Abstract
Purpose
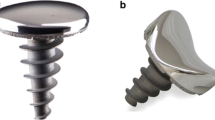
The UniCAP® implant for femoral resurfacing treatment of large cartilage lesions and early OA was introduced in 2006. The outcome of the present study is from a prospective cohort study of 64 patients, followed 2 years clinically and 7 years for revisions.
Methods
From 2009 to 2013, 64 patients were treated with femoral resurfacing using the UniCAP implant. Indication for treatment with UniCAP implant was symptomatic huge cartilage lesion or early OA at the femoral condyle demonstrated by MRI or arthroscopy, which was ICRS grades 3–4 and more than 4 cm2. There were 28 males and 36 females with a median age of 51 (range 35–65) years. Patients were followed for 2 years clinically with Knee Society subjective outcome scores (KSS), pain scores and radiographic evaluations and for 7 years with complications and reoperations.
Results
At 2 years, the follow-up mean KSS improved from 49 (6.9) to 88 (17.1), the mean KSS function score improved from 46 (8.0) to 90 (17.1), and the mean Pain score improved from 7.4 (0.5) to 2.3 (1.4). 47 % of the implants were revised within 7 years to arthroplasty due to the progression of cartilage lesions, progressing of osteoarthritis or increased knee pain. The reoperation rate did not show any significant difference between females and males. The Kaplan–Meier survival rate was 50 % at 7 years, no difference among females and males.
Conclusion
The present study demonstrated an improved subjective outcome and reduced pain after femoral resurfacing using the UniCAP® implant in a relatively large cohort of patients with symptomatic large cartilage lesions or early OA. A 47 % reoperation rate with conversion to arthroplasty was found. The femoral resurfacing implantation can be a temporary treatment for large cartilage lesions or early OA that is expected to develop into osteoarthritis. For younger patients who are ineligible for arthroplasty treatment, this implant can offer a temporary solution.
Level of evidence
IV.




Similar content being viewed by others
References
Australian Orthopaedic Association National Joint Replacement Registry (2013) Annual report, pp 108–109
Becher C, Huber R, Thermann H, Ezechieli L, Ostermeier S, Wellmann M, von Skrbensky G (2011) Effects of a surface matching articular resurfacing device on tibiofemoral contact pressure: results from continuous dynamic flexion-extension cycles. Arch Orthop Trauma Surg 131:413–419
Becher C, Kalbe C, Thermann H, Paessler HH, Laprell H, Kaiser T, Fechner A, Bartsch S, Windhagen H, Ostermeier S (2011) Minimum 5-year results of focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee. Arch Orthop Trauma Surg 131:1135–1143
Bollars P, Bosquet M, Vandekerckhove B, Hardeman F, Bellemans J (2012) Prosthetic inlay resurfacing for the treatment of focal, full thickness cartilage defects of the femoral condyle: a bridge between biologics and conventional arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:1753–1759
Brennan SA, Devitt BM, O’Neill CJ, Nicholson P (2013) Focal femoral condyle resurfacing. Bone Joint J 95-B:301–304
Cicuttini F, Ding C, Wluka A, Davis S, Ebeling PR, Jones G (2005) Association with cartilage defects with loss of knee cartilage in healthy, middle-age adults: a prospective study. Arthritis Rheum 52:2033–2039
Danish Orthopaedic Association (DOS) (2013) National Joint Replacement Registry (DKR) Annual report
Guettler JH, Demetropoulos CK, Yang KH, Jurist KA (2004) Osteochondral defects in the human knee:influence of defect size on cartilage rim stress and load redistribution to surrounding cartilage. Am J Sports Med 32(6):1451–1458
Görtz S, Bugbee WD (2006) Allografts in articular cartilage repair. J Bone Joint Surg Am 88(6):1374–1384
Hangody L, Fules P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am 85A(Suppl 2):25–32
Heir S, Nerhus TK, Rotterud JH, Loken S, Ekeland A, Engebretsen L, Aroen A (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38:231–237
Hjelle K, Solheim E, Strand T, Muri R, Brittberg M (2002) Articular cartilage defects in 1.000 knee arthroscopies. Arthroscopy 18(7):730–734
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Kirker-Head CA, Van Sickle DC, Ek SW, McCool JC (2006) Safety of, and biological and functional response to, a novel metallic implant for the management of focal full-thickness cartilage defects: preliminary assessment in an animal model out to 1 year. J Orthop Res 24:1095–1108
Kreuz PC, Erggelet C, Steinwachs MR, Krause SJ, Lahm A, Niemeyer P, Ghanem N, Uhl M, Sudkamp N (2006) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy 22:1180–1186
Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M, Südkamp N (2006) Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage 14(11):1119–1125
Laprell H, Petersen W (2001) Autologous osteochondral transplantation using the diamond bone-cutting system (DBCS): 6-12 years’ follow-up of 35 patients with osteochondral defects at the knee joint. Arch Orthop Trauma Surg 121(5):248–253
Laursen JO, Lind M (2015) Treatment of full-thickness femoral cartilage lesions using condyle resurfacing prosthesis. Knee Surg Sports Traumatol Arthrosc. doi:1007/s00167-05-3726-1
Li CS, Karlsson J, Winemaker M, Sancheti P, Bhandari M (2014) Orthopedic surgeons feel that there is a treatment gap in management of early OA: international survey. Knee Surg Sports Traumatol Arthrosc 22(2):363–378
London NJ, Miller LE, Block JE (2011) Clinical and economic consequences of the treatment gap in knee osteoarthritis management. Med Hypotheses 76:887–892
Micheli LJ, Browne JE, Erggelet CF, Fu F, Mandelbaum B, Moseley JB, Zurakowski D (2001) Autologous chondrocyte implantation of the knee: multicenter experience and minimum 3-year follow-up. Clin J Sports Med 11(4):223–228
Miniaci A (2014) UniCAP as an alternative for unicompartmental arthritis. Clin Sports Med 33(1):57–65
Mithoefer K, Williams RJ 3rd, Warren RF, Potter HG, Spock CR, Jones EC (2005) The microfracture technique for the treatment of articular cartilage lesions in the knee: a prospective cohort study. JBJS Am 87(9):1911–1920
Morelli M, Nagamori J, Miniaci A (2002) Management of chondral injuries of the knee by osteochondral autogenous transfer (mosaicplasty). J Knee Surg 15:185–190
Skrbensky G, Becher C, Schmidt M (2008) Resurfacing for sportive patients: HemiCAP results and biomechanic in vitro tests. In: SICOT/SIROT 2008 XXIV triennial world congress, 24–28 August 2008, Hong Kong
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: 11-year follow-up. J Arthroscopy 19:477–480
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laursen, J.O. Treatment of full-thickness cartilage lesions and early OA using large condyle resurfacing prosthesis: UniCAP® . Knee Surg Sports Traumatol Arthrosc 24, 1695–1701 (2016). https://doi.org/10.1007/s00167-016-4000-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4000-x