Abstract
Summary
Denosumab is an injectable drug that reduces the risk of fractures. The objective was to estimate the cost-effectiveness of denosumab in a Swedish setting, also accounting for poor adherence to treatment. Denosumab is cost-effective, particularly for patients at high risk of fracture and low adherence to oral treatments.
Introduction
Denosumab is a novel biologic agent developed for the treatment of osteoporosis and osteoporotic fractures that has been shown to reduce the risk of fractures in a phase III trial. The objective of this study was to estimate the cost-effectiveness of denosumab from a societal perspective compared with generic alendronate, branded risedronate, strontium ranelate, and no treatment in a Swedish setting.
Methods
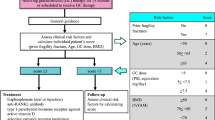
A Markov cohort model was used to estimate the cost-effectiveness of denosumab given for up to 5 years to a typical Swedish patient population (women aged 71 years, T-score ≤ −2.5 SD and a prevalence of morphometric vertebral fractures of 34%). The model included treatment persistence and residual effect after discontinuation assumed to be equal to the time on treatment. Persistence with the comparator treatments and with denosumab was derived from prescription data and a persistence study, respectively.
Results
The base-case incremental cost-effectiveness ratios were estimated at €27,000, €12,000, €5,000, and €14,000, for denosumab compared with generic alendronate, risedronate, strontium ranelate, and no treatment, respectively. Sub-optimal persistence had the greatest impact in the comparison with generic alendronate, where the difference in drug cost was large.
Conclusion
Improving persistence with osteoporosis treatment impacts positively on cost-effectiveness with a larger number of fractures avoided in the population targeted for treatment. Denosumab is a cost-effective alternative to oral osteoporosis treatments, particularly for patients at high risk of fracture and low expected adherence to oral treatments.





Similar content being viewed by others
References
Kanis JA, Johnell O (2005) Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int 16:229–238
Delmas PD (2002) Treatment of postmenopausal osteoporosis. Lancet 359:2018–2026
Murthy RK, Morrow PK, Theriault RL (2009) Bone biology and the role of the RANK ligand pathway. Oncology (Williston Park) 23:9–15
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, Silverman S (2006) Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc 81:1013–1022
Papaioannou A, Ioannidis G, Adachi JD, Sebaldt RJ, Ferko N, Puglia M, Brown J, Tenenhouse A, Olszynski WP, Boulos P, Hanley DA, Josse R, Murray TM, Petrie A, Goldsmith CH (2003) Adherence to bisphosphonates and hormone replacement therapy in a tertiary care setting of patients in the CANDOO database. Osteoporos Int 14:808–813
Strom O, Borgstrom F, Kanis JA, Jonsson B (2009) Incorporating adherence into health economic modelling of osteoporosis. Osteoporos Int 20:23–34
Strom O, Borgstrom F, Sen SS, Boonen S, Haentjens P, Johnell O, Kanis JA (2007) Cost-effectiveness of alendronate in the treatment of postmenopausal women in 9 European countries–an economic evaluation based on the fracture intervention trial. Osteoporos Int 18:1047–1061
Borgstrom F, Jonsson B, Strom O, Kanis JA (2006) An economic evaluation of strontium ranelate in the treatment of osteoporosis in a Swedish setting: based on the results of the SOTI and TROPOS trials. Osteoporos Int 17:1781–1793
Kanis JA, Adams J, Borgstrom F, Cooper C, Jonsson B, Preedy D, Selby P, Compston J (2008) The cost-effectiveness of alendronate in the management of osteoporosis. Bone 42:4–15
Landfeldt E, Borgström F, Robbins S, Ström O (2009) A retrospective cohort study of medication adherence to treatment of osteoporosis in a Swedish population. Oral presentation, ISPOR, Paris
Kanis J (2008) Assessment of osteoporosis at the primary health-care level. Technical Report, p61, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, UK
