Abstract
Introduction and hypothesis
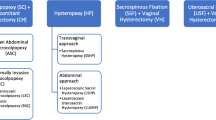
Laparoscopic techniques for pelvic organ prolapse surgery using mesh are gaining interest. A standard approach or published guideline for the laparoscopic sacrohysteropexy (LSH) or laparoscopic sacrocolpopexy (LSC) is lacking. The purpose of this study is to assess the variation between Dutch gynecologists in executing LSH and LSC.
Methods
A questionnaire was developed to evaluate the technique of LSH and LSC. All members of the Dutch Society for Gynecological Endoscopy and Minimally Invasive Surgery and the Dutch Society for Urogynecology were invited by email to participate in a web-based survey.
Results
With 357 respondents, the response rate was 71 %. Of the respondents, a total of 49 gynecologists (13.7 %) perform LSH and/or LSC. Gynecologists who perform both procedures use the same surgical technique for LSH and LSC. There are variations among gynecologists on several key points such as the level of dissection along the anterior and posterior walls of the vagina, the type of mesh used, the type of sutures used, the tension of the implanted mesh and reperitonealization of the mesh.
Conclusions
There is a high practice variation in LSH and LSC performed by a selected group of Dutch gynecologists. Different methods have been described in the literature and there is no consensus on how to perform these procedures. A well-designed prospective study or randomized controlled trial with regard to the specific parts of these procedures is needed to provide evidence for the best surgical technique. The outcomes of these studies will help to establish evidence-based guidelines.
Similar content being viewed by others
References
Smith FJ, Holman CD, Moorin RE, Tsokos N (2010) Life time risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol 116(5):1096–1100
Rogo-Gupta L, Rodriguez LV, Litwin MS, Herzog TJ, Neugut AI, Lu YS, Raz S, Hershman DL, Wright JD (2012) Trends in surgical mesh use for pelvic organ prolapse from 2000 to 2010. Obstet Gynecol 120(5):1105–1115
Food and Drug Administration (2011) FDA Safety communication: UPDATE on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm. Accessed 13 July 2011
Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. doi:10.1002/14651858.CD004014.pub5
Leron E, Stanton SL (2001) Sacrohysteropexy with synthetic mesh for the management of uterovaginal prolapse. BJOG 108(6):629–633
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, Zyczynski H (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104(4):805–823
Rosenblatt PL, Chelmow D, Ferzandi TR (2008) Laparoscopic sacrocervicopexy for the treatment of uterine prolapse: a retrospective case series report. J Minim Invasive Gynecol 15(3):268–272
Nezhat CH, Nezhat F, Nezhat C (1994) Laparoscopic sacrocolpopexy for vaginal vault prolapse. Obstet Gynecol 84(5):885–888
Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L, Moran P, Slack M, Scott P, Waterfield M (2013) A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J 24(3):377–384
Coolen AL, van Oudheusden AM, van Eijndhoven HW, van der Heijden TP, Stokmans RA, Mol BW, Bongers MY (2013) A comparison of complications between open abdominal sacrocolpopexy and laparoscopic sacrocolpopexy for the treatment of vault prolapse. Obstet Gynecol Int 2013:528636 doi:10.1155/2013/528636
Pollard ME, Eilber KS, Anger JT (2013) Abdominal approaches to pelvic prolapse repairs. Curr Opin Urol 23:306–311
Sarlos D, Kots L, Rye G, Schaer G (2014) Longterm follow-up of laparoscopic sacrocolpopexy. Int Urogynecol J 25(9):1207–1212
Rahmanou P, Price N, Jackson S (2014) Laparoscopic hysteropexy: a novel technique for uterine preservation. Int Urogynecol J 25(1):139–140
