Abstract
Purpose
Early mobilization within 72 h of intensive care unit (ICU) admission improves functional status at hospital discharge. We aimed to assess the effectiveness of early, goal-directed mobilization in critically ill patients across a broad spectrum of initial consciousness levels.
Methods
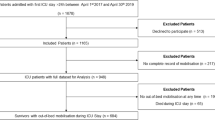
Post hoc analysis of the international, randomized, controlled, outcome-assessor blinded SOMS trial conducted 2011–2015. Randomization was stratified according to the immediate post-injury Glasgow Coma Scale (GCS) (≤ 8 or > 8). Patients received either SOMS-guided mobility treatment with a facilitator or standard care. We used general linear models to test the hypothesis that immediate post-randomization GCS modulates the intervention effects on functional independence at hospital discharge.
Results
Two hundred patients were included in the intention-to-treat analysis. The significant effect of early, goal-directed mobilization was consistent across levels of GCS without evidence of effect modification, for the primary outcome functional independence at hospital discharge (p = 0.53 for interaction), as well as average achieved mobility level during ICU stay (mean achieved SOMS level) and functional status at hospital discharge measured with the functional independence measure. In patients with low GCS, delay to first mobilization therapy was longer (0.7 ± 0.2 days vs. 0.2 ± 0.1 days, p = 0.008), but early, goal-directed mobilization compared with standard care significantly increased functional independence at hospital discharge in this subgroup of patients with immediate post-randomization GCS ≤ 8 (OR 3.67; 95% CI 1.02–13.14; p = 0.046).
Conclusion
This post hoc analysis of a randomized controlled trial suggests that early, goal-directed mobilization in patients with an impaired initial conscious state (GCS ≤ 8) is not harmful but effective.



Similar content being viewed by others
References
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, McCallister KE, Hall JB, Kress JP (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373:1874–1882
Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, Heim M, Houle T, Kurth T, Latronico N, Lee J, Meyer MJ, Peponis T, Talmor D, Velmahos GC, Waak K, Walz JM, Zafonte R, Eikermann M, International Early S-gMRI (2016) Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 388:1377–1388
von Bornstadt D, Houben T, Seidel JL, Zheng Y, Dilekoz E, Qin T, Sandow N, Kura S, Eikermann-Haerter K, Endres M, Boas DA, Moskowitz MA, Lo EH, Dreier JP, Woitzik J, Sakadzic S, Ayata C (2015) Supply-demand mismatch transients in susceptible peri-infarct hot zones explain the origins of spreading injury depolarizations. Neuron 85:1117–1131
Group ATC, Bernhardt J, Langhorne P, Lindley RI, Thrift AG, Ellery F, Collier J, Churilov L, Moodie M, Dewey H, Donnan G (2015) Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial. Lancet 386:46–55
Langhorne P, Collier JM, Bate PJ, Thuy MN, Bernhardt J (2018) Very early versus delayed mobilisation after stroke. Cochrane Database Syst Rev 10:CD006187
Kasotakis G, Schmidt U, Perry D, Grosse-Sundrup M, Benjamin J, Ryan C, Tully S, Hirschberg R, Waak K, Velmahos G, Bittner EA, Zafonte R, Cobb JP, Eikermann M (2012) The surgical intensive care unit optimal mobility score predicts mortality and length of stay. Crit Care Med 40:1122–1128
Schaller SJ, Stauble CG, Suemasa M, Heim M, Duarte IM, Mensch O, Bogdanski R, Lewald H, Eikermann M, Blobner M (2016) The German validation study of the surgical intensive care unit optimal mobility score. J Crit Care 32:201–206
Piva S, Dora G, Minelli C, Michelini M, Turla F, Mazza S, D’Ottavi P, Moreno-Duarte I, Sottini C, Eikermann M, Latronico N (2015) The surgical optimal mobility score predicts mortality and length of stay in an Italian population of medical, surgical, and neurologic intensive care unit patients. J Crit Care 30:1251–1257
Meyer MJ, Stanislaus AB, Lee J, Waak K, Ryan C, Saxena R, Ball S, Schmidt U, Poon T, Piva S, Walz M, Talmor DS, Blobner M, Latronico N, Eikermann M (2013) Surgical intensive care unit optimal mobilisation score (SOMS) trial: a protocol for an international, multicentre, randomised controlled trial focused on goal-directed early mobilisation of surgical ICU patients. BMJ Open 3:e003262
