Abstract
Purpose
The study aimed to (1) determine the trends in the utilisation of metformin in Australia, (2) determine the appropriateness of metformin dosing in an Australian teaching hospital and (3) gather the opinions of prescribers on the relationship between metformin dose and renal function.
Methods
National prescription data between 1990 and 2012 were accessed. A retrospective audit (2008–2012) of metformin doses and patient renal function (20 % random sample of all in-patients prescribed metformin) was conducted at St Vincent’s Hospital (SVH), Sydney. Prescribers of metformin were interviewed (semi-structured; consultants at SVH) or surveyed (Australian endocrinologists) to gather their understanding of metformin dosing in relation to renal function.
Results
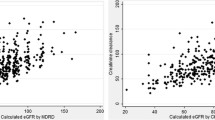
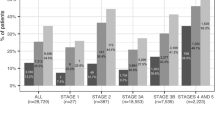
Metformin utilisation increased fivefold nationally between 1995 and 2012. Metformin tended to be under-dosed in SVH patients with normal renal function (83.5 %) and over-dosed in patients with impaired renal function (estimated glomerular filtration rate (eGFR) <30 mL/min, 50 %). Consultants indicated that metformin doses needed to be reduced in renal impairment. Most endocrinologists (61 %) were comfortable prescribing metformin down to eGFRs around 30 mL/min.
Conclusion
The use of metformin increased greatly over the period of the study. Metformin is prescribed frequently for patients with eGFR values below the minimal level approved in the product label (60 mL/min). While prescribers expressed their understanding of the need to reduce metformin doses in patients with renal impairment, we found that metformin doses were higher than appropriate in patients with impaired renal function. Metformin may be used safely when renal function is poor provided dosage is appropriately reduced.

Similar content being viewed by others
Notes
Subsidised: government pays difference between patient co-payments and cost of drug. For metformin, this applies to concessionary patients namely those aged over 65 years and those with sickness benefits and from a low socio-economic background. Unsubsidised: government pays nothing, applies to non-concessionary patients
Under copayment data began to be incorporated in Medicare data late in 2012 but was not included in the Medicare data accessed for this study.
Administrations for which the corresponding orders spanned the annual cutoff (December 31) into the successive year were counted in the year in which the order was made.
References
Shenfield G (2013) Metformin: myths, misunderstandings and lessons from history. Aust Prescr 36:38–39
Group UPDSU (1998) Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352(9131):854–865
(2014) Executive summary: standards of medical care in diabetes—2014. Diabetes Care 37(Suppl 1):S5–S13
Davoren P (2014) Safe prescribing of metformin in diabetes. Aust Prescr 37:2–5
Inzucchi SE, Lipska KJ, Mayo H, Bailey CJ, McGuire DK (2014) Metformin in patients with type 2 diabetes and kidney disease: a systematic review. JAMA 312(24):2668–2675
Rossi S (2013) Australian medicines handbook 2013. https://amhonline.amh.net.au/
Administration FaD (2016) FDA drug safety communication: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function. Silver Spring. [Available from: http://www.fda.gov/downloads/Drugs/DrugSafety/UCM494140.pdf
Excellence NIoC (2015) Type 2 diabetes in adults: management. London. [Available from: https://www.nice.org.uk/guidance/ng28/chapter/1-Recommendations#drug-treatment-2
MedSafe (2015) Renal impairment and risk of lactic acidosis. Prescriber Update 36(4):56–57
Huang W, Peterson GM, Zaidi ST, Castelino RL (2015) Metformin utilisation in Australian community and aged care settings. Diabetes Res Clin Pract 108(2):336–341
Duong J, Roberts D, Furlong T, Kumar S, Greenfield J, Kirkpatrick C, et al. (2012) Metformin therapy in patients with chronic kidney disease. Diabetes, Obesity and Metabolism 14(10):963–965
Duong JK, Kumar SS, Kirkpatrick CM, Greenup LC, Arora M, Lee TC, et al. (2013) Population pharmacokinetics of metformin in healthy subjects and patients with type 2 diabetes mellitus: simulation of doses according to renal function. Clin Pharmacokinet 52(5):373–384
