Abstract
Introduction and hypothesis
The impact of pregnancy on pelvic floor disorders remains poorly understood. During pregnancy, an increase in ligamentous laxity and pelvic organ mobility is often reported. Our main objective was to investigate a possible association between peripheral ligamentous laxity and levator hiatus (LH) distension during pregnancy.
Methods
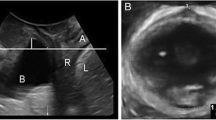
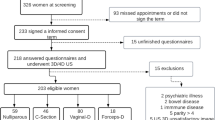
This was a prospective longitudinal study of 26 pregnant women followed up from the first to the third trimester. We collected the following information: occurrence of pelvic organ prolapse (POP) symptoms (score higher than 0 for the POP section of the Pelvic Floor Distress Inventory 20 questions score), 4D perineal ultrasound scan results with LH distension assessment and measurement of metacarpophalangeal joint mobility (MCP laxity). The association between MCP laxity and LH distension was estimated by mixed multilevel linear regression. The associations between MCP laxity and categorical parameters were estimated in a multivariate analysis using a generalized estimating equation model.
Results
MCP laxity and LH distension were correlated with a correlation coefficient of 0.26 (p = 0.02), and 6.8% of the LH distension variance was explained by MCP laxity. In the multivariate analysis, MCP laxity was associated with POP symptoms with an odds ratio at 1.05 (95% CI 1.01–1.11) for an increase of 1° in MCP laxity.
Conclusion
LH distension and peripheral ligamentous laxity are significantly associated during pregnancy. However, the relationship is weak, and the results need to be confirmed in larger populations and with more specific techniques such as elastography to directly assess the elastic properties of the pelvic floor muscles.

Similar content being viewed by others
References
Lowenstein E, Ottesen B, Gimbel H. Incidence and lifetime risk of pelvic organ prolapse surgery in Denmark from 1977 to 2009. Int Urogynecol J. 2015;26:49–55.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson FM. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123:1201–1206.
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I. Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120:152–160.
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I. The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120:144–151.
Volloyhaug I, Morkved S, Salvesen O, Salvesen K. Pelvic organ prolapse and incontinence 15–23 years after first delivery: a cross-sectional study. BJOG. 2015;122:964–971.
Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S; Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900–907.
Dietz HP, Shek C, De Leon J, Steensma AB. Ballooning of the levator hiatus. Ultrasound Obstet Gynecol. 2008;31:676–680.
Dietz HP, Clarke B, Herbison P. Bladder neck mobility and urethral closure pressure as predictors of genuine stress incontinence. Int Urogynecol J. 2002;13:289–93.
Veit-Rubin N, Cartwright R, Singh AU, Digesu GA, Fernando R, Khullar V. Association between joint hypermobility and pelvic organ prolapse in women: a systematic review and meta-analysis. Int Urogynecol J. 2016;27:1469–1478.
Mastoroudes H, Giarenis I, Cardozo L, Srikrishna S, Vella M, Robinson D, et al. Lower urinary tract symptoms in women with benign joint hypermobility syndrome: a case-control study. Int Urogynecol J. 2013;24:1553–1558.
Chen B, Yeh J. Alterations in connective tissue metabolism in stress incontinence and prolapse. J Urol. 2011;186:1768–1772.
Russek LN. Hypermobility syndrome. Phys Ther. 1999;79:591–599.
Gachon B, Desseauve D, Fradet L, Decatoire A, Lacouture P, Pierre F, et al. Changes in pelvic organ mobility and ligamentous laxity during pregnancy and postpartum. Review of literature and prospects. Prog Urol. 2016;26:385–394.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193:103–113.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23:322–330.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–17.
Dietz HP, Wong V, Shek KL. A simplified method for determining hiatal biometry. Aust N Z J Obstet Gynaecol. 2011;51:540–543.
Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32:413–418.
Jobbins B, Bird HA, Wright V. A joint hyperextensometer for the quantification of joint laxity. Eng Med. 1979;8:103–104.
Lowder JL, Debes KM, Moon DK, Howden N, Abramowitch SD, Moalli PA. Biomechanical adaptations of the rat vagina and supportive tissues in pregnancy to accommodate delivery. Obstet Gynecol. 2007;109:136–143.