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, Tesoro EP, Elswick RK (2002) The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 166:1338–1344
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, Hart RP, Dittus R (2001) Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 286:2703–2710
Gennarelli TA, Champion HR, Copes WS, Sacco WJ (1994) Comparison of mortality, morbidity, and severity of 59,713 head injured patients with 114,447 patients with extracranial injuries. J Trauma 37:962–968
Wagner AK, Fabio T, Zafonte RD, Goldberg G, Marion DW, Peitzman AB (2003) Physical medicine and rehabilitation consultation: relationships with acute functional outcome, length of stay, and discharge planning after traumatic brain injury. Am J Phys Med Rehabil 82:526–536
Fuest K, Schaller SJ (2018) Recent evidence on early mobilization in critical-Ill patients. Curr Opin Anaesthesiol 31:144–150
Li Z, Zhang X, Wang K, Wen J (2018) Effects of early mobilization after acute stroke: a meta-analysis of randomized control trials. J Stroke Cerebrovasc Dis 27:1326–1337
Titsworth WL, Hester J, Correia T, Reed R, Guin P, Archibald L, Layon AJ, Mocco J (2012) The effect of increased mobility on morbidity in the neurointensive care unit. J Neurosurg 116:1379–1388
Lee JJ, Waak K, Grosse-Sundrup M, Xue F, Lee J, Chipman D, Ryan C, Bittner EA, Schmidt U, Eikermann M (2012) Global muscle strength but not grip strength predicts mortality and length of stay in a general population in a surgical intensive care unit. Phys Ther 92:1546–1555
Garzon-Serrano J, Ryan C, Waak K, Hirschberg R, Tully S, Bittner EA, Chipman DW, Schmidt U, Kasotakis G, Benjamin J, Zafonte R, Eikermann M (2011) Early mobilization in critically ill patients: patients’ mobilization level depends on health care provider’s profession. PM&R 3:307–313
Waxman K, Sundine MJ, Young RF (1991) Is early prediction of outcome in severe head injury possible? Arch Surg 126:1237–1241 (discussion 1242)
Singh B, Murad MH, Prokop LJ, Erwin PJ, Wang Z, Mommer SK, Mascarenhas SS, Parsaik AK (2013) Meta-analysis of Glasgow Coma Scale and simplified motor score in predicting traumatic brain injury outcomes. Brain Inj 27:293–300
Jiang JY, Gao GY, Li WP, Yu MK, Zhu C (2002) Early indicators of prognosis in 846 cases of severe traumatic brain injury. J Neurotrauma 19:869–874
Kouloulas EJ, Papadeas AG, Michail X, Sakas DE, Boviatsis EJ (2013) Prognostic value of time-related Glasgow Coma Scale components in severe traumatic brain injury: a prospective evaluation with respect to 1-year survival and functional outcome. Int J Rehabil Res 36:260–267
Kevric J, Jelinek GA, Knott J, Weiland TJ (2011) Validation of the full outline of unresponsiveness (FOUR) scale for conscious state in the emergency department: comparison against the Glasgow Coma Scale. Emerg Med J 28:486–490
Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G (2014) The Glasgow Coma Scale at 40 years: standing the test of time. Lancet Neurol 13:844–854
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Zanni JM, Korupolu R, Fan E, Pradhan P, Janjua K, Palmer JB, Brower RG, Needham DM (2010) Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care 25:254–262
Clavet H, Doucette S, Trudel G (2015) Joint contractures in the intensive care unit: quality of life and function 3.3 years after hospital discharge. Disabil Rehabil 37:207–213
Clavet H, Hebert PC, Fergusson DA, Doucette S, Trudel G (2011) Joint contractures in the intensive care unit: association with resource utilization and ambulatory status at discharge. Disabil Rehabil 33:105–112
Koch SM, Fogarty S, Signorino C, Parmley L, Mehlhorn U (1996) Effect of passive range of motion on intracranial pressure in neurosurgical patients. J Crit Care 11:176–179
Moss M, Nordon-Craft A, Malone D, Van Pelt D, Frankel SK, Warner ML, Kriekels W, McNulty M, Fairclough DL, Schenkman M (2016) A randomized trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med 193:1101–1110
Wright SE, Thomas K, Watson G, Baker C, Bryant A, Chadwick TJ, Shen J, Wood R, Wilkinson J, Mansfield L, Stafford V, Wade C, Furneval J, Henderson A, Hugill K, Howard P, Roy A, Bonner S, Baudouin S (2018) Intensive versus standard physical rehabilitation therapy in the critically ill (EPICC): a multicentre, parallel-group, randomised controlled trial. Thorax 73:213–221
