Abstract
Rationale
Acute respiratory distress syndrome (ARDS) is frequently associated with hemodynamic instability which appears as the main factor associated with mortality. Shock is driven by pulmonary hypertension, deleterious effects of mechanical ventilation (MV) on right ventricular (RV) function, and associated-sepsis. Hemodynamic effects of ventilation are due to changes in pleural pressure (Ppl) and changes in transpulmonary pressure (TP). TP affects RV afterload, whereas changes in Ppl affect venous return. Tidal forces and positive end-expiratory pressure (PEEP) increase pulmonary vascular resistance (PVR) in direct proportion to their effects on mean airway pressure (mPaw). The acutely injured lung has a reduced capacity to accommodate flowing blood and increases of blood flow accentuate fluid filtration. The dynamics of vascular pressure may contribute to ventilator-induced injury (VILI). In order to optimize perfusion, improve gas exchange, and minimize VILI risk, monitoring hemodynamics is important.
Results
During passive ventilation pulse pressure variations are a predictor of fluid responsiveness when conditions to ensure its validity are observed, but may also reflect afterload effects of MV. Central venous pressure can be helpful to monitor the response of RV function to treatment. Echocardiography is suitable to visualize the RV and to detect acute cor pulmonale (ACP), which occurs in 20–25 % of cases. Inserting a pulmonary artery catheter may be useful to measure/calculate pulmonary artery pressure, pulmonary and systemic vascular resistance, and cardiac output. These last two indexes may be misleading, however, in cases of West zones 2 or 1 and tricuspid regurgitation associated with RV dilatation. Transpulmonary thermodilution may be useful to evaluate extravascular lung water and the pulmonary vascular permeability index. To ensure adequate intravascular volume is the first goal of hemodynamic support in patients with shock. The benefit and risk balance of fluid expansion has to be carefully evaluated since it may improve systemic perfusion but also may decrease ventilator-free days, increase pulmonary edema, and promote RV failure. ACP can be prevented or treated by applying RV protective MV (low driving pressure, limited hypercapnia, PEEP adapted to lung recruitability) and by prone positioning. In cases of shock that do not respond to intravascular fluid administration, norepinephrine infusion and vasodilators inhalation may improve RV function. Extracorporeal membrane oxygenation (ECMO) has the potential to be the cause of, as well as a remedy for, hemodynamic problems. Continuous thermodilution-based and pulse contour analysis-based cardiac output monitoring are not recommended in patients treated with ECMO, since the results are frequently inaccurate. Extracorporeal CO2 removal, which could have the capability to reduce hypercapnia/acidosis-induced ACP, cannot currently be recommended because of the lack of sufficient data.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) is frequently associated with hemodynamic instability. More than 60 % of patients experience hemodynamic failure [1] and around 65 % require infusion of catecholamines [2]. Circulatory failure consistently appears as the main factor associated with mortality, an association much higher than that relating to degree of hypoxemia [3]. In ARDS, shock is driven by three main factors: (1) pulmonary hypertension due to microthrombi, arterial remodeling and vasoconstriction from hypoxia, acidosis and/or inflammatory mediators, (2) deleterious effects of mechanical ventilation on right ventricular (RV) function, and (3) sepsis-induced tissue demands coupled to hemodynamic dysfunction. Patients may also develop shock because of co-existent left ventricular impairment by acute or chronic cardiac disease. Sepsis, the most common cause of shock in ARDS, may be associated with distributive hypovolemia, vasoplegia, and myocardial depression. Pulmonary hypertension-related to ARDS, sepsis-induced vascular dysfunction, and mechanical ventilation can all combine to produce RV failure, either by preload insufficiency or by excessive afterload.
