Abstract
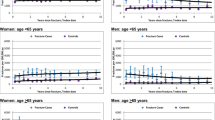
Introduction:Clinical fractures are associated with an increased relative risk of future fractures, but the absolute risk and timing of new clinical fractures immediately after a clinical fracture have not been reported extensively. The study objective was to determine the absolute risk of subsequent clinical fractures within 2 years after a clinical fracture. Methods:We analyzed clinical fracture data from a university hospital recruiting all fractures in the area between January 1999 and December 2001. Subjects were 2,419 male and female patients aged 50 years and older, with a total of 2,575 fractures. There were 139 patients with more than one simultaneous fracture. Mean age was 66 years for males and 72 for females. Results:The cumulative incidence of patients with new clinical fractures over 2 years was 10.8% (262/2,419). In the 262 patients with subsequent fractures, we observed a higher mean age, more females and more often multiple baseline fractures compared with the 2,157 patients without subsequent fractures. Kaplan-Meier analysis indicated that age, gender and having multiple baseline fractures contributed significantly to cumulative new fracture incidence. Cox regression showed that these variables independently contributed to a higher subsequent fracture incidence. New fracture incidence was higher with increasing age ( p <0.001; hazard ratio [HR] 1.2 per decade; confidence interval [CI] 1.1–1.3). Females had a new fracture incidence of 12.2% compared with 7.4% in males ( p =0.015; HR 1.5; CI 1.1–2.0). Patients with multiple baseline fractures had a new fracture incidence of 17.3% compared with 10.4% for subjects with one baseline fracture ( p =0.006; HR 1.8; CI 1.2–2.7). Of all clinical fractures occurring within 2 years after a clinical fracture, 60% occurred during the first year and 40% during the second year ( p =0.005). The absolute risk to develop an incident clinical fracture within 2 years after any clinical fracture was 10.8%. Increased age, female gender and the presence of multiple simultaneous fractures at baseline each independently increased the risk of incident fracture. Significantly more fractures occurred in the first year following the index fracture than in the second year. Conclusion: Altogether, these data support the need for early prevention of future fracture among individuals with a fracture after age 50, using interventions which have been shown to have a rapid anti-fracture benefit.




Similar content being viewed by others
References
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Silman AJ (1995) The patient with fracture: the risk of subsequent fractures. Am J Med 98:12S–16S
Karlsson MK, Hasserius R, Obrant KJ (1993) Individuals who sustain non-osteoporotic fractures continue to also sustain fragility fractures. Calcif Tissue Int 53:229–231
van der Klift M, de Laet CE, McCloskey EV, Johnell O, Kanis JA, Hofman A, Pols HA (2004) Risk factors for incident vertebral fractures in men and women: the Rotterdam Study. J Bone Miner Res 19:1172–1180
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Torgerson DJ, Campbell MK, Thomas RE, Reid DM (1996) Prediction of perimenopausal fractures by bone mineral density and other risk factors. J Bone Miner Res 11:293–297
Port L, Center J, Briffa NK, Nguyen T, Cumming R, Eisman J (2003) Osteoporotic fracture: missed opportunity for intervention. Osteoporos Int 14:780–784
Ismail AA, O’Neill TW, Cockerill W, Finn JD, Cannata JB, Hoszowski K, Johnell O, Matthis C, Raspe H, Raspe A, Reeve J, Silman AJ (2000) Validity of self-report of fractures: results from a prospective study in men and women across Europe. EPOS Study Group. European Prospective Osteoporosis Study Group. Osteoporos Int 11:248–254
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Helden, S., Cals, J., Kessels, F. et al. Risk of new clinical fractures within 2 years following a fracture. Osteoporos Int 17, 348–354 (2006). https://doi.org/10.1007/s00198-005-2026-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-2026-x