Medical products agency (2007) Behandling av osteoporos. www.mpa.se
Felsenberg D, Silman A, Lunt M, Ambrecht G, Ismail A (2002) Incidence of vertebral fracture in Europe: results from the European prospective osteoporosis study (EPOS). J Bone Miner Res 17:716–724
Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O (2003) Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int 14:61–68
NICE (2008) Systematic reviews of clinical effectiveness prepared for the guideline Osteoporosis: “Assessment of fracture risk and the prevention of osteoporotic fractures in individuals at high risk”. (http://wwwniceorguk/guidance/indexjsp?action=byID&o=11621)
Jones ML, Wilkinson A (2006) Adverse effects and persistence with therapy in patients taking oral alendronate, etidronate or residronate: systematic reviews (NICE). The University of Sheffield, School of Health and Related Research (http://www.nice.org.uk/guidance/index.jsp?action=download&o=36718)
Stevenson M, Davis S (2006) DSU economic evaluation of pooled alendronate and risedronate compared with strontium ranelate, raloxifene, etidronate and teriparatide. National Institute of Clinical Exelence (NICE), http://www.nice.org.uk/page.aspx?o=370643. Accessed 13 May 2009
Reginster JY, Bruyere O, Sawicki A, Roces-Varela A, Fardellone P, Roberts A, Devogelaer JP (2009) Long-term treatment of postmenopausal osteoporosis with strontium ranelate: results at 8 years. Bone 45:1059–1064
Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ (2007) Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clin Proc 82:1493–1501
McClung M, Freemantle N, Kendler D, Lillestol M, Moffett A, Satram-Hoang S, Yang Y, Kaur P, Macarios D, Siddhanti S (2010) Open-label study to evaluate the adherence, preference, and satisfaction of denosumab and alendronate in postmenopausal women. S 386 Osteoporos Int 21:[Suppl1]S25-S388 1 C P899
Kanis JA, Borgstrom F, Johnell O, Oden A, Sykes D, Jonsson B (2005) Cost-effectiveness of raloxifene in the UK: an economic evaluation based on the MORE study. Osteoporos Int 16:15–25
Kanis JA, Johnell O, Oden A, Jonsson B, Dawson A, Dere W (2000) Risk of hip fracture derived from relative risks: an analysis applied to the population of Sweden. Osteoporos Int 11:120–127
De Laet CE, van Hout BA, Burger H, Hofman A, Pols HA (1997) Bone density and risk of hip fracture in men and women: cross sectional analysis. Br Med J 315:221–225
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O'Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Average Exchange Rates. http://www.riksbank.com Accessed 18 October 2009
Dental and Pharmaceutical Benefits Agency (2003) General guidelines for economic evaluations from the Pharmaceutical Benefits Board. www.tlv.se
Borgstrom F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, Abdon P, Ornstein E, Lunsjo K, Thorngren KG, Sernbo I, Rehnberg C, Jonsson B (2006) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 17:637–650
Ström O, Borgstrom F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, Abdon P, Ornstein E, Ceder L, Thorngren KG, Sernbo I, Jonsson B (2008) Long-term cost and effect on quality of life of osteoporosis-related fractures in Sweden. Acta Orthop 79:269–280
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–427
Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A, De Laet C, Jonsson B (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int 11:669–674
Jonsson B, Christiansen C, Johnell O, Hedbrandt J (1995) Cost-effectiveness of fracture prevention in established osteoporosis. Osteoporos Int 5:136–142
Ekman M (2002) Consumption and production by age in Sweden: Basic facts and health economic implications. http://www.tlv.se/Upload/Foretag/FOR-040506-tabell-lakemedel.pdf, Accessed 2009-12-11
Johanesson M, Jonsson B, Jonsson L, Kobelt G, Zethraeus N (2009) Why should economic evaluations of medical innovations have a societal perspective? Office of healt economics (OHE) No. 51 October