Webbie K, O'Brien K (2006) Use of medicines by Australians with diabetes, cat. no. AUS 82. AIHW, Canberra [Available from: http://www.aihw.gov.au/publication-detail/?id=6442467875
Australian Institute of Health and Welfare (AIHW) (2008) [Available from: http://www.aihw.gov.au/publication-detail/?id=6442468075 Diabetes: Australian facts 2008, cat. no. CVD 40. AIHW, Canberra
Australian Bureau of Statistics (ABS) (2012) Australian health survey: first results 2011–12. Cited 8 Dec 2014. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.001main+features12011-12
Palmer SC, Mavridis D, Nicolucci A, Johnson DW, Tonelli M, Craig JC, et al. (2016) Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: a meta-analysis. JAMA 316(3):313–324
Melander A, Folino-Gallo P, Walley T, Schwabe U, Groop PH, Klaukka T, et al. (2006) Utilisation of antihyperglycaemic drugs in ten European countries: different developments and different levels. Diabetologia 49(9):2024–2029
Hampp C, Borders-Hemphill V, Moeny DG, Wysowski DK (2014) Use of antidiabetic drugs in the U.S., 2003-2012. Diabetes Care 37(5):1367–1374
Torre C, Guerreiro J, de Oliveira MS, Raposo JF, Martins AP, Leufkens H (2015) Patterns of glucose lowering drugs utilisation in Portugal and in the Netherlands. Trends over time. Prim Care Diabetes 9(6):482–489
Zaharan NL, Williams D, Bennett K (2014) Prescribing of antidiabetic therapies in Ireland: 10-year trends 2003-2012. Ir J Med Sci 183(2):311–318
Clemens KK, Shariff S, Liu K, Hramiak I, Mahon JL, McArthur E, et al. (2015) Trends in antihyperglycemic medication prescriptions and hypoglycemia in older adults: 2002-2013. PLoS One 10(9):e0137596
Ou HT, Chang KC, Liu YM, Wu JS (2016) Recent trends in utilisation of antidiabetic medications from 2008 to 2013: a nation-wide population-based study from Taiwan. J Diabetes
Ekström N, Schiöler L, Svensson A-M, Eeg-Olofsson K, Jonasson JM, Zethelius B, et al. (2012) Effectiveness and safety of metformin in 51 675 patients with type 2 diabetes and different levels of renal function: a cohort study from the Swedish National Diabetes Register. BMJ open 2(4):e001076
Herrington W, Nye H, Aung T (2013) Metformin use in chronic kidney disease: new evidence to guide dosing. QJM 106(11):1059–1061
Vasisht K, Chen SC, Peng Y, Bakris G (2010) Limitations of metformin use in patients with kidney disease: are they warranted? Diabetes. Obes Metab 12(12):1079–1083
Duong JK, Furlong TJ, Roberts DM, Graham GG, Greenfield JR, Williams KM, et al. (2013) The role of metformin in metformin-associated lactic acidosis (MALA): case series and formulation of a model of pathogenesis. Drug Saf 36:733–746
Acknowledgments
The authors would like to thank Ms. Agata Szylczak, Medical Records SVH, and Ms. Maxine Robinson, Secretary, Drug Utilisation Sub Committee of Pharmaceutical Benefits Advisory Committee, Pharmaceutical Benefits Scheme. The study was supported by the National Health and Medical Research Council Program under grants APP 568612 and APP 1054146 and Australian Research Council Linkage under grant LP0990670.
Author’s contributions
J Moon was responsible for data collection, data entry, data analysis and preparation of manuscript; SS Kumar for data entry, data analysis and preparation of manuscript; GG Graham for data analysis and preparation of manuscript; MT Baysari for data analysis and preparation of manuscript; KM Williams for data analysis and preparation of manuscript; W Chen for data collection and data analysis; A Viardot and JR Greenfield for clinical guidance and preparation of manuscript; and RO Day for clinical guidance, data analysis and preparation of manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Electronic supplementary material
Supplementary Table 1
(DOCX 27 kb)
Supplementary Table 2
(DOCX 50 kb)
Supplementary Table 3
(DOCX 24 kb)
Supplementary Table 4
(DOCX 20 kb)
Supplementary 5
(DOCX 30 kb)
Rights and permissions
About this article
Cite this article
Moon, J., Kumar, S.S., Graham, G.G. et al. Trends in metformin utilisation and dose appropriateness in Australia. Eur J Clin Pharmacol 72, 1489–1496 (2016). https://doi.org/10.1007/s00228-016-2117-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2117-y