivity and 66.7 % specificity.
Conclusion
Infarct volume may predict needs for ICU monitoring and interventions in stroke patients treated with IVT.


Similar content being viewed by others
References
Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, Brott T, Frankel M, Grotta JC, Haley EC Jr, Kwiatkowski T, Levine SR, Lewandowski C, Lu M, Lyden P, Marler JR, Patel S, Tilley BC, Albers G, Bluhmki E, Wilhelm M, Hamilton S, ATLANTIS Trials Investigators, ECASS Trials Investigators, NINDS rt-PA Study Group Investigators (2004) Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 363:768–774
Ronning OM, Guldvog B (1998) Stroke unit versus general medical wards, II: neurological deficits and activities of daily living: a quasi-randomized controlled trial. Stroke 29:586–590
Indredavik B, Bakke F, Solberg R, Rokseth R, Haaheim LL, Holme I (1991) Benefit of a stroke unit: a randomized controlled trial. Stroke 22:1026–1031
Ringelstein EB, Chamorro A, Kaste M, Langhorne P, Leys D, Lyrer P, Thijs V, Thomassen L, Toni D, ESO Stroke Unit Certification Committee (2013) European Stroke Organisation recommendations to establish a stroke unit and stroke center. Stroke 44:828–840
Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, Khatri P, McMullan PW Jr, Qureshi AI, Rosenfield K, Scott PA, Summers DR, Wang DZ, Wintermark M, Yonas H, American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Peripheral Vascular Disease, Council on Clinical Cardiology (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44:870–947
Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP, DELAY-ED study group (2007) Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 35:1477–1483
Faigle R, Sharrief A, Marsh EB, Llinas RH, Urrutia VC (2014) Predictors of critical care needs after IV thrombolysis for acute ischemic stroke. PLoS One 9:e88652
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Larrue V, von Kummer RR, Muller A, Bluhmki E (2001) Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke 32:438–441
Dardzinski BJ, Sotak CH, Fisher M, Hasegawa Y, Li L, Minematsu K (1993) Apparent diffusion coefficient mapping of experimental focal cerebral ischemia using diffusion-weighted echo-planar imaging. Magn Reson Med 30:318–325
Schaefer PW, Hassankhani A, Putman C, Sorensen AG, Schwamm L, Koroshetz W, Gonzalez RG (2004) Characterization and evolution of diffusion MR imaging abnormalities in stroke patients undergoing intra-arterial thrombolysis. AJNR Am J Neuroradiol 25:951–957
Saver JL, Johnston KC, Homer D, Wityk R, Koroshetz W, Truskowski LL, Haley EC (1999) Infarct volume as a surrogate or auxiliary outcome measure in ischemic stroke clinical trials. RANTTAS Investigators Stroke 30:293–298
Olavarria VV, Delgado I, Hoppe A, Brunser A, Carcamo D, Diaz-Tapia V, Lavados PM (2011) Validity of the NIHSS in predicting arterial occlusion in cerebral infarction is time-dependent. Neurology 76:62–68
Kruetzelmann A, Kohrmann M, Sobesky J, Cheng B, Rosenkranz M, Rother J, Schellinger PD, Ringleb P, Gerloff C, Fiehler J, Thomalla G (2011) Pretreatment diffusion-weighted imaging lesion volume predicts favorable outcome after intravenous thrombolysis with tissue-type plasminogen activator in acute ischemic stroke. Stroke 42:1251–1254
Purushotham A, Campbell BC, Straka M, Mlynash M, Olivot JM, Bammer R, Kemp SM, Albers GW, Lansberg MG (2013) Apparent diffusion coefficient threshold for delineation of ischemic core. Int J Stroke. doi:10.1111/ijs.12068
Wheeler HM, Mlynash M, Inoue M, Tipirneni A, Liggins J, Zaharchuk G, Straka M, Kemp S, Bammer R, Lansberg MG, Albers GW, DEFUSE 2 Investigators (2013) Early diffusion-weighted imaging and perfusion-weighted imaging lesion volumes forecast final infarct size in DEFUSE 2. Stroke 44:681–685
Lansberg MG, Lee J, Christensen S, Straka M, De Silva DA, Mlynash M, Campbell BC, Bammer R, Olivot JM, Desmond P, Davis SM, Donnan GA, Albers GW (2011) RAPID automated patient selection for reperfusion therapy: a pooled analysis of the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET) and the Diffusion and Perfusion Imaging Evaluation for Understanding Stroke Evolution (DEFUSE) Study. Stroke 42:1608–1614
Acknowledgments
RF was supported by an R25 Grant-NIH/NINDS Research Education Program for Residents and Fellows in Neurology and Neurosurgery.
Ethical standards and patient consent
We declare that all human studies have been approved by the Johns Hopkins University School of Medicine Institutional Review Board (IRB) and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that we are permitted to use and disclose protected health information in our stroke database via an IRB-approved HIPAA waiver of the requirement for patients’ authorization.
Conflict of interest
VCU is the PI for the investigator initiated trial SAIL ON (a pilot clinical trial of IVT treatment for patients that wake up with stroke); Genentec Inc. has provided funding for this trial. VCU is the PI at Johns Hopkins for the multicenter clinical trial DIAS 4, sponsored by Lundbeck. We declare that there are no patents, products in development, or marketed products.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Faigle, R., Wozniak, A.W., Marsh, E.B. et al. Infarct volume predicts critical care needs in stroke patients treated with intravenous thrombolysis. Neuroradiology 57, 171–178 (2015). https://doi.org/10.1007/s00234-014-1453-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1453-9