Abstract
Introduction and hypothesis
The objective was to assess the feedback from a quality improvement training programme to reduce obstetric anal sphincter injuries (OASIS).
Methods
Training sessions were organised that included evidence-based information on OASIS risk factors and training on models to measure perineal body length (PBL), perform episiotomies with standard and 60° fixed angle scissors (EPISCISSORS-60®), and measure post-delivery episiotomy suture angles with protractor transparencies. Feedback forms using a Likert scale (1–4) were completed and analysed. The setting was an evidence-based quality improvement programme (Strategy for Using Practical aids for Prevention of OASIS, Recording episiotomies and clinician Training [SUPPORT]) at two National Health Service (NHS) Hospitals in the UK. The participants were midwives and doctors attending the SUPPORT training programme
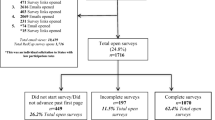
Results
All of the participants (100 %) would recommend the training programme to a friend or colleague. 92 % felt that the training session improved their knowledge of the impact of PBL and perineal distension and their knowledge of the relationship between episiotomy angle and OASIS “a lot” or “somewhat”.
Conclusion
Based on this feedback, we recommend the addition of the knowledge content of the SUPPORT programme to other centres providing perineal assessment and repair courses.
Similar content being viewed by others
References
Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington: IOM; 2001.
Ovretveit J. Does improving quality save money? A review of the evidence of which improvements to quality reduce costs to health service providers. London: Health Foundation; 2009. p. 8.
Ismail KM, Kettle C, Macdonald SE, Tohill S, Thomas PW, Bick D. Perineal Assessment and Repair Longitudinal Study (PEARLS): a matched-pair cluster randomized trial. BMC Med. 2013;11:209. doi:10.1186/1741-7015-11-209.
Mahmud A, Morris E, Johnson S, Ismail KM. Developing core patient-reported outcomes in maternity: PRO-Maternity. BJOG. 2014;121 Suppl 4:15–9. doi:10.1111/1471-0528.12901.
Royal College of Obstetricians and Gynaecologists. Third- and fourth-degree perineal tears, management (Green-top Guideline No. 29). London: RCOG; 2015.
Silf K, Woodhead N, Kelly J, Fryer A, Kettle C, Ismail KMK. Evaluation of accuracy of mediolateral episiotomy incisions using a training model. Midwife. 2014;31:197–200.
Aytan H, Tapisiz OL, Tuncay G, Avsar FA. Severe perineal lacerations in nulliparous women and episiotomy type. Eur J Obstet Gynecol Reprod Biol. 2005;121:46–50.
Dua A, Whitworth M, Dugdale A, Hill S. Perineal length: norms in gravid women in the first stage of labour. Int Urogynecol J. 2009;20:1361–4.
Geller EJ. Perineal body length as a risk factor for ultrasound-diagnosed anal sphincter tear at first delivery. Int Urogynecol J. 2014;25:631–6.
Lai CY, Cheung HW, His Lao TT, Lau TK, Leung TY. Is the policy of restrictive episiotomy generalizable? A prospective observational study. J Matern Fetal Neonatal Med. 2009;22:1116–21.
Rizk DEE, Abadir MN, Thomas LB, Abu-Zidan F. Determinants of the length of episiotomy or spontaneous perineal lacerations during vaginal birth. Int Urogynecol J. 2005;16:395–400.
Tsai PS, Oyama IA, Hiraoka M, Minaglia S, Thomas J, Kaneshiro B. Perineal body length among different racial groups in the first stage of labour. Female Pelvic Med Reconstr Surg. 2012;18:165–7.
Walfisch A, Hallak M, Harley S, Mazor M, Shoham-Vardi I. Association of spontaneous perineal stretching during delivery with perineal lacerations. J Reprod Med. 2005;50:23–8.
Laine K, Skjeldestad FE, Sandvik L, et al. Incidence of obstetric anal sphincter injuries after training to protect the perineum: cohort study. BMJ Open 2012;2:e001649. doi:10.1136/bmjopen-2012-001649.
Naidu M, Kapoor DS, Evans S, Vinayakarao L, Thakar R, Sultan AH. Cutting an episiotomy at 60 degrees: how good are we? Int Urogynecol J. 2015;26:813–6.
National Institute for Health Care and Excellence. Intrapartum care for healthy women and babies; NICE guidelines [CG190]. London: NICE; 2014.
East CE, Lau R, Biro MA. Midwives’ and doctors’ perceptions of their preparation for and practice in managing the perineum in the second stage of labour: a cross-sectional survey. Midwifery. 2015;31:122–31.
Bick DE, Ismail KM, Macdonald S, Thomas P, Tohill S, Kettle C. How good are we at implementing evidence to support the management of birth related perineal trauma? A UK wide survey of midwifery practice. BMC Pregnancy Childbirth. 2012;12:57.
Löwenstein L, Drugan A, Gonen R, Itskovitz-Eldor J, Bardicef M, Jakobi P. Episiotomy: beliefs, practice and the impact of educational intervention. Eur J Obstet Gynecol Reprod Biol. 2005;123:179–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Rahman, N., Vinayakarao, L., Pathak, S. et al. Evaluation of training programme uptake in an attempt to reduce obstetric anal sphincter injuries: the SUPPORT programme. Int Urogynecol J 28, 403–407 (2017). https://doi.org/10.1007/s00192-016-3158-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3158-6