Abstract
Introduction
Bedside swallowing assessments are often used to assess dysphagia. However, in some patients, aspiration pneumonia occurs without any problems on bedside swallowing assessments and some patients do not suffer aspiration pneumonia despite abnormal results of bedside swallowing assessments in acute stroke. To detect the differences of lesions related to bedside swallowing assessment abnormality and aspiration, we investigated swallowing-related functional lesions in terms of cerebral blood flow in patients with dysphagia after stroke.
Methods
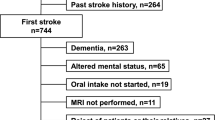
The study included 50 acute stroke patients who underwent bedside swallowing assessments and videofluorography as well as single-photon emission computed tomography (CT) at approximately the same time. Bedside swallowing assessments included repetitive saliva swallowing test and modified water swallowing test as dry and wet swallowing tasks. The presence or absence of aspiration was assessed using videofluorography. We divided patients into three subgroups based on the outcomes of the bedside swallowing assessments and presence or absence of aspiration. Statistical image analysis was performed using single-photon emission CT to determine their relationship with bedside swallowing assessments and videofluorography results.
Results
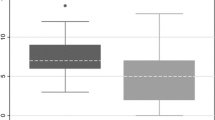
Twenty-seven (54.0 %) and 28 (56.0 %) patients had abnormal repetitive saliva swallowing test and modified water swallowing test results. Videofluorography indicated aspiration in 35 (70.0 %) patients. In comparing patients with and without abnormal results on each test, the groups with abnormal repetitive saliva swallowing test, abnormal modified water swallowing test, and aspiration demonstrated lower cerebral blood flow in the left precuneus, left insula, and anterior cingulate gyrus, respectively.
Conclusions
Based on the analysis of cerebral blood flow, functional lesions differed across abnormal repetitive saliva swallowing test and abnormal modified water swallowing test findings and aspiration on videofluorography, and each test may assess different functions among the many processes involved in swallowing.




Similar content being viewed by others
References
Gordon C, Hewer RL, Wade DT (1987) Dysphagia in acute stroke. BMJ (Clin Res Ed) 295:411–414
Horner J, Massey EW (1988) Silent aspiration following stroke. Neurology 38:317–319
Smithard DG, O'Neill PA, Parks C, Morris J (1996) Complications and outcome after acute stroke: does dysphagia matter? Stroke 27:1200–1204
Ickenstein GW, Stein J, Ambrosi D, Goldstein R, Horn M, Bogdahn U (2005) Predictors of survival after severe dysphagic stroke. J Neurol 252:1510–1516
Kedlaya D, Brandstater ME (2002) Swallowing, nutrition and hydration during acute stroke care. Top Stroke Rehabil 9:23–28
Rosenvinge SK, Starke ID (2005) Improving care for patients with dysphagia. Age Ageing 34:587–593
Yoo SH, Kim JS, Kwon SU, Yun SC, Koh JY, Kang DW (2008) Undernutrition as a predictor of poor clinical outcome in acute ischemic stroke patients. Arch Neurol 65:39–43
Marques CHD, de Rosso ALZ, Andre C (2008) Bedside assessment of swallowing in stroke: water tests are not enough. Top Stroke Rehabil 15:378–383
DePippo KL, Holas MA, Reding MJ (1992) Validation of the 3-oz water swallow test for aspiration following stroke. Arch Neurol 49:1259–1261
Gottlieb D, Kipnis M, Sister E, Vardi Y, Brill S (1996) Validation of the 50 ml3 drinking test for evaluation of post-stroke dysphagia. Disabil Rehabil 18:529–532
