Abstract
Purpose
Despite its effectiveness in other surgeries, studies on continuous epidural block in upper-extremity surgery are rare because of technical difficulties and potential complications. This study compared postoperative analgesic efficacy and safety of ultrasound-guided continuous interscalene brachial plexus block (UCISB) and fluoroscopy-guided targeted continuous cervical epidural block (FCCEB) in arthroscopic rotator cuff repair (ARCR).
Methods
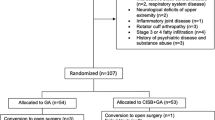
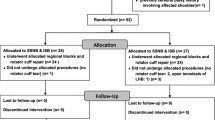
Seventy-five patients were randomly and equally assigned to groups FCCEB (0.2 %), UCISB75 (0.75 %), and UCISB20 (0.2 %) according to the initial ropivacaine dose (8 ml). The background infusion (0.2 % ropivacaine at 5 ml/h), bolus (3 ml of 0.2 % ropivacaine), and lockout time (20 min) were consistent. Respiratory effects [respiratory discomfort (modified Borg scale), ventilatory function, and hemidiaphragmatic excursion (ultrasound)], analgesic quality [pain severity at rest and motion attempt (VAS-R and -M), number of boluses, analgesic supplements, and sleep disturbance], neurologic effects, procedural discomfort, satisfaction, and adverse effects were evaluated preprocedurally and up to 72 h postoperatively.
Results
FCCEB caused less respiratory depression and sensorimotor block, but had less analgesic efficacy than UCISBs (P < 0.05). FCCEB caused nausea, vomiting, and dizziness more frequently (P < 0.05) and had lower patient satisfaction than UCISBs (P < 0.05). UCISB75 can cause severe respiratory distress in patients with lung disorders. Other variables were not significantly different between the groups.
Conclusions
UCISB20 may provide superior postoperative analgesia and is the most recommendable postoperative analgesic method in ARCR.
Level of evidence
Randomized controlled trials, Therapeutic study, Level I.



Similar content being viewed by others
References
Antonakakis JG, Sites BD, Shiffrin J (2009) Ultrasound-guided posterior approach for the placement of a continuous interscalene catheter. Reg Anesth Pain Med 34:64–68
Bedforth NM, Hardman JG (2010) The hidden cost of neuraxial anaesthesia? Anaesth 65:437–439
Bettmann MA (2005) Contrast media: safety, viscosity, and volume. Eur Radiol 15(Suppl 4):D62–D64
Bonnet F, Derosier JP, Pluskwa F, Abhay K, Gaillard A (1990) Cervical epidural anaesthesia for carotid artery surgery. Can J Anaesth 37:353–358
Borene SC, Rosenquist RW, Koorn R, Haider N, Boezaart AP (2003) An indication for continuous cervical paravertebral block (posterior approach to the interscalene space). Anesth Analg 97:898–900
Borgeat A, Ekatodramis G, Guzzella S, Ruland P, Votta-Velis G, Aguirre J (2012) Deltoid, triceps, or both responses improve the success rate of the interscalene catheter surgical block compared with the biceps response. Br J Anaesth 109:975–980
Boussuges A, Gole Y, Blanc P (2009) Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values. Chest 135:391–400
Buchheit T, Crews JC (2000) Lateral cervical epidural catheter placement for continuous unilateral upper extremity analgesia and sympathetic block. Reg Anesth Pain Med 25:313–317
Cho CH, Song KS, Min BW, Jung GH, Lee YK, Shin HK (2015) Efficacy of interscalene block combined with multimodal pain control for postoperative analgesia after rotator cuff repair. Knee Surg Sports Traumatol Arthrosc 23:542–547
Cho YH, Shin SH, Lee DH, Yu EY, Yoon MS (2009) The effect of preoperative interscalene block using low-dose mepivacaine on the postoperative pain after shoulder arthroscopic surgery. Korean J Pain 22:224
Davies RG, Myles PS, Graham JM (2006) A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy—a systematic review and meta-analysis of randomized trials. Br J Anaesth 96:418–426
Forster JG, Niemi TT, Salmenpera MT, Ikonen S, Rosenberg PH (2009) An evaluation of the epidural catheter position by epidural nerve stimulation in conjunction with continuous epidural analgesia in adult surgical patients. Anesth Analg 108:351–358
Fredrickson MJ, Krishnan S, Chen CY (2010) Postoperative analgesia for shoulder surgery: a critical appraisal and review of current techniques. Anaesth 65:608–624
Fredrickson MJ, Stewart AW (2008) Continuous interscalene analgesia for rotator cuff repair: a retrospective comparison of effectiveness and cost in 205 patients from a multi-provider private practice setting. Anaesth Intensive Care 36:786–791
Grider JS, Mullet TW, Saha SP, Harned ME, Sloan PA (2012) A randomized, double-blind trial comparing continuous thoracic epidural bupivacaine with and without opioid in contrast to a continuous paravertebral infusion of bupivacaine for post-thoracotomy pain. J Cardiothorac Vasc Anesth 26:83–89
Ilfeld BM, Moeller LK, Mariano ER, Loland VJ, Stevens-Lapsley JE, Fleisher AS, Girard PJ, Donohue MC, Ferguson EJ, Ball ST (2010) Continuous peripheral nerve blocks: is local anesthetic dose the only factor, or do concentration and volume influence infusion effects as well? Anesthesiology 112:347–354
