Abstract
Summary
We estimated primary non-adherence to oral bisphosphonate medication and examined the factors associated with primary non-adherence. Nearly 30 % of women did not pick up their new bisphosphonate within 60 days. Identifying barriers and developing interventions that address patients’ needs and concerns at the time a new medication is prescribed are warranted.
Introduction
To estimate primary non-adherence to oral bisphosphonate medications using electronic medical record data in a large, integrated healthcare delivery system and to describe patient and prescribing provider factors associated with primary non-adherence.
Methods
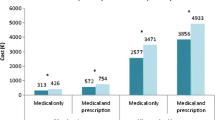
Women aged 55 years and older enrolled in Kaiser Permanente Southern California (KPSC) with a new prescription for oral bisphosphonates between December 1, 2009 and March 31, 2011 were identified. Primary non-adherence was defined as failure to pick up the new prescription within 60 days of the order date. Multivariable logistic regression models were used to investigate patient factors (demographics, healthcare utilization, and health conditions) and prescribing provider characteristics (demographics, years in practice, and specialty) associated with primary non-adherence.
Results
We identified 8,454 eligible women with a new bisphosphonate order. Among these women, 2,497 (29.5 %) did not pick up their bisphosphonate prescription within 60 days of the order date. In multivariable analyses, older age and emergency department utilization were associated with increased odds of primary non-adherence while prescription medication use and hospitalizations were associated with lower odds of primary non-adherence. Prescribing providers practicing 10 or more years had lower odds of primary non-adherent patients compared with providers practicing less than 10 years. Internal medicine and rheumatology providers had lower odds of primary non-adherent patients than primary care providers.
Conclusion
This study found that nearly one in three women failed to pick up their new bisphosphonate prescription within 60 days. Identifying barriers and developing interventions aimed at reducing the number of primary non-adherent patients to bisphosphonate prescriptions are warranted.


Similar content being viewed by others
References
Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM (1993) Primary non-compliance with prescribed medication in primary care. Bmj 307:846–848
Gadkari AS, McHorney CA (2010) Medication nonfulfillment rates and reasons: narrative systematic review. Curr Med Res Opin 26:683–705. doi:10.1185/03007990903550586
Waalen J, Bruning AL, Peters MJ, Blau EM (2009) A telephone-based intervention for increasing the use of osteoporosis medication: a randomized controlled trial. Am J Manag Care 15:e60–70
Cook PF, Emiliozzi S, McCabe MM (2007) Telephone counseling to improve osteoporosis treatment adherence: an effectiveness study in community practice settings. Am J Med Qual 22:445–456. doi:10.1177/1062860607307990
Greenwald B, Bardwell A, Malinak J, Rude R, Silverman SL, White-Greenwald M (2002) New bone density report format influences patient compliance in filling prescriptions for osteoporosis. Clin J Wom Health 2:13–18
Karter AJ, Parker MM, Moffet HH, Ahmed AT, Schmittdiel JA, Selby JV (2009) New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res 44:1640–1661. doi:10.1111/j.1475-6773.2009.00989.x
Koebnick C, Langer-Gould AM, Gould MK, Chao CR, Iyer RL, Smith N, Chen W, Jacobsen SJ (2012) Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. The Permanente Journal 16:37–41
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Hosmer DW, Lemeshow S (1989) Applied logistic regression. John Wiley & Sons, New York
Shin J, McCombs JS, Sanchez RJ, Udall M, Deminski MC, Cheetham TC (2012) Primary nonadherence to medications in an integrated healthcare setting. Am J Manag Care 18:426–434
Fischer MA, Choudhry NK, Brill G, Avorn J, Schneeweiss S, Hutchins D, Liberman JN, Brennan TA, Shrank WH (2011) Trouble getting started: predictors of primary medication nonadherence. Am J Med 124(1081):1089–1022. doi:10.1016/j.amjmed.2011.05.028
Raebel MA, Ellis JL, Carroll NM, Bayliss EA, McGinnis B, Schroeder EB, Shetterly S, Xu S, Steiner JF (2012) Characteristics of patients with primary non-adherence to medications for hypertension, diabetes, and lipid disorders. J Gen Intern Med 27:57–64. doi:10.1007/s11606-011-1829-z
Shah ND, Dunlay SM, Ting HH, Montori VM, Thomas RJ, Wagie AE, Roger VL (2009) Long-term medication adherence after myocardial infarction: experience of a community. Am J Med 122(961):967–913. doi:10.1016/j.amjmed.2008.12.021
Shah NR, Hirsch AG, Zacker C, Taylor S, Wood GC, Stewart WF (2009) Factors associated with first-fill adherence rates for diabetic medications: a cohort study. J Gen Intern Med 24:233–237. doi:10.1007/s11606-008-0870-z
Liberman JN, Hutchins DS, Popiel RG, Patel MH, Jan SA, Berger JE (2010) Determinants of primary nonadherence in asthama-controller and dyslipidemia pharmacotherapy. Am J Pharm Benefits 2:111–118
Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X (2008) Interventions for enhancing medication adherence. Cochrane database of systematic reviews CD000011. doi:10.1002/14651858.CD000011.pub3
Derose SF, Green K, Marrett E, Cheetham TC, Chiu VY, Harrison TN, Reynolds K, Vansomphone SS, Scott RD (2012) Automated outreach to increase primary adherence to cholesterol-lowering medications. Arch Intern Med Published online: doi:10.1001/2013.jamainternmed.717
Gerend MA, Erchull MJ, Aiken LS, Maner JK (2006) Reasons and risk: factors underlying women's perceptions of susceptibility to osteoporosis. Maturitas 55:227–237. doi:10.1016/j.maturitas.2006.03.003
Hsieh C, Novielli KD, Diamond JJ, Cheruva D (2001) Health beliefs and attitudes toward the prevention of osteoporosis in older women. Menopause 8:372–376
McHorney CA, Spain CV (2011) Frequency of and reasons for medication non-fulfillment and non-persistence among American adults with chronic disease in 2008. Health Expect 14:307–320. doi:10.1111/j.1369-7625.2010.00619.x
Reginster JY, Rabenda V (2006) Patient preference in the management of postmenopausal osteoporosis with bisphosphonates. Clin Interv Aging 1:415–423
Scoville EA, de Leon P, Lovaton P, Shah ND, Pencille LJ, Montori VM (2011) Why do women reject bisphosphonates for osteoporosis? A videographic study. PLoS One 6:e18468. doi:10.1371/journal.pone.0018468
Yood RA, Mazor KM, Andrade SE, Emani S, Chan W, Kahler KH (2008) Patient decision to initiate therapy for osteoporosis: the influence of knowledge and beliefs. J Gen Intern Med 23:1815–1821. doi:10.1007/s11606-008-0772-0
Danese MD, Badamgarav E, Bauer DC (2009) Effect of adherence on lifetime fractures in osteoporotic women treated with daily and weekly bisphosphonates. J Bone Miner Res 24:1819–1826. doi:10.1359/jbmr.090506
Acknowledgements
This study was funded by a contractual agreement between Kaiser Permanente Southern California and Amgen Inc., Thousand Oaks, CA.
Conflicts of interest
Dr. O’Malley is an employee of Amgen Inc. and owns stock in Amgen Inc. Drs. Muntner, Gold, Silverman, and Morisky have served as advisors for Amgen Inc. Drs. Muntner, Gold and Silverman have served as consultants for Amgen Inc. Drs. Reynolds and Muntner received research support from Amgen Inc. Dr. Silverman has served as an advisor for Lilly, Novartis and Pfizer/Wyeth. Dr. Silverman has served as a consultant for Genentech, Lilly, Novartis and Pfizer/Wyeth. Dr. Silverman has received research support from Lilly and Pfizer/Wyeth. This study was funded by a contractual agreement between Kaiser Permanente Southern California and Amgen Inc., Thousand Oaks, CA.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Rights and permissions
About this article
Cite this article
Reynolds, K., Muntner, P., Cheetham, T.C. et al. Primary non-adherence to bisphosphonates in an integrated healthcare setting. Osteoporos Int 24, 2509–2517 (2013). https://doi.org/10.1007/s00198-013-2326-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2326-5