Burstrom K, Johannesson M, Diderichsen F (2001) Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 10:621–635
Dolan P (1997) Modeling valuations for EuroQol health states. Med Care 35:1095–1108
Statistics Sweden http://www.ssd.scb.se/databaser/makro/Produkt.asp?produktid=BE0101, Accessed 2010-03-16
The National Board of Health and Welfare. National Patient Register (NPC) and Cause of Death Register (CDR). http://www.sos.se/epc/epceng.htm
Ioannidis G, Papaioannou A, Hopman WM, Akhtar-Danesh N, Anastassiades T, Pickard L, Kennedy CC, Prior JC, Olszynski WP, Davison KS, Goltzman D, Thabane L, Gafni A, Papadimitropoulos EA, Brown JP, Josse RG, Hanley DA, Adachi JD (2009) Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. Cmaj 181:265–271
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15:38–42
Barrett JA, Baron JA, Beach ML (2003) Mortality and pulmonary embolism after fracture in the elderly. Osteoporos Int 14:889–894
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B (2004) Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int 15:108–112
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. Jama 301:513–521
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture. Bone 32:468–473
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, Vogt T, Wallace R, Yates AJ, LaCroix AZ (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. Jama 280:2077–2082
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, Adami S, Fogelman I, Diamond T, Eastell R, Meunier PJ, Reginster JY (2001) Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med 344:333–340
McCloskey EV, Johansson H, Oden A, Vasireddy S, Kayan K, Pande K, Jalava T, Kanis JA (2009) Ten-year fracture probability identifies women who will benefit from clodronate therapy–additional results from a double-blind, placebo-controlled randomised study. Osteoporos Int 20:811–817
Kanis JA, Johansson H, Oden A, McCloskey EV (2009) Bazedoxifene reduces vertebral and clinical fractures in postmenopausal women at high risk assessed with FRAX. Bone 44:1049–1054
Vägverket (1997) Vägverkets samhällsekonomiska kalkymodell. Ekonomisk teori och värderingar. In Authority VSR (ed). Stockholm
Tosteson AN, Burge RT, Marshall DA, Lindsay R (2008) Therapies for treatment of osteoporosis in US women: cost-effectiveness and budget impact considerations. Am J Manag Care 14:605–615
Tosteson AN, Do TP, Wade SW, Anthony MS, Downs RW (2010) Persistence and switching patterns among women with varied osteoporosis medication histories: 12-month results from POSSIBLE US. Osteoporos Int (E-pub ahead of print)
Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M (2007) Glucocorticoid-induced osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess 11:1–256
Stevenson M, Davies S (2006) DSU economic evaluation of pooled alendronate and risedronate compared with strontium ranelate, raloxifene, etidronate and teriparatide(http://guidance.nice.org.uk/page.aspx?o=370643)
Ström O, Landfeldt E, Robbins S, Borgström F (2010) Adherence to treatment of osteoporosis and fracture risk: The Swedish Adherence Register Analysis (SARA). Oral presentation/poster ECCEO/IOF, Florence
Huybrechts KF, Ishak KJ, Caro JJ (2006) Assessment of compliance with osteoporosis treatment and its consequences in a managed care population. Bone 38:922–928
McCloskey E, De Takats D, Orgee J, Aropinn S, Jalava T, Cliffe J, Reaney L, McGurk C, Charlesworth DJAK (2005) Characteristics associated with non-persistence during daily therapy. Experience from the placebo wing of a community based clinical trial. J Bone Miner Res 20(suppl 1):S282
Jonsson B, Kanis J, Dawson A, Oden A, Johnell O (1999) Effect and offset of effect of treatments for hip fracture on health outcomes. Osteoporos Int 10:193–199
Kanis JA, Jonsson B (2002) Economic evaluation of interventions for osteoporosis. Osteoporos Int 13:765–767
