Abstract
Rationale
The optimal dose for achieving the maximum antidepressive effect of selective serotonin reuptake inhibitors (SSRIs) or serotonin-noradrenalin reuptake inhibitors (SNRIs) remains a controversial issue. The varying sensitivity of scales that measure the severity of depression is one of the many factors affecting the evaluation of the dose–response relationship with antidepressants.
Objectives
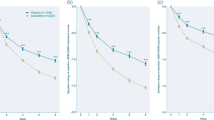
To determine if the 6-item Hamilton rating scale for depression (HAM-D6) demonstrates a clearer association between dose and antidepressive effect compared with the 17-item Hamilton rating scale for depression (HAM-D17) for fixed doses of duloxetine hydrochloride (40, 60, 80, and 120 mg daily) from six double-blind, randomized, placebo-controlled clinical trials assessing safety and efficacy in the acute treatment of patients with DSM-IV-defined major depressive disorder (MDD).
Methods
Mantel–Haenszel adjusted effect sizes were determined by dose for change from baseline to endpoint in HAM-D6 and HAM-D17 scores from the six studies. To confirm, assessments were repeated on the subset of the population corresponding to the 70% of patients with the longest duration of treatment regardless of study, treatment, dose, geography, or completion status.
Results
For the majority of assessments, HAM-D6 effect sizes were numerically larger than those estimated from the HAM-D17. Findings support that duloxetine 60 mg daily is the best effective dose.
Conclusions
In this assessment of patients with MDD, the HAM-D6 was shown to be more sensitive compared with the HAM-D17 at detecting treatment effects. These findings are consistent with published results of other effective antidepressants.
Similar content being viewed by others
References
Angst J et al (1989) Consensus conference on the methodology of clinical trials of antidepressants. Pharmacopsychiatry 22:3–7
Bagby RM et al (2004) The Hamilton Depression Rating Scale: has the gold standard become a lead weight? Am J Psychiatry 161:2163–2177
Bech P (2001) Meta-analysis of placebo-controlled trials with mirtazapine using the core items of the Hamilton Depression Scale as evidence of a pure antidepressive effect in the short-term treatment of major depression. Int J Neuropsychopharmacol 4:337–345
Bech P (2002) The Bech-Rafaelsen Melancholia Scale (MES) in clinical trials of therapies in depressive disorders: a 20-year review of its use as outcome measure. Acta Psychiatr Scand 106:252–264
Bech P et al (1975) Quantitative rating of depressive states. Acta Psychiatr Scand 51:161–170
Bech P et al (1981) The Hamilton Depression Scale. Evaluation of objectivity using logistic models. Acta Psychiatr Scand 63:290–299
Bech P et al (1984) Assessment of symptom change from improvement curves on the Hamilton Depression Scale in trials with antidepressants. Psychopharmacology (Berl) 84:276–281
Bech P et al (2000) Meta-analysis of randomized controlled trials of fluoxetine v. placebo and tricyclic antidepressants in the short-term treatment of major depression. Br J Psychiatry 176:421–428
Bech P et al (2002) Citalopram dose–response revisited using an alternative psychometric approach to evaluate clinical effects of four fixed citalopram doses compared to placebo in patients with major depression. Psychopharmacology (Berl) 163:20–25
Bech P et al (2004) Escitalopram dose-response revisited: an alternative psychometric approach to evaluate clinical effects of escitalopram compared to citalopram and placebo in patients with major depression. Int J Neuropsychopharmacol 7:283–290
Bobes J et al (2003) A comparative psychometric study of the Spanish versions with 6, 17, and 21 items of the Hamilton Depression Rating Scale. Med Clin (Barc) 120:693–700 (Article in Spanish)
Borsboom D (2005) Measuring the mind. Conceptual issues in contemporary psychometrics. Cambridge University Press, Cambridge
Bulpitt CJ (1988) Medical statistics: meta-analysis. Lancet 2:93–94
Burroughs VJ et al (2002a) Cultural and genetic diversity and America: the need for individualized pharmaceutical treatment. National Pharmaceutical Council and National Medical Association. Last accessed on 12/06/2005 available from: http://www.npcnow.org/resources/PDFs/CulturalFINAL.pdf
Burroughs VJ et al (2002b) Racial and ethnic differences in response to medicines: towards individualized pharmaceutical treatment. J Natl Med Assoc 94:1–26
Bymaster FP et al (2001) Comparative affinity of duloxetine and venlafaxine for serotonin and norepinephrine transporters in vitro and in vivo, human serotonin receptor subtypes, and other neuronal receptors. Neuropsychopharmacology 25:871–880
Detke MJ et al (2002a) Duloxetine 60 mg once daily dosing versus placebo in the acute treatment of major depression. J Psychiatr Res 36:383–390
Detke MJ et al (2002b) Duloxetine, 60 mg once daily, for major depressive disorder: a randomized double-blind placebo-controlled trial. J Clin Psychiatry 63:308–315
Detke MJ et al (2004) Duloxetine in the acute and long-term treatment of major depressive disorder: a placebo- and paroxetine-controlled trial. Eur Neuropsychopharmacol 14:457–470
DUAG (Danish University Antidepressant Group) (1999) Clomipramine dose–effect study in patients with depression: clinical endpoints and pharmacokinetics. Clin Pharmacol Ther 66:152–165