Hemodynamic effects of mechanical ventilation
Hemodynamic effects of ventilation on the heart are mainly due to changes in pleural pressure (Ppl) and changes in transpulmonary pressure (TP). Changes in Ppl primarily affect inflow to the RV and outflow from the left ventricle (LV). Changes in TP primarily effect outflow from the RV and inflow to the LV. Change in Ppl is a key factor [4]. While the systemic circulation is surrounded by unvarying atmospheric pressure, vascular structures in the chest are surrounded by Ppl, which changes relative to atmospheric pressure throughout the respiratory cycle [5]. The decrease in Ppl during spontaneous inspiratory efforts, whether in a ventilated or non-ventilated patient, effectively lowers the pressure baseline of the heart relative to the rest of the body, and increases the gradient for the return of blood to the RV. The transient inspiratory increase in RV filling is passed to the LV over the next few beats. Release of inspiratory effort raises Ppl and produces a small expiratory rise in arterial pressure. When Ppl decreases and intracavitary cardiac pressures are lowered relative to atmosphere, LV afterload is increased because the heart needs more force to maintain normal arterial pressure [6]. Increased LV afterload and increased RV filling during repetitive large negative swings in Ppl can increase pulmonary blood volume considerably, even producing pulmonary edema when LV function is decreased and capillary permeability is increased.
Inflation with positive airway pressure does the opposite. Increasing Ppl by positive airway pressure decreases LV afterload but there is little benefit for cardiac output because venous return simultaneously decreases. The increase in Ppl transiently decreases venous return to the RV and eventually to the LV. Falling Ppl tends to decrease systemic arterial pressure during expiration. The pressure gradient from the upstream large venous reservoir to the heart normally is only 4–8 mmHg [7]. Thus, by increasing the right atrial back pressure, small changes in Ppl can exert relatively large effects on cardiac output. When positive end-expiratory pressure (PEEP) is present, the gradient for venous return is decreased throughout the ventilatory cycle. A reflex decrease in vascular capacitance or infusion of fluid then is necessary to maintain the venous pressure gradient and cardiac output [6]. As an approximate guide, in normal subjects, about 50 % of the change in alveolar pressure is transmitted to Ppl. Diseased lungs are stiffer so that less is transmitted. Because the normal right ventricle is highly compliant but has limited myocardial thickness and contractile power, it is relatively more sensitive to afterload than to variations of preload. However, whatever its cause, e.g., external pressure or impeded RV ejection, intracavitary right atrial pressure is a potent determinant of venous return.
TP, the difference between alveolar pressure and Ppl, determines lung volume in conjunction with lung compliance. When Ppl exceeds pulmonary venous pressure, microvascular collapse produces West zone 2 conditions [8]. When regional pleural and interstitial pressures exceed pulmonary arterial pressure, pulmonary blood flow is largely obstructed through that lung region (West zone 1) [8]. Under both conditions, alveolar pressure becomes the outflow pressure for the RV and can considerably increase the RV afterload [9]. This is important in septic, post-cardiac surgery, and ARDS patients with decreased RV function and low lung compliance.
The acutely injured lung has a reduced capacity to accommodate flowing blood due to inflammation, consolidation, compressive vascular collapse, and microthrombosis [10] while its gas exchange barrier leaks easily in response to transmural hydrostatic pressure [11]. Increased permeability characterizes pre-alveolar, post-alveolar, and capillary microvessels. Because a large fraction of total pulmonary vascular resistance (PVR) dissipates across the microvasculature, increases of blood flow during ARDS accentuate fluid filtration. Moreover, depleted capillary reserve heightens both mean vascular pressure and its response to variations of cardiac output. During controlled ventilation, tidal forces and PEEP increase PVR and Ppl in direct proportion to their effects upon mean alveolar pressure, which is clinically approximated as mean airway pressure (mPaw). PEEP is a prominent but not sole determinant of mPaw, which is also increased by the longer duty cycles and/or higher tidal driving pressures that characterize greater minute ventilation [12]. Raising mPaw not only increases average lung size but also pushes the chest wall outward by incrementing Ppl. Higher mPaw simultaneously distends lung units already open and encourages microvascular closure, even as it increases lung unit number by recruitment. In ARDS patients with highly recruitable lung units, maintaining a relatively open lung while limiting overdistention improves vascular resistance. Yet, at high levels of mPaw the net result is to encourage West zone 2 conditions, thereby raising effective vascular resistance within the aerated compartment, redirecting blood flow toward poorly ventilated units, increasing dead space, and afterloading the RV [13]. Occasionally, elevated right-sided pressures increase shunt through a patent foramen ovale and in severe ARDS overdistend the afterload-sensitive RV. Such overdistention functionally stiffens the left ventricle, which becomes interdependent of its right-sided counterpart via their shared septum, circumferential muscle fibers, and pericardial space [14]. If cardiac output remains unchanged, reduced left ventricular compliance mandates higher left atrial and pulmonary venous pressures, which in turn increase the tendency for edema to form. The increased right atrial pressure that results from higher Ppl and RV afterload also imposes back pressure on venous return that limits effectiveness of fluid loading and may reduce cardiac output unless compensated by increased upstream filling and vascular tone. Although abnormally high at rest, Ppl in ARDS rises relatively little as mPaw increases [15], whereas PVR escalates progressively. Resistance to systemic venous return can also rise as the vena cava is compressed at the thoracic inlet during lung expansion [16], but this effect is usually minor. Conversely, selective increases of abdominal pressure tend to translocate blood volume into the thorax and therefore to increase edema formation [17].
