Abstract
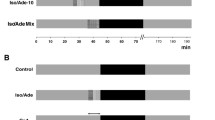
Evidence as to how ACE inhibitors attenuate ischemia-reperfusion injury (IR) after cardioplegic arrest remains scarce. Twenty-four rabbit hearts were perfused on a Langendorff apparatus. Control hearts (n = 6) were arrested with pure histidine-tryptophan-ketoglutarate (HTK)-Bretschneider. Treatment groups received added to the cardioplegic solution (n = 6) captopril (100 μmol/l) and losartan (100 μmol/l) for selective AT1-receptor antagonism or BQ123 (100 nmol/l) for selective ETA-receptor antagonism. Pre-ischemic equilibration of 45 min was followed by 90 min of cardioplegic arrest and 30 min of reperfusion. Indices of myocardial contractility (LVP, dp/dt max, dp/dt min), coronary flow, heart rate, and O2 consumption were recorded before and after ischemic arrest. Tissue adenosine triphosphate (ATP) and malondialdehyde (MDA) contents were measured to evaluate energy content and oxidative stress, respectively. After selective cardiac arrest with Bretschneider, captopril-treated hearts showed improved hemodynamics compared to control and the other treatment groups. Oxygen consumption was significantly decreased during early reperfusion in captopril-treated hearts (34 ± 3 μmol/min/g/mmHg) compared to controls and losartan- and BQ123-treated hearts (controls: 77 ± 9 μmol/min/g/mmHg, p = 0.003; losartan: 54 ± 9 μmol/min/g/mmHg, p = 0.015; BQ123: 64 ± 13 μmol/min/g/mmHg, p = 0.046). The ATP content of the reperfused tissue was significantly elevated after captopril treatment compared to control group (24 ± 2 vs. 16 ± 2 μmol/g, p = 0.033), whereas the level of MDA was substantially decreased (0.58 ± 0.163 vs. 1.5 ± 0.28 μmol/g, p = 0.009). ACE inhibition leads to a significantly greater and faster recovery of myocardial contractility after prolonged cardiac arrest with Bretschneider solution. Due to decreased oxygen consumption, myocardial protection is enhanced. The association between ACE and ischemia cannot be clarified by selective blockade of angiotensin-II receptor type 1 (AT1-R) or ETa receptor (ETa-R).




Similar content being viewed by others
References
Allen IS, Cohen NM, Dhallan RS, Gaa ST, Lederer WJ, Rogers TB (1988) Angiotensin II increases spontaneous contractile frequency and stimulates calcium current in cultured neonatal rat heart myocytes: insights into the underlying biochemical mechanisms. Circ Res 62(3):524–534
Anselmi A, Abbate A, Girola F, Nasso G, Biondi-Zoccai GG, Possati G, Gaudino M (2004) Myocardial ischemia, stunning, inflammation, and apoptosis during cardiac surgery: a review of evidence. Eur J Cardiothorac Surg 25(3):304–311
Bolli R, Becker L, Gross G, Mentzer R, Balshaw D, Lathrop DA (2004) Myocardial protection at a crossroads: the need for translation into clinical therapy. Circ Res 95(2):125–134
Braathen B, Jeppsson A, Scherstén H, Hagen OM, Vengen Ø, Rexius H, Tønnessen T (2011) One single dose of histidine–tryptophan–ketoglutarate solution gives equally good myocardial protection in elective mitral valve surgery as repetitive cold blood cardioplegia: a prospective randomized study. J Thorac Cardiovasc Surg 141(4):995–1001
Bretschneider HJ (1980) Myocardial protection. Thorac Cardiovasc Surg 28(5):295–302
Bretschneider HJ, Hübner G, Knoll D, Lohr B, Nordbeck H, Spieckermann PG (1974) Myocardial resistance and tolerance to ischemia: physiological and biochemical basis. J Cardiovasc Surg (Torino) 16(3):241–260