Oguchi K, Saitoh E, Baba M, Kusudo M, Tanaka T, Onogi K (2000) The repetitive saliva swallowing test (RSST) as a screening test of functional dysphagia (2). Validity of RSST. Jpn J Rehabil Med 38:383–388
Tohara H, Saitoh E, Mays KA, Kuhlemeier K, Palmer JB (2003) Three tests for predicting aspiration without videofluorography. Dysphagia 18:126–134
Smithard DG, O’Neill PA, Park C, England R, Renwick DS, Wyatt R, Morris J, Martin DF (1998) Can bedside assessment reliably exclude aspiration following acute stroke? Age Ageing 27:99–106
Trapl M, Enderle P, Nowotny M, Teuschi Y, Mats K, Dachenhausen A, Brainin M (2007) Dysphagia bedside screening for acute-stroke patients: the Gugging Swallowing Screen. Stroke 38:2948–2952
Horner J, Buoyer FG, Alberts MJ, Helms MJ (1991) Dysphagia following brain-stem stroke: clinical correlates and outcome. Arch Neurol 48:1170–1173
Daniels SK, Foundas AL (1997) The role of the insular cortex in swallowing. Dysphagia 12:146–156
Steinhagen V, Grossmann A, Benecke R, Walter U (2009) Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke 40:1903–1906
Martin RE, Goodyear BG, Gati JS, Menon RS (2001) Cerebral cortical representation of automatic and volitional swallowing in humans. J Neurophysiol 85:938–950
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL (2010) Relevance of subcortical stroke in dysphagia. Stroke 41:482–486
Li S, Luo C, Yu B, Yan B, Gong Q, He C, He L, Huang X, Yao D, Lui S, Tang H, Chen Q, Zeng Y, Zhou D (2009) Functional magnetic resonance imaging study on dysphagia after unilateral hemispheric stroke: a preliminary study. J Neurol Neurosurg Psychiatry 80:1320–1329
Shinohara Y, Yanagihara T, Abe K, Yoshimina T, Fujinaka T, Chuma T, Ochi F, Nagayama M, Ogawa A, Suzuki N, Katayama Y, Kimura A, Liu M, Eto F (2011) VII. Rehabilitation. J Stroke Cerebrovasc Dis 20:S145–S180
Tsubahara A, Tanimoto K, Baba M (2004) Standard method for videofluorography: the Japanese Society of Dysphagia Rehabilitation. JJDR (Japanese Journal of Dysphagia Rehabilitation) 8:71–86
Matsuda H, Yagishita A, Tsuji S, Hisada K (1995) A quantitative approach to technetium-99 m ethyl cysteinate dimer: a comparison with technetium-99 m hexamethylpropylene amine oxime. Eur J Nuc Med 22:633–637
Friston KJ, Holmes AP, Worsley KJ, Poline JP, Frith CD, Frackowiak RS (1995) Statistical parametric maps in functional imaging. Hum Brain Map 2:189–210
Côté R, Hachinski VC, Shurvell BL, Norris JW, Wolfson C (1986) The Canadian Neurological Scale: a preliminary study in acute stroke. Stroke 17:731–737
Lewell SY, Reynolds RC, Chen G, Horwitz B, Ludlow CL (2012) Functional connectivity and laterality of the motor and sensory components in the volitional swallowing network. Exp Brain Res 219:85–96
Meng NH, Wang TG, Lien IN (2000) Dysphagia in patients with brainstem stroke: incidence and outcome. Am J Phys Med Rehabil 79:170–175
Meadows JC (1973) Dysphagia in unilateral cortical lesions. J Neurol Neurosurg Psychiatry 38:853–860
Jacobson DL, Bica I, Knox TA, Wanke C, Tchetgen E, Spiegelman D, Silva M, Gorbach S, Wilson IB (2003) Difficulty swallowing and lack of receipt of highly active antiretroviral therapy predict acute weight loss in human immunodeficiency virus disease. Clin Infect Dis 37:1349–1356
Okamura N, Maruyama M, Ebihara T, Matsui T, Nemoto M, Arai H, Sasaki H, Yanai K (2004) Aspiration pneumonia and insular hypoperfusion in patients with cerebrovascular disease. J Am Geriatr Soc 52:645–646
Schroeder MF, Daniels SK, McClain M, Corey DM, Fondas AL (2006) Clinical and cognitive predictors of swallowing recovery in stroke. J Rhabil Res and Development 43:301–303