Vascular considerations in ventilator-induced lung injury
Ventilator-induced lung injury (VILI) arises from static and dynamic forces that affect the airspaces and epithelium [18]. However, the alveolus is a fragile membrane separating gas and blood so that once the ventilating forces are sufficiently high, vascular pressures and flows might strongly influence the severity of VILI [19]. Pulmonary edema depletes surfactant and promotes stress-focusing interfaces between closed and open lung units [20]. Experimentally, raising precapillary vascular pressure intensifies VILI, as does lowering postcapillary pressure if precapillary pressure is held constant [21]. The reason for the latter remains unclear, but one attractive hypothesis is that promoting West zone 2 conditions produces microvascular waterfalls (pressure gradients) that impose poorly tolerated shear stress and/or dissipate excessive energy across the vascular endothelium [19]. Directing the globally increased cardiac output of ARDS through fewer available vascular channels also boosts luminal velocity of blood flow. Experimental observations demonstrate that for a given combination of tidal airway pressures and breath frequency, reducing vascular flow and flow velocity downgrades capillary stress injury and VILI [22]. Conversely, without changing the magnitudes or profiles of airway and vascular pressures, reducing the frequency of lung stretch improves tissue tolerance [23]. As with the airspaces, the dynamics of vascular pressure may contribute to injury. Confirmatory clinical studies targeted specifically at defining the vascular contribution to VILI are both difficult and currently lacking. Yet, taken together, available experimental and anecdotal [24] observations suggest the value of reducing ventilatory and oxygen demands to avoid adverse two-way interactions between ventilation and perfusion.
Hemodynamic monitoring
For optimizing perfusion, improving gas exchange, and minimizing VILI risk, monitoring hemodynamics is of utmost importance in patients with ARDS. Insertion of an arterial catheter allows real-time monitoring of blood pressure and of pulse pressure variation (PPV) (Fig. 1). When appropriately observed and interpreted, PPV is a good predictor of fluid responsiveness [25, 26]. By indicating that stroke volume markedly changes during swings of positive pressure, high values of PPV suggest that the patient is fluid responsive. However, PPV is not valuable in cases of spontaneous breathing activity, low tidal volume, and low lung compliance—all conditions frequently encountered in ARDS. Nevertheless, if PPV is high (>12 to 13 %) while tidal volume or lung compliance is low, it is likely that the patient is preload responsive. In such cases, cardiac output should increase with fluid administration [25] but decrease with increments of PEEP [27]. In some cases of severe RV failure, a high PPV could be a sign of RV afterload dependence rather than of fluid responsiveness. This should prompt the clinician to assess RV function with echocardiography and/or to follow the changes in PPV during passive leg raising (PLR). A decrease in PPV during PLR suggests fluid responsiveness, whereas no change could indicate the presence of RV afterload dependence.
A central venous catheter is mandatory in most cases of ARDS when vasoactive drugs are required and allows measurements of both central venous pressure (CVP) and central venous oxygen saturation (ScvO2). Although CVP is a poor predictor of preload responsiveness, it is helpful to monitor the response of RV function to treatment. Measuring the esophageal pressure, a surrogate for Ppl, allows estimation of right atrial transmural pressure (right atrial pressure minus Ppl), facilitating assessment of how tidal ventilation affects hemodynamics. Unfortunately, routinely measuring esophageal pressure currently remains a challenge.
