Abstract
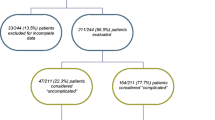
Voiding difficulty has been relatively overlooked as a diagnosis. Previous estimates of its prevalence have generally been no more than 14% with one exception at 24%. The aim of this study is to determine the true prevalence and associations of voiding difficulty using a validated definition [urine flow rate under 10th centile of the Liverpool Nomograms and/or residual urine volume (by transvaginal ultrasound) more than 30 ml]. This study involved 592 women referred for an initial urogynecological assessment including urodynamics. Data were separated according to the presence or absence of voiding difficulty. The prevalence of voiding difficulty was 39%, far higher than previous estimates. It is the third most common urodynamic diagnosis behind urodynamic stress incontinence (USI—72%) and uterine/vaginal prolapse (61%) and ahead of the overactive bladder (13%). Voiding difficulty significantly increased in prevalence with age and increasing grades of all types of uterine/vaginal prolapse. Prolapse appeared to be the main factor in the age deterioration. Other significant positive relationships with voiding difficulty were prior hysterectomy and prior continence surgery, whilst USI and the symptom and sign of stress incontinence had significant inverse relationships.


Similar content being viewed by others
References
Sutherst JR, Frazer MI, Richmond DH, Haylen BT (1990) Introduction to clinical gynaecological urology. Butterworths, London, p 121
Stanton SL, Ozsoy D, Hilton P (1983) Voiding difficulties in the female: prevalence, clinical and urodynamics review. Obstet Gynecol 61:144–147
Groutz A, Blaivas JG, Chaikin DC (2000) Bladder outflow obstruction in women: definition and characteristics. Neurourol Urodyn 19:213–220
Massey JA, Abrams PH (1988) Obstructed voiding in the female. Br J Urol 61:36–39
Costantini E, Mearini E, Pajoncini C et al (2003) Uroflowmetry in female voiding disturbances. Neurourol Urodyn 22:569–573
Haylen BT, Ashby, D, Sutherst, JR et al (1989) Maximum and average urine flow rates in normal male and female populations—the Liverpool Nomograms. Brit J Urol 64:30–38
Haylen BT, Parys BT, Anyaegbunam WI et al (1990) Urine flow rates in male and female urodynamics patients compared with the Liverpool Nomograms. Brit J Urol 65:483–487
Haylen BT, Law, MG, Frazer M, Schulz S (1999) Urine flow rates and residual urine volumes in urogynaecology patients. Int Urogynecol J 10:378–383
Versi E, Harvey MA, Hudson LB (1999) The symptom of voiding dysfunction: its predictive value in the diagnosis of emptying function disorder. Urogynaecologia 2:71
Haylen BT (1989) Residual urine volumes in a normal female population: an application of transvaginal ultrasound. Br J Urol 64:347–349
O’Grady F, Cattell WR (1966) Kinetics of urinary tract infection. II. The bladder. Br J Urol 38:156–162
Haylen BT, Parys BT, Verity L, Schulz S, Zhou J, Law MG, Sutherst JR (2005) Can we identify the women more likely to experience recurrent UTI. Int Urogynecol J 16(Suppl 2):S45
Yang A, Mostwin J, Genadry R, Sanders R (1993) Patterns of prolapse demonstrated with dynamic fastscan MRI: reassessment of conventional concepts of pelvic floor weaknesses. Neurourol Urodyn 12:310
Bump R, Bo K, Brubaker L et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10
Haylen BT, Frazer MI, Sutherst JR, West CR (1989) Transvaginal ultrasound in the assessment of bladder volumes in women. Preliminary report. Br J Urol 63:149–151
Haylen BT (1989) Verification of the accuracy and range of transvaginal ultrasound in measuring bladder volumes in women. Br J Urol 64:350–352
Fantl JA, Smith PJ, Schneider V et al (1982) Fluid weight uroflowmetry in women. Am J Obstet Gynecol 145:1017–1024
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten et al (2003) The standardisation of terminology of lower urinary tract function. Report from the standardisation subcommittee of the International Continence Society. Urology 61:37–49
Ryall RL, Marshall VR (1982) The effect of urinary catheter on the measurement of maximum urinary flow rate. J Urol 128:429–432
Rosenzweig BA (1993) Genital prolapse and lower urinary tract dysfunction. Int Urogynecol J 4:296–300
Parys BT, Haylen BT, Woolfenden KA, Parsons KF (1989) Vesico-urethral dysfunction after simply hysterectomy. Neurourol Urodyn 8:315–316
Ulmsten UJ, Johnson P, Rezapour M (1999) A three-year follow-up of tension-free vaginal tape for surgical treatment of stress urinary incontinence. Br J Obstet Gynaecol 106:345–350
Groutz A, Gordon D, Avni A, Lessing JB, David MP (1998) Subjective symptoms of voiding difficulties—are they substantiated by objective urodynamics data? Neurourol Urodyn 17(4):430–431
Salvatore S, Khullar V, Cardozo L, Digesu AG, Soligo M, Lalia M, Milani R (2000) Urodynamic studies in obstructed women. Neurourol Urodyn 19(4):480–481
Haylen BT (2000) Voiding difficulty in women (editorial). Int Urogynecol J 11(1):1–3
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haylen, B.T., Krishnan, S., Schulz, S. et al. Has the true prevalence of voiding difficulty in urogynecology patients been underestimated?. Int Urogynecol J 18, 53–56 (2007). https://doi.org/10.1007/s00192-006-0094-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-006-0094-x