Sellars C, Bowie L, Bagg J, Sweeney P, Miller H, Tinlston J, Langhorne P, Stott DJ (2007) Risk factors for chest infection in acute stroke: a prospective cohort study. Stroke 38:2284–2291
Matsuda H, Mizumura S, Nagao T, Ota T, Iizuka T, Nemoto K, Takemura N, Arai H, Homma A (2007) Automated discrimination between very early Alzheimer disease and controls using an easy Z-score imaging system for multicenter brain perfusion single photon emission tomography. Am J Neuroradiol 28:731–736
Daniels SK, Foundas AL, Iglesia GC, Sullivan MA (1996) Lesion site in unilateral stroke patients with dysphagia. J Stroke Cerebrovasc Dis 6:30–34
Soros P, Lalone E, Smith R, Stevens T, Theurer J, Menon RS, Martin RE (2008) Functional MRI of oropharyngeal air-pulse stimulation. Neurosci 153:1300–1308
Warabi T, Ito T, Kato M, Takei H, Kobayashi N, Chiba S (2008) Effects of stroke-induced damage to swallow-related areas in the brain on swallowing mechanics of elderly patients. Geriatr Gerontol Int 8:234–242
Geldberg G (1985) Supplementary motor area structure and function: review and hypothesis. Behav Brain Sci 8:567–615
Watanabe Y, Abe S, Ishikawa T, Yamada Y, Yamane GY (2004) Cortical regulation during the early stage of initiation of voluntary swallowing in humans. Dysphagia 19:100–108
Hamdy S, Milkulis DJ, Crawley A, Xue S, Lau H, Henry S, Diamant NE (1999) Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Physiol 277:G219–225
Maeshima S, Osawa A, Takajo F, Kurozumi S, Ota N, Kumakura I (2007) A comparison study of aspiration with clinical manifestations in stroke patients. Brain Nerve (Tokyo) 59:521–526
Ramsey DJ, Smithard DG, Kalra L (2003) Early assessments of dysphagia and aspiration risk in acute stroke patients. Stroke 34:1252–1257
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Repetitive saliva swallowing test
The RSST is an assessment of the patient’s potential to swallow saliva. Patients were instructed by verbal command (sometimes by gesture) to swallow the saliva repeatedly for 30 s (forced swallowing). Based on the upper limit of cumulative swallowing rates in the elderly, twice or less per 30 s was defined as the screening value [11].
Modified water swallowing test
For the MWST, cold water (3 ml) was placed on the floor of the mouth using a 5-ml syringe; placement on the floor of the mouth prevented premature spillage into the pharynx. Patients were then instructed to swallow. If the patient was unable to swallow or experienced dyspnea, coughing, or wet–hoarse dysphonia after swallowing, a score was recorded (1 for inability to swallow, 2 for dyspnea, and 3 for cough or dysphonia), and the test was terminated. Otherwise, the patient was asked to perform two dry (saliva) swallows. If the patient was able to swallow the water but unable to perform either of the two dry swallows, a score of 4 was recorded. If the patient was able to complete the water and both dry swallows, a score of 5 was recorded. The entire procedure was repeated twice over, and the final score was defined as the lowest score on any trial. Ratings of 4 and 5 that represent no coughing or moist hoarseness after swallowing of water are normal [12].
Rights and permissions
About this article
Cite this article
Osawa, A., Maeshima, S., Matsuda, H. et al. Functional lesions in dysphagia due to acute stroke: discordance between abnormal findings of bedside swallowing assessment and aspiration on videofluorography. Neuroradiology 55, 413–421 (2013). https://doi.org/10.1007/s00234-012-1117-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-012-1117-6