Echocardiography should be performed early in the course of management to quickly obtain information on ventricular dimensions and function, to assess changes in cardiac output in response to therapy, to observe vena caval dimensions during the tidal cycle, and to assess preload adequacy by responsiveness to tests such as PLR. Transthoracic echocardiography (TTE) is noninvasive and gives reliable information in most cases. However, when TTE is limited by poor echogenicity, transesophageal echocardiography (TEE) may prove helpful. TEE more accurately detects acute cor pulmonale (ACP) than TTE [28]. During ARDS, assessing RV size is a key objective which may be easily attained by comparing the RV end-diastolic area (RVEDA) with the LV end-diastolic area (LVEDA) [29]. An RVEDA/LVEDA ratio between 0.6 and 1 indicates moderate RV dilatation while an RVEDA/LVEDA ratio >1 indicates severe RV dilatation. ACP has been defined as the combination of an RVEDA/LVEDA ratio >0.6 and the presence of a paradoxical septal motion during end-systole [29]. The echocardiographic examination should be completed by determination of LV ejection fraction, LV end-diastolic area, cardiac output, and markers of LV filling pressures.
In patients with severe ARDS or sepsis-associated disorders that do not respond to the initial therapy, advanced hemodynamic monitoring should be considered [30]. In these cases, inserting a pulmonary artery catheter (PAC) may be useful [30]. It allows measurement of pulmonary artery pressure (PAP) and pulmonary artery occlusion pressure (PAOP) and calculation of pulmonary and systemic vascular resistance. During ventilation with high PEEP, calculating the transmural value of PAOP [31] allows estimation of true LV filling pressure. The PAC also allows monitoring of cardiac output and mixed venous oxygen saturation (SvO2), two indexes that serve to assess the response to key therapies (PEEP, fluids, drugs). In cases of tricuspid regurgitation associated with RV dilatation, measurements of cardiac output can be erroneous. In the context of ARDS, West zones 1 and 2 can be abnormally extended as a result of a high TP, especially in cases of hypovolemia. Thus, calculated PVR may underestimate the true resistance of the pulmonary vascular tree. In such a context, the transpulmonary pressure gradient (mean PAP − PAOP) remains valuable in assessing the degree of pulmonary vascular abnormality [32].
Transpulmonary thermodilution systems can also be used in complex situations [30]. Apart from cardiac output, the most useful transpulmonary thermodilution-derived variables are extravascular lung water and pulmonary vascular permeability index, particularly in ARDS [33]. Measurement of these indicators may help assess the risk of fluid overload in ARDS. Additionally, transpulmonary thermodilution serves to calibrate the pulse contour method that allows monitoring cardiac output in real time from a femoral artery pressure curve. Preload responsiveness indices such as PPV and stroke volume variation (SVV) are also provided by pulse contour analysis. However, this technique has been reported as inaccurate in ARDS patients with a patent foramen ovale.
Multiple invasive (e.g., radial artery catheter) and noninvasive (e.g., volume clamp and applanation tonometry) uncalibrated pulse contour methods have been developed in the last 10 years. However, such tools cannot be recommended for ARDS patients as they can only provide continuous cardiac output, PPV, and SVV values, and validity has been seriously questioned in the presence of sepsis and/or vasopressor use.
Key steps in hemodynamic management (Tables 1 and 2)
In ventilated ARDS patients, the first step is to determine if tissue perfusion is adequate. In order to ensure adequacy of intravascular volume or preload there are three methods: ultrasound evaluation of inferior vena cava dimension and filling dynamics, pulse pressure variation observations, and/or central venous pressure monitoring in response to intervention. Urine output and metabolic acidosis are also standard clinical indices of tissue perfusion. Volume resuscitation may include isotonic fluids and also red blood cells, especially if the hemoglobin is less than approximately 8 g/dL. Albumin may be considered, especially in cases of sepsis-related ARDS or severely decreased serum albumin. However, fluids should be administered cautiously since they may decrease oxygenation by increasing the quantity of pulmonary edema, and may precipitate cor pulmonale as a result of the RV-specific properties in this situation of increased afterload [34]. Conversely, restriction of fluids may promote West zone 2 conditions. The risks and the benefits have to be carefully evaluated and use of just one approach to correct any parameters of fluid responsiveness is not appropriate since physicians have to take into account many other parameters such as tissue perfusion, oxygenation, and central venous pressure. Several experimental studies of RV failure related to obstruction of pulmonary circulation have reported the deleterious effect of excess fluids on cardiac output, blood pressure, and RV function, compared to norepinephrine [35]. Moreover, RV failure is the main factor limiting efficacy of fluid administration in restoring perfusion [36].