McWilliams D, Jones C, Atkins G, Hodson J, Whitehouse T, Veenith T, Reeves E, Cooper L, Snelson C (2018) Earlier and enhanced rehabilitation of mechanically ventilated patients in critical care: a feasibility randomised controlled trial. J Crit Care 44:407–412
Morris PE, Berry MJ, Files DC, Thompson JC, Hauser J, Flores L, Dhar S, Chmelo E, Lovato J, Case LD, Bakhru RN, Sarwal A, Parry SM, Campbell P, Mote A, Winkelman C, Hite RD, Nicklas B, Chatterjee A, Young MP (2016) Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: a randomized clinical trial. JAMA 315:2694–2702
Kim HJ, Lee Y, Sohng KY (2014) Effects of bilateral passive range of motion exercise on the function of upper extremities and activities of daily living in patients with acute stroke. J Phys Ther Sci 26:149–156
Relaix F, Zammit PS (2012) Satellite cells are essential for skeletal muscle regeneration: the cell on the edge returns centre stage. Development 139:2845–2856
Carel C, Loubinoux I, Boulanouar K, Manelfe C, Rascol O, Celsis P, Chollet F (2000) Neural substrate for the effects of passive training on sensorimotor cortical representation: a study with functional magnetic resonance imaging in healthy subjects. J Cereb Blood Flow Metab 20:478–484
Edwards DJ, Thickbroom GW, Byrnes ML, Ghosh S, Mastaglia FL (2002) Reduced corticomotor excitability with cyclic passive movement: a study using transcranial magnetic stimulation. Hum Mov Sci 21:533–540
Investigators TS, Hodgson C, Bellomo R, Berney S, Bailey M, Buhr H, Denehy L, Harrold M, Higgins A, Presneill J, Saxena M, Skinner E, Young P, Webb S (2015) Early mobilization and recovery in mechanically ventilated patients in the ICU: a bi-national, multi-centre, prospective cohort study. Crit Care 19:81
Funding
This study was funded by an unrestricted grant from Jeff and Judy Buzen to Matthias Eikermann. The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Study concept and design: MB, ME, SJS. Acquisition, analysis or interpretation of data: All authors. Drafting of the manuscript: SJS and ME. Revising the manuscript critically for important intellectual content: All authors. Statistical analysis: MB, HD, TH, SJS, FTS. Final approval of the version to be published: All authors. ME had full access to all the data in the study and is the guarantor for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflicts of interest
Stefan J. Schaller received research support from MSD (Haar, Germany) not related to this manuscript. He holds stocks from Rhoen-Klinikum, Bayer AG and Siemens AG and held stocks in the recent past from GE Healthcare, Merck and Co., Inc., and Fresenius SE. These holdings have not affected any decisions regarding his research or this study. Flora T. Scheffenbichler reports no disclosures. Nicole Mazwi reports no disclosures. Hao Deng reports no disclosures. Franziska Krebs reports no disclosures. Christian L. Seifert reports no disclosures. George Kasotakis reports no disclosures. Stephanie D Grabitz reports no disclosures. Nicola Latronico reports no disclosures. Somnath Bose reports no disclosures. Timothy Houle reports no disclosures. Manfred Blobner received research support from MSD (Haar, Germany) not related to this manuscript; he received honoraria for lectures from GE Healthcare (Helsinki, Finland) and Grünenthal (Aachen, Germany). Matthias Eikermann received research support from Merck not related to this manuscript; he also received research support for this study from Jeff and Judy Buzen.
Ethical approval
For this analysis was obtained by the institutional review board of Massachusetts General Hospital (protocol number 2016P002199) and registered at Clinical Trials (NCT03666338).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Stefan J. Schaller and Flora T. Scheffenbichler made equal contributions to the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schaller, S.J., Scheffenbichler, F.T., Bose, S. et al. Influence of the initial level of consciousness on early, goal-directed mobilization: a post hoc analysis. Intensive Care Med 45, 201–210 (2019). https://doi.org/10.1007/s00134-019-05528-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05528-x