Dhein S, Mueller A, Gerwin R, Klaus W (1993) Comparative study on the proarrhythmic effects of some antiarrhythmic agents. Circulation 87:617–630
Endoh M (1993) Pharmacological characteristics of the positive inotropic effect of angiotensin II in the rabbit ventricular myocardium. Br J Pharmacol 108(4):999–1005
Endoh M, Fujita S, Yang HT, Talukder MA, Maruya J, Norota I (1998) Endothelin: receptor subtypes, signal transduction, regulation of ca < sup > 2 + </sup > transients and contractility in rabbit ventricular myocardium. Life Sci 62(17):1485–1489
Fan Y, Zhang AM, Xiao YB, Weng YG, Hetzer R (2010) Warm versus cold cardioplegia for heart surgery: a meta-analysis. Eur J Cardiothorac Surg 37(4):912–919
Fischer UM, Klass O, Stock U, Easo J, Geissler HJ, Fischer JH, Mehlhorn U (2003) Cardioplegic arrest induces apoptosis signal-pathway in myocardial endothelial cells and cardiac myocytes. Eur J Cardiothorac Surg 23(6):984–990
Garbade J, Davierwala P, Seeburger J, Pfannmueller B, Misfeld M, Borger MA, Mohr FW (2013) Myocardial protection during minimally invasive mitral valve surgery: strategies and cardioplegic solutions. Ann cardiothorac Surg 2(6):803
Gurevitch MD, Pevni MD, Frolkis MD, Matsa MD, Paz MD, Mohr MD, Yakirevich MD (1997) Captopril in cardioplegia and reperfusion: protective effects on the ischemic heart. Ann Thorac Surg 63(3):627–633
Heyndrickx GR (2006) Early reperfusion phenomena. Semin Cardiothorac Vasc Anesth 10(3):236–241
Hirsch AT, Talsness C, Schunkert H, Paul M, Dzau VJ (1991) Tissue-specific activation of cardiac angiotensin converting enzyme in experimental heart failure. Circ Res 69(2):475–482
Jacob S, Kallikourdis A, Sellke F, Dunning J (2008) Is blood cardioplegia superior to crystalloid cardioplegia? Interact Cardiovasc Thorac Surg 7(3):491–498
Jalowy A, Schulz R, Dörge H, Behrends M, Heusch G (1998) Infarct size reduction by AT1-receptor blockade through a signal cascade of AT2-receptor activation, bradykinin and prostaglandins in pigs. J Am Coll Cardiol 32(6):1787–1796
Katz AM (1977) Physiology of the heart. Raven Press Books, Ltd., New York
Kitakaze M, Minamino T, Node K, Komamura K, Shinozaki Y, Mori H, Kamada T (1995) Beneficial effects of inhibition of angiotensin-converting enzyme on ischemic myocardium during coronary hypoperfusion in dogs. Circulation 92(4):950–961
Korn P, Kröner A, Schirnhofer J, Hallström S, Bernecker O, Mallinger R, Podesser BK (2002) Quinaprilat during cardioplegic arrest in the rabbit to prevent ischemia-reperfusion injury. J Thorac Cardiovasc Surg 124(2):352–360
Louch WE, Ferrier GR, Howlett SE (2005) Attentuation of cardiac stunning by losartan in a cellular model of ischemia and reperfusion is accompanied by increased sarcoplasmic reticulum Ca2+ stores and prevention of cytosolic Ca2+ elevation. J Pharmacol Exp Ther 312(1):238–247
Mehlhorn U, Krahwinkel A, Geissler HJ, LaRosee K, Fischer UM, Klass O, Bloch W (2003) Nitrotyrosine and 8-isoprostane formation indicate free radical-mediated injury in hearts of patients subjected to cardioplegia. J Thorac Cardiovasc Surg 125(1):178–183
Menasché P, Grousset C, Peynet J, Mouas C, Bloch G, Piwnica A (1992) Pretreatment with captopril improves myocardial recovery after cardioplegic arrest. J Cardiovasc Pharmacol 19(3):402–407
Murphy E, Steenbergen C (2008) Mechanisms underlying acute protection from cardiac ischemia-reperfusion injury. Physiol Rev 88(2):581–609