Dunlop SR et al (1990) Pattern analysis shows beneficial effect of fluoxetine treatment in mild depression. Psychopharmacol Bull 26:173–180
Engels EA et al (2000) Heterogeneity and statistical significance in meta-analysis: an empirical study of 125 meta-analyses. Stat Med 19:1707–1728
Entsuah R et al (2002) A critical examination of the sensitivity of unidimensional subscales derived from the Hamilton Depression Rating Scale to antidepressant drug effects. J Psychiatr Res 36:437–448
Fabre LF et al (1995) Sertraline safety and efficacy in major depression: a double-blind fixed-dose comparison with placebo. Biol Psychiatry 38:592–602
Faries D et al (2000) The responsiveness of the Hamilton Depression Rating Scale. J Psychiatr Res 34:3–10
Gex-Fabry M et al (2004) Time course of clinical response to venlafaxine: relevance of plasma level and chirality. Eur J Clin Pharmacol 59:883–891
Gibbons RD et al (1993) Exactly what does the Hamilton Depression Rating Scale measure? J Psychiatr Res 27:259–273
Goldstein et al (2004) Duloxetine in the treatment of depression: a double-blind placebo-controlled comparison with paroxetine. J Clin Psychopharmacol 24(4):389–399
Hamilton M (1967) Development of a rating sale for primary depressive illness. Br J Soc Clin Psychol 6:278–296
Hedges LV, Olkin I (1985) Statistical methods for meta-analysis. Academic, New York, NY
Lecrubier Y et al (1996) Clinical efficacy of milnacipran: placebo-controlled trials. Int Clin Psychopharmacol 11(Suppl 4):29–33
Licht RW et al (2005) Validation of the Bech–Rafaelsen Melancholia Scale and the Hamilton Depression Scale in patients with major depression: is the total score a valid measure of illness severity? Acta Psychiatr Scand 111:144–199
Maier W, Philipp M (1985) Improving the assessment of severity of depressive states: a reduction of the Hamilton Depression Scale. Pharmacopsychiatry 18:114–115
Mendels J et al (1993) Efficacy and safety of b.i.d. doses of venlafaxine in a dose-response study. Psychopharmacol Bull 29:169–174
Moncrieff J, Kirsch I (2005) Efficacy of antidepressants in adults. BMJ 331:155–157
Nemeroff et al (2002) Duloxetine for the treatment of major depressive disorder. Psychopharmacol Bull 36(4):106–132
Niklson IA, Reimitz PE (2001) Baseline characteristics of major depressive disorder patients in clinical trials in Europe and United States: is there a transatlantic difference? J Psychiatr Res 35:71–81
O’Sullivan RL et al (1997) Sensitivity of the six-item Hamilton Depression Rating Scale. Acta Psychiatr Scand 95:379–384
Paykel ES (1990) The use of the Hamilton Depression Scale in general practice. Psychopharmacol Ser 9:40–47
Peto R (1987) Why do we need systematic overviews of randomized trials? Stat Med 6:233–244
Pogue J, Yusuf S (1998) Overcoming the limitations of current meta-analysis of randomized controlled trials. Lancet 351:47–52
Preskorn SH (1998) Recent dose-effect studies regarding antidepressants. In: Balant LP, Benitez J, Dahl SG, Gram LF, Pinder RM, Potter WZ (eds) European cooperation in the field of scientific and technical research. European Commission, Brussels, Belgium, pp 45–61
Reisby N et al (1979) Clomipramine: plasma levels and clinical effects. Commun Psychopharmacol 3:341–351
Rifkin A (1997) SSRI optimal dose remains at issue. J Clin Psychiatry 58:87–88
Rudolph RL et al (1998) A randomized, placebo-controlled, dose–response trial of venlafaxine hydrochloride in the treatment of major depression. J Clin Psychiatry 59:116–122
Ruhe H et al (2005) Clinical use of the Hamilton Depression Scale: is increased efficiency possible? A post hoc comparison of the Hamilton Depression Rating Scale, Maier and Bech subscales, Clinical Global Impression and Symptom Checklist-90 scores. Compr Psychiatry 46:417–427
Schmid JE et al (1991) An overview of statistical issues and methods of meta-analysis. J Biopharm Stat 1:103–120
Wernicke JF et al (1988) Low-dose fluoxetine therapy for depression. Psychopharmacol Bull 24:183–188
Wernicke JF et al (1987) Fixed-dose fluoxetine therapy for depression. Psychopharmacol Bull 23:164–168
Acknowledgements
The authors wish to thank Ling Ling Xie, MS; Barry M. Brolley, MS; Quan Zhao, MS; and Ying Yuan Chen, MS, for their assistance with statistical analyses and reporting. The clinical studies referred to in this work were conducted under the Declaration of Helsinki and confirmed to all applicable local and region regulations. All protocols and informed consent documents were approved by local or regional review boards before study initiation, and all patients were required to sign an informed consent before participation in any study-related activities.
Author information
Authors and Affiliations
Corresponding author
Additional information
Drs. Porsdal and Kajdasz are employees of Eli Lilly & Company.
Rights and permissions
About this article
Cite this article
Bech, P., Kajdasz, D.K. & Porsdal, V. Dose–response relationship of duloxetine in placebo-controlled clinical trials in patients with major depressive disorder. Psychopharmacology 188, 273–280 (2006). https://doi.org/10.1007/s00213-006-0505-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-006-0505-1