Rahn DD, Ruff MD, Brown SA, Tibbals HF, Word RA. Biomechanical properties of the vaginal wall: effect of pregnancy, elastic fiber deficiency, and pelvic organ prolapse. Am J Obstet Gynecol. 2008;198:590.e1–590.e6.
Alperin M, Lawley DM, Esparza MC, Lieber RL. Pregnancy-induced adaptations in the intrinsic structure of rat pelvic floor muscles. Am J Obstet Gynecol. 2015;213:190.e1–190.e7.
Alperin M, Kaddis T, Pichika R, Esparza MC, Lieber RL. Pregnancy-induced adaptations in intramuscular extracellular matrix of rat pelvic floor muscles. Am J Obstet Gynecol. 2016;215:210.e1–210.e7.
Harvey MA, Johnston SL, Davies GA. Mid-trimester serum relaxin concentrations and post-partum pelvic floor dysfunction. Acta Obstet Gynecol Scand. 2008;87:1315–1321.
Schauberger CW, Rooney BL, Goldsmith L, Shenton D, Silva PD, Schaper A. Peripheral joint laxity increases in pregnancy but does not correlate with serum relaxin levels. Am J Obstet Gynecol. 1996;174:667–671.
Vollestad NK, Torjesen PA, Robinson HS. Association between the serum levels of relaxin and responses to the active straight leg raise test in pregnancy. Man Ther. 2012;17:225–230.
Tincello DG, Teare J, Fraser WD. Second trimester concentration of relaxin and pregnancy related incontinence. Eur J Obstet Gynecol Reprod Biol. 2003;106:237–238.
Norton PA, Allen-Brady K, Cannon-Albright LA. The familiality of pelvic organ prolapse in the Utah population database. Int Urogynecol J. 2013;24:413–418.
Cartwright R, Kirby AC, Tikkinen KA, Mangera A, Thiagamoorthy G, Rajan P, et al. Systematic review and metaanalysis of genetic association studies of urinary symptoms and prolapse in women. Am J Obstet Gynecol. 2015;212:199.e1–199.e24.
Kamisan Atan I, Gerges B, Shek KL, Dietz HP. The association between vaginal parity and hiatal dimensions: a retrospective observational study in a tertiary urogynaecological centre. BJOG. 2015;122:867–872.
Calguneri M, Bird HA, Wright V. Changes in joint laxity occurring during pregnancy. Ann Rheum Dis. 1982;41:126–128.
Kupper JC, Loitz-Ramage B, Corr DT, Hart DA, Ronsky JL. Measuring knee joint laxity: a review of applicable models and the need for new approaches to minimize variability. Clin Biomech. 2007;22:1–13.
Chen L, Low LK, DeLancey JO, Ashton-Miller JA. In vivo estimation of perineal body properties using ultrasound quasistatic elastography in nulliparous women. J Biomech. 2015;48:1575–1579.
Gennisson JL, Muller M, Gabor P, Frydman R, Musset D, Tanter M, et al. Quantification of elasticity changes in the myometrium during labor using supersonic shear imaging: a feasibility study. Ultrasonics. 2015;56:183–188.
Muller M, Ait-Belkacem D, Hessabi M, Gennisson JL, Grangé G, Goffinet F, et al. Assessment of the cervix in pregnant women using shear wave elastography: a feasibility study. Ultrasound Med Biol. 2015;41:2789–2797.
Wilson D, Dornan J, Milsom I, Freeman R. UR-CHOICE: can we provide mothers-to-be with information about the risk of future pelvic floor dysfunction? Int Urogynecol J. 2014;25:1449–1452.
Milsom I. Can we predict and prevent pelvic floor dysfunction? Int Urogynecol J. 2015;26:1719–1723.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Gachon, B., Fritel, X., Fradet, L. et al. Is levator hiatus distension associated with peripheral ligamentous laxity during pregnancy?. Int Urogynecol J 28, 1223–1231 (2017). https://doi.org/10.1007/s00192-016-3252-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3252-9