Finally, the Fluid And Catheter Treatment Trial (FACTT) from the ARDS Network, although carried out in patients who did not require vasopressor support, provided persuasive evidence that most ARDS benefits from a fluid conservative protocol when shock (vasopressor dependence) is resolved. The fluid conservative protocol was associated with a significant increase in ventilator-free days, although it did not demonstrate a reduction in mortality [37]. Because the fluid conservative protocol was complex, the ARDS Network subsequently designed a simplified version of fluid management for patients with ARDS who were not in shock. This simplified version of fluid management, based on central venous pressure and urine output, was entitled ‘FACTT-lite’, as shown in Table 1. A recent analysis of the FACTT-lite protocol versus the original FACTT protocol indicated that the FACTT-lite and FACTT conservative groups had similar ventilator-free days. Interestingly, prevalence of new-onset shock was lower in the FACTT-lite group than in the FACTT conservative group, while the prevalence of acute kidney injury was similar. This secondary analysis suggests that the FACTT-lite protocol had similar clinical outcomes compared to the more detailed original FACTT conservative protocol [38].
Once adequacy of intravascular volume is ensured, the second step is to look for ACP, which is reported in around 20–25 % of ARDS patients [1]. In these, the key hemodynamic priority is to support the right ventricle adequately. As emphasized above, once replete, further fluid expansion is usually useless and even deleterious. Norepinephrine has been reported to significantly improve RV function by restoring mean arterial pressure and RV blood supply, especially when deteriorated by high RV wall stress [39, 40]. A study performed in ARDS has also proposed to administer levosimendan, a calcium sensitizer, that could be especially indicated in this situation by its ability to restore the coupling between the RV (inotropic effect) and the pulmonary circulation (vasodilatory effect) [41]. However, more data are needed before recommending such an approach, which may simultaneously promote significant hypotension.
Inhaled selective pulmonary vasodilators have been proposed for patients with refractory hypoxemia. They may also improve RV function, but they have not yet been rigorously tested for this specific indication in ARDS. The two commonly used agents, inhaled nitric oxide (5–10 ppm) and inhaled prostacyclin (20–30 ng/kg/min), appear to have comparable efficacy in improving oxygenation, though there is no evidence for improved clinical outcomes [42]. Both agents reduce pulmonary vascular resistance and improve ventilation/perfusion matching without inducing systemic hypotension. Their benefits often diminish, however, after the initial period of use. Systemic vasodilators have not been shown to be beneficial in ARDS. Although some studies have suggested the possibility that anticoagulation therapy might help in ARDS, there have been no clinical trials to demonstrate improved clinical outcomes with anticoagulant therapy. In fact, a phase 2 clinical trial of activated protein C for the treatment of ARDS did not show benefit [43].