Ip VH, Tsui BC (2012) Continuous interscalene block: the good, the bad and the refined spread. Acta Anaesthesiol Scand 56:526–530
Joshi GP, Bonnet F, Shah R, Wilkinson RC, Camu F, Fischer B, Neugebauer EA, Rawal N, Schug SA, Simanski C, Kehlet H (2008) A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth Analg 107:1026–1040
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367:1618–1625
Kim YI, Nam SG, Hong ST, Kang KS, Park W (2001) Comparison of visual analogue scale, categorical scale and satisfaction for postoperative pain. Korean J Pain 14:156–163
Liu SS, Bieltz M, Wukovits B, John RS (2010) Prospective survey of patient-controlled epidural analgesia with bupivacaine and hydromorphone in 3736 postoperative orthopedic patients. Reg Anesth Pain Med 35:351–354
McNaught A, Shastri U, Carmichael N, Awad IT, Columb M, Cheung J, Holtby RM, McCartney CJ (2011) Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth 106:124–130
Narouze SN, Govil H, Guirguis M, Mekhail NA (2009) Continuous cervical epidural analgesia for rehabilitation after shoulder surgery: a retrospective evaluation. Pain Physician 12:189–194
Nystrom UM, Nystrom NA (1997) Continuous cervical epidural anesthesia in reconstructive hand surgery. J Hand Surg Am 22:906–912
Oh JH, Kim WS, Kim JY, Gong HS, Rhee KY (2007) Continuous intralesional infusion combined with interscalene block was effective for postoperative analgesia after arthroscopic shoulder surgery. J Shoulder Elbow Surg 16:295–299
Oh JH, Rhee KY, Kim SH, Lee PB, Lee JW, Lee SJ (2009) Comparison of analgesic efficacy between single interscalene block combined with a continuous intra-bursal infusion of ropivacaine and continuous interscalene block after arthroscopic rotator cuff repair. Clin Orthop Surg 1:48–53
Prusinkiewicz C, Lang S, Tsui BC (2005) Lateral cervical epidural catheter placement using nerve stimulation for continuous unilateral upper extremity analgesia following a failed continuous peripheral nerve block. Acta Anaesthesiol Scand 49:579–582
Rawal N (2012) Epidural technique for postoperative pain: gold standard no more? Reg Anesth Pain Med 37:310–317
Renes SH, van Geffen GJ, Rettig HC, Gielen MJ, Scheffer GJ (2010) Minimum effective volume of local anesthetic for shoulder analgesia by ultrasound-guided block at root C7 with assessment of pulmonary function. Reg Anesth Pain Med 35:529–534
Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ (2008) Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth 101:549–556
Ryu HG, Bahk JH, Lee CJ, Lim YJ (2007) The coiling length of thoracic epidural catheters: the influence of epidural approach angle. Br J Anaesth 98:401–404
Sandefo I, Bernard JM, Elstraete V, Lebrun T, Polin B, Alla F, Poey C, Savorit L (2005) Patient-controlled interscalene analgesia after shoulder surgery: catheter insertion by the posterior approach. Anesth Analg 100:1496–1498
Scarci M, Joshi A, Attia R (2010) In patients undergoing thoracic surgery is paravertebral block as effective as epidural analgesia for pain management? Interact CardioVasc Thorac Surg 10:92–96
Stevens RA, Frey K, Sheikh T, Kao TC, Mikat-Stevens M, Morales M (1998) Time course of the effects of cervical epidural anesthesia on pulmonary function. Reg Anesth Pain Med 23:20–24
Tsui BC, Bateman K, Bouliane M, Finucane B (2004) Cervical epidural analgesia via a thoracic approach using nerve stimulation guidance in an adult patient undergoing elbow surgery. Reg Anesth Pain Med 29:355–360
Tsui BC, Bury J, Bouliane M, Ganapathy S (2007) Cervical epidural analgesia via a thoracic approach using nerve-stimulation guidance in adult patients undergoing total shoulder replacement surgery. Acta Anaesthesiol Scand 51:255–260
Tuominen M, Pitkanen M, Rosenberg PH (1987) Postoperative pain relief and bupivacaine plasma levels during continuous interscalene brachial plexus block. Acta Anaesthesiol Scand 31:276–278
Urmey WF, McDonald M (1992) Hemidiaphragmatic paresis during interscalene brachial plexus block: effects on pulmonary function and chest wall mechanics. Anesth Analg 74:352–357
Wilson AT, Nicholson E, Burton L, Wild C (2004) Analgesia for day-case shoulder surgery. Br J Anaesth 92:414–415
Wittich DJ Jr, Berny JJ, Davis RK (1984) Cervical epidural anesthesia for head and neck surgery. Laryngoscope 94:615–619
Yang CW, Jung SM, Kwon HU, Cho CK, Yi JW, Kim CW, Jung JK, An YM (2010) A clinical comparison of continuous interscalene brachial plexus block with different basal infusion rates of 0.2 % ropivacaine for shoulder surgery. Korean J Anesthesiol 59:27–33
Acknowledgments
This research was supported by Chung-Ang University Research Grants in 2011.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, JY., Song, KS., Kim, WJ. et al. Analgesic efficacy of two interscalene blocks and one cervical epidural block in arthroscopic rotator cuff repair. Knee Surg Sports Traumatol Arthrosc 24, 931–939 (2016). https://doi.org/10.1007/s00167-015-3667-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3667-8