Kanis JA, Borgstrom F, Johnell O, Jonsson B (2004) Cost-effectiveness of risedronate for the treatment of osteoporosis and prevention of fractures in postmenopausal women. Osteoporos Int 15:862–871
WHO (1998) Guidelines for preclinical evaluation and clinical trials in osteoporosis. Geneve. http://whqlibdoc.who.int/publications/1998/9241545224_eng.pdf, Accessed
Prince R, Sipos A, Hossain A, Syversen U, Ish-Shalom S, Marcinowska E, Halse J, Lindsay R, Dalsky GP, Mitlak BH (2005) Sustained nonvertebral fragility fracture risk reduction after discontinuation of teriparatide treatment. J Bone Miner Res 20:1507–1513
Greendale GA, Espeland M, Slone S, Marcus R, Barrett-Connor E (2002) Bone mass response to discontinuation of long-term hormone replacement therapy: results from the Postmenopausal Estrogen/Progestin Interventions (PEPI) Safety Follow-up Study. Arch Intern Med 162:665–672
Bagger YZ, Tanko LB, Alexandersen P, Hansen HB, Mollgaard A, Ravn P, Qvist P, Kanis JA, Christiansen C (2004) Two to three years of hormone replacement treatment in healthy women have long-term preventive effects on bone mass and osteoporotic fractures: the PERF study. Bone 34:728–735
Christiansen C, Christensen MS, Transbol I (1981) Bone mass in postmenopausal women after withdrawal of oestrogen/gestagen replacement therapy. Lancet 1:459–461
Cauley JA, Seeley DG, Ensrud K, Ettinger B, Black D, Cummings SR (1995) Estrogen replacement therapy and fractures in older women. Study of Osteoporotic Fractures Research Group. Ann Intern Med 122:9–16
Banks E, Beral V, Reeves G, Balkwill A, Barnes I (2004) Fracture incidence in relation to the pattern of use of hormone therapy in postmenopausal women. Jama 291:2212–2220
Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, Satterfield S, Wallace RB, Bauer DC, Palermo L, Wehren LE, Lombardi A, Santora AC, Cummings SR (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. Jama 296:2927–2938
Gallagher AM, Rietbrock S, Olson M, van Staa TP (2008) Fracture outcomes related to persistence and compliance with oral bisphosphonates. J Bone Miner Res 23:1569–1575
Curtis JR, Westfall AO, Cheng H, Delzell E, Saag KG (2008) Risk of hip fracture after bisphosphonate discontinuation: implications for a drug holiday. Osteoporos Int 19:1613–1620
Lekander I, Borgstrom F, Strom O, Zethraeus N, Kanis JA (2008) Cost effectiveness of hormone therapy in women at high risks of fracture in Sweden, the US and the UK-Results based on the Women's Health Initiative randomised controlled trial. Bone 42:294–306
Zethraeus N, Borgstrom F, Jonsson B, Kanis J (2005) Reassessment of the cost-effectiveness of hormone replacement therapy in Sweden: results based on the Women's Health Initiative randomized controlled trial. Int J Technol Assess Health Care 21:433–441
NICE (2008) Osteoporosis—secondary prevention including strontium ranelate: Appraisal consultation document. www.nice.org.uk
Borgstrom F, Johnell O, Kanis JA, Oden A, Sykes D, Jonsson B (2004) Cost effectiveness of raloxifene in the treatment of osteoporosis in Sweden: an economic evaluation based on the MORE study. Pharmacoeconomics 22:1153–1165
Acknowledgments
The authors would like to acknowledge Amgen Inc. Thousand Oaks, CA, USA for funding model development and Steering Committee meetings. The authors are also grateful to Enkhe Badamgarav and David Macarios of Amgen Inc. and Deborah Marshall of the University of Calgary for their assistance in framing the research questions, aid in model development, and participation in the Steering Committee. The authors also sincerely appreciate the tremendous logistical and planning support provided by Dominika Dabrowski of i3 Innovus.
Conflicts of interest
Sponsored by Amgen.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jönsson, B., Ström, O., Eisman, J.A. et al. Cost-effectiveness of Denosumab for the treatment of postmenopausal osteoporosis. Osteoporos Int 22, 967–982 (2011). https://doi.org/10.1007/s00198-010-1424-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1424-x