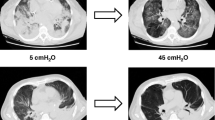
To apply a respiratory strategy aimed at unloading the right ventricle is a cornerstone of hemodynamic management. RV overload in ARDS relates to lung derecruitment [44], lung overdistension [45], and also hypoxic and hypercapnic pulmonary vasoconstriction [46–48], all of which are impacted strongly by ventilatory modalities and settings. Because severe RV failure has been reported to be independently associated with poor prognosis [1], the respiratory strategy should aim to promote cardiac function and limit the potentially adverse impact of ventilation. Recently, four risk factors promoting RV failure have been reported, i.e., pneumonia as a cause of ARDS, a PaO2/FiO2 ratio <150 mmHg, a driving pressure ≥18 cmH2O, and a PaCO2 ≥48 mmHg [1]. When all factors are present, the risk of RV failure exceeds 60 %, whereas when no factor is present the risk is less than 10 %. All but the first of these can be modulated by adjusting the respiratory settings. Risk factor avoidance helps optimize hemodynamics, reverse pre-existing RV failure, and improve prognosis [49]. Ideally, PEEP should be optimized so as to benefit alveolar patency while avoiding deleterious (or even accomplishing beneficial) effects on the pulmonary circulation, thereby unloading the right ventricle. On the one hand, sufficient PEEP is required to avoid lung derecruitment and the contribution to RV afterload induced by lung collapse [44]. On the other hand, PEEP-induced lung overdistension sequentially impairs the pulmonary circulation, RV function, and hemodynamics [50–52]. This was recently illustrated using strain and strain rate echocardiography in normal lungs in pigs. In that study, high PEEP (above a value of 15 cmH2O) applied to normal lungs promoted overdistension and dramatically worsened systemic hemodynamics owing to RV systolic dysfunction [53]. Respiratory modalities that promote high mPaw and lung overdistension should be avoided. These may include high frequency oscillation about a high PEEP baseline, an approach which has been reported to worsen prognosis, presumably as a result of the hemodynamic impairment [54] and RV failure [55]. From a hemodynamic point of view, vigorous spontaneous breathing also has to be avoided. Forceful inspiratory efforts augment transvascular pressure and the tendency for lung edema to form [56]. Interstitial pressure that surrounds the alveoli and the leaky vessels that perfuse them is traditionally equated with pressure at the pleural surface but may be regionally higher or lower within the mechanically heterogeneous injured lung [57]. Moreover, because the inflating force (including that needed to overcome airflow resistance) originates at the pleura, transmicrovascular pressures are especially high during forceful spontaneous efforts [58] (Fig. 2). Finally, asynchronous ventilation and pendelluft [59, 60] could potentially impair the pulmonary circulation and RV function. Prone positioning (PP), by virtue of its ability to improve the uniformity of ventilation [61] and to attenuate and redistribute VILI [62], may unload the right ventricle. In two studies, PP actually restored RV function in patients with a previously overloaded right ventricle [63, 64]. Such observations tally well with the capacity of PP to improve prognosis [65], which seems unexplained by amelioration of gas exchange [66]. In studies reporting such PP-induced improvement in RV function, the indication for proning was exclusively the severity of lung injury based on the PaO2/FiO2 ratio. It remains to be seen whether a strategy of turning patients prone on the basis of the existence of RV overloading is effective and could improve prognosis.
Hypothetical effect of the pleural pressure during controlled and spontaneous breathing on transvascular pressure. In this illustration the lung distends to the same 30 cmH2O transpulmonary pressure by three combinations of alveolar and pleural pressure. If the luminal microvascular pressure is equivalent to 15 cmH2O, and interstitial pressure is assumed equal to pleural pressure, then the fluid-filtering transvascular pressure (PTV) in this extreme example would theoretically range from 5 to 25 cmH2O
Place for extracorporeal circulation and its consequences
ECMO has potential to be the cause of, as well as a remedy for, hemodynamic problems in ARDS. Venovenous extracorporeal membrane oxygenation (vvECMO) is used with increased frequency to avoid life-threatening refractory hypoxemia, and to reduce harm from ventilation in patients with severe ARDS [67]. By its ability to increase blood oxygenation, vvECMO may also help to limit pulmonary artery hypertension and then to unload the right ventricle [68]. Venoarterial ECMO (vaECMO) not only avoids hypoxemia but also provides hemodynamic stability in cases of cardiogenic shock provoked by various causes and refractory to medical treatment [69]. Venovenous extracorporeal CO2 removal (ECCO2R) is an approach that allows lower extracorporeal blood and sweep gas flows than vvECMO and vaECMO, and is primarily used to avoid unacceptable hypercapnia, acidosis, and/or injurious ventilator settings—conditions that impact the heart as well as lungs [67]. The following choices have recently been recommended [70, 71] (Fig. 3): vvECMO can be indicated in patients with severe ARDS within 7 days after onset and with persistent life-threatening hypoxemia unresponsive to optimized supportive therapy; vaECMO can be considered when ARDS is combined with severe cardiogenic shock with a very low cardiac output and reduced LV ejection fraction (confirmed by echocardiography and need for significant inotropic support and/or norepinephrine at dosages >0.5 µg/kg/min). Currently, ECCO2R cannot be recommended for ARDS without reservation owing to lack of sufficient data.
Proposed algorithm regarding indications for ECMO/ECCO2R and hemodynamic management during ECMO/ECCO2R in patients with severe ARDS at risk of hemodynