Abstract
Introduction and hypothesis
There has been increasing media attention regarding transvaginal mesh (TVM). We hypothesized that new urogynecology patients have limited knowledge and negative opinions of TVM.
Methods
An anonymous survey was distributed to all new patients presenting to the Mt Auburn Hospital urogynecology practice from 1 November 2012 to 31 January 2013. A total of 146 patients completed the questionnaire. The survey was designed to elicit information on participants’ knowledge and opinions about TVM and knowledge about recent FDA safety communications. All statistical tests were two-sided, and P values <0.05 were considered statistically significant.
Results
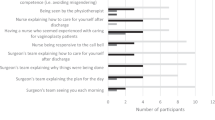
Analyses were restricted to the 77 women who had either heard of TVM or were unsure if they had heard of TVM. A minority (32.5 %) of these women correctly defined TVM, and 33.8 % had a negative impression of TVM. Respondents obtained their information on TVM from the media (48.1 %), the Internet (24.7 %), family or friends (22.1 %), and health care providers (18.2 %). The majority (71.4 %) agreed that they needed more information about TVM before making any decisions about using it to treat their condition. Nearly one quarter of respondents (23.4 %) agreed that they would not want their doctor to use TVM on them for any reason. When asked about recent FDA communications, 27.3 % of patients correctly responded that the FDA had released a safety communication regarding TVM.
Conclusions
The majority of participants had limited knowledge of TVM; however, only a minority had negative opinions. Given our findings, it is important that providers spend more time during the consent process explaining TVM and its risks and benefits as a treatment option.

Similar content being viewed by others
References
Olsen AL, Smith VJ, Bergstrom JO et al (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Smith FJ, Holman CD, Moorin RE et al (2010) Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol 116:1096–1100
Hendrix SL, Clark A, Nygaard I et al (2002) Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol 186:1160–1166
Rogo-Gupta L, Rodriguez LV, Litwin MS et al (2012) Trends in surgical mesh use for pelvic organ prolapse from 2000 to 2010. Obstet Gynecol 120:1105–1115
Hiltunen R, Nieminen K, Takala T et al (2007) Low-weight polypropylene mesh for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol 110:455–462
Julian TM, Grody T (1996) The efficacy of Marlex mesh in the repair of severe, recurrent vaginal prolapse of the anterior midvaginal wall. Am J Obstet Gynecol 175:1472–1475
Bai SW, Jung HJ, Jeon MJ et al (2007) Surgical repair of anterior wall vaginal defects. Int J Gynaecol Obstet 98:147–150
Maher C, Feiner B, Baessler K et al (2013) Surgical management of pelvic organ prolapse in women (review). Cochrane Database Sys Rev (3):CD004014
Iglesia CB (2011) Synthetic vaginal mesh for pelvic organ prolapse. Curr Opin Obstet Gynecol 23:362–365
FDA Public Health Notification: serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. 20 October 2008. Available at: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm061976.htm. Accessed 11 November 2014
FDA Safety Communication: update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. 13 July 2011. Available at: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm. Accessed 11 November 2014
Mucowski SJ, Jurnalov C, Phelps JY et al (2010) Use of vaginal mesh in the face of recent FDA warnings and litigation. Am J Obstet Gynecol 203:103e.1–103e.4
Gomelsky A, Dmochowski RR (2012) Vaginal mesh update. Curr Opin Urol 22:271–275
Clemons JL, Weinstein M, Guess MK et al (2013) Impact of the 2011 FDA transvaginal mesh safety update on AUGS members’ use of synthetic mesh and biologic grafts in pelvic reconstructive surgery. Female Pelvic Med Reconstr Surg 194:191–196
American College of Obstetricians and Gynecologists (2011) Committee opinion no. 513: vaginal placement of synthetic mesh for pelvic organ prolapse. Obstet Gynecol 118:1459–1464
Reynolds WS, Gold KP, Ni S et al (2013) Immediate effects of the initial FDA notification on the use of surgical mesh for pelvic organ prolapse surgery in Medicare beneficiaries. Neurourol Urodyn 32:330–335
Conflicts of interest
Dr. Rosenblatt is a consult for American Medical Systems, Bard, Boston Scientific, Coloplast and Ethicon. He receives research funding from Boston Scientific and Coloplast and has a licensing agreement with for American Medical Systems.
Sources of financial support
Harvard Catalyst, the Harvard Clinical and Translational Science Center (NIH Award #UL1 RR 025758 and financial contributions from Harvard University and its affiliated academic health care centers).
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix



Rights and permissions
About this article
Cite this article
Dessie, S.G., Hacker, M.R., Haviland, M.J. et al. Attitudes toward transvaginal mesh among patients in a urogynecology practice. Int Urogynecol J 26, 865–873 (2015). https://doi.org/10.1007/s00192-014-2607-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2607-3