Neely JR, Liebermeister H, Morgan HE (1967) Effect of pressure development on membrane transport of glucose in isolated rat heart. Am J Physiol 212(4):815–822
Ozdemir R, Parlakpinar H, Polat A, Colak C, Ermis N, Acet A (2006) Selective endothelin a (ETa) receptor antagonist (BQ-123) reduces both myocardial infarct size and oxidant injury. Toxicology 219(1):142–149
Paz MD, Gurevitch MD, Frolkis MD, Matsa MD, Kramer MD, Locker MD, Keren MD (1998) Effects of an angiotensin II antagonist on ischemic and nonischemic isolated rat hearts. Ann Thorac Surg 65(2):474–479
Pfeffer MA (2000) Enhancing cardiac protection after myocardial infarction: rationale for newer clinical trials of angiotensin receptor blockers. Am Heart J 139(1):23–28
Pritzwald-Stegmann P, Hoyer A, Kempfert J, Dhein S, Mohr FW (2011) Cardioprotective effects of low-dose cyclosporin A added to histidine-tryptophan-ketoglutarate cardioplegia solution prior to total myocardial ischemia: an in vitro rabbit heart study. Pharmacology 88(3–4):167–173
Sadoshima J (2002) Novel AT1 receptor–independent functions of losartan. Circ Res 90(7):754–756
Scott-Burden T, Resink TJ, Hahn AW, Vanhoutte PM (1991) Induction of endothelin secretion by angiotensin II: effects on growth and synthetic activity of vascular smooth muscle cells. J Cardiovasc Pharmacol 17:S96–100
Sharpe N, Smith H, Murphy J, Greaves S, Hart H, Gamble G (1991) Early prevention of left ventricular dysfunction after myocardial infarction with angiotensin-converting-enzyme inhibition. The Lancet 337(8746):872–876
Steenbergen C, Murphy E, Watts JA, London RE (1990) Correlation between cytosolic free calcium, contracture, ATP, and irreversible ischemic injury in perfused rat heart. Circ Res 66(1):135–146
Sternbergh WC, Brunsting LA, Abd-Elfattah AS, Wechsler AS (1989) Basal metabolic energy requirements of polarized and depolarized arrest in rat heart. Am J Physiol 256(3 pt 2):H846–51
Takanashi M, Endoh M (1991) Characterization of positive inotropic effect of endothelin on mammalian ventricular myocardium. Am J Physiol 261(3 Pt 2):H611–9
Trescher K, Bauer M, Dietl W, Hallström S, Wick N, Wolfsberger M, Ullrich R, Jürgens G, Wollner E, Podesser BK (2009) Improved myocardial protection in the failing heart by selective endothelin-A receptor blockade. J Thorac Cardiovasc Surg 137(4):1005–1011
Werrmann JG, Cohen SM (1996) Use of losartan to examine the role of the cardiac renin-angiotensin system in myocardial dysfunction during ischemia and reperfusion. J Cardiovasc Pharmacol 27(2):177–182
Woo YJ, Grand TJ, Zentko S, Cohen JE, Hsu V, Atluri P, Berry MF, Taylor MD, Moise MA, Fisher O, Kolakowski S (2005) Creatine phosphate administration preserves myocardial function in a model of off-pump coronary revascularization. J Cardiovasc Surg 46:297–303
Yang HT, Sakurai K, Sugawara H, Watanabe T, Norota I, Endoh M (1999) Role of Na+/Ca2+ exchange in endothelin‐1‐induced increases in Ca2+ transient and contractility in rabbit ventricular myocytes: pharmacological analysis with KB‐R7943. Br J Pharmacol 126(8):1785–1795
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoyer, A., Kempfert, J., Pritzwald-Stegmann, P. et al. Acute hemodynamic effects of angiotensin- converting enzyme inhibition after prolonged cardiac arrest with Bretschneider’s solution. Naunyn-Schmiedeberg's Arch Pharmacol 387, 1221–1229 (2014). https://doi.org/10.1007/s00210-014-1052-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-014-1052-7