Won H, Maley P, Salim S, Rao A, Campbell NT, Abbott JA (2013) Surgical and patient outcomes using mechanical bowel preparation before laparoscopic gynecological surgery: a randomized controlled trial. Obstet Gynecol 121(3):538–546
Siedhoff MT, Clark LH, Hobbs KA, Findley AD, Moulder JK, Garrett JM (2014) Mechanical bowel preparation before laparoscopic hysterectomy: a randomized controlled trial. Obstet Gynecol 123:562–567
Ramanah R, Ballester M, Chereau E, Bui C, Rouzier R, Daraï E (2012) Anorectal symptoms before and after laparoscopic sacrocolpoperineopexy for pelvic organ prolapse. Int Urogynecol J 23(6):779–783
De Tayrac R, Sentilhes L (2013) Complications of pelvic organ prolapse surgery and methods of prevention. Int Urogynecol J 24(11):1859–1872
Antiphon P, Elard S, Benyoussef A, Fofana M, Yiou R, Gettman M, Hoznek A, Vordos D, Chopin DK, Abbou CC. Laparoscopic promontory sacral colpopexy: is the posterior, recto-vaginal mesh mandatory? Eur Urol 45(5):655–661
Boukerrou M, Orazi G, Nayama M, Boodhun R, Crépin G, Cosson M (2003) Promontofixation procedure: use of non-absorbable sutures or tackers. J Gynecol Obstet Biol Reprod 32(6):524–528
Parkes IL, Shveiky D (2014) Sacrocolpopexy for the treatment of vaginal apical prolapse: evidence based surgery. J Minim Invasive Gynecol 21(4):546–557
Elneil S, Cutner AS, Remy M, Leather AT, Toozs-Hobson P, Wise B (2005) Abdominal sacrocolpopexy for vault prolapse without burial of mesh: a case series. BJOG 112(4):486–489
Frenkl TL, Rackley RR, Vasavada SP, Goldman HB (2008) Management of iatrogenic foreign bodies of the bladder and urethra following pelvic floor surgery. Neurourol Urodyn 27(6):491–495
Maher C, Feiner B (2011) Laparoscopic removal of intravesical mesh following pelvic organ prolapse mesh surgery. Int Urogynecol J 22(12):1593–1595
Manchouri E, Cohen SL, Sandberg EM, Kibel AS, Einarsson J (2012) Ureteral injury in laparoscopic gynecologic surgery. Rev Obstet Gynecol 5(2):106–111
Sandberg EM, Cohen SL, Hurwitz S, Einarsson JI (2012) Utility of cystoscopy during hysterectomy. Obstet Gynecol 120(6):1363–1370
Dimitri S, Thomas A, Gabriel S (2014) Laparoscopic sacrocolpopexy with deep attachment of anterior and posterior mesh. Int Urogynecol J 25(11):1591–1592
Shippey SH, Quiroz LH, Sanses TV, Knoepp LR, Cundiff GW, Handa VL (2010) Anatomic outcomes of abdominal sacrocolpopexy with or without paravaginal repair. Int Urogynecol J 21(3):279–283
Guiahi M, Kenton K, Brubaker L (2008) Sacrocolpopexy without concomitant posterior repair improves posterior compartment defects. Int Urogynecol J Pelvic Floor Dysfunct 19(9):1267–1270
Crane AK, Geller EJ, Matthews CA (2013) Outlet constipation 1 year after robotic sacrocolpopexy with and without concomitant posterior repair. South Med J 106(7):409–414
Lensen EJM, Stoutjesdijk JA, Withagen MIJ, Kluivers KB, Vierhout ME (2011) Technique of anterior colporrhaphy: a Dutch evaluation. Int Urogynecol J 22:557–561
Conflicts of interest
None.
Ethical/institutional review board approval
Not applicable, since this study does not involve patients (not obligatory according to the Dutch law [WMO]).
Author information
Authors and Affiliations
Corresponding author
Additional information
Wilbert A. Spaans and Hugo W. F. van Eijndhoven contributed equally to the manuscript
Rights and permissions
About this article
Cite this article
van IJsselmuiden, M.N., Kerkhof, M.H., Schellart, R.P. et al. Variation in the practice of laparoscopic sacrohysteropexy and laparoscopic sacrocolpopexy for the treatment of pelvic organ prolapse: a Dutch survey. Int Urogynecol J 26, 757–764 (2015). https://doi.org/10.1007/s00192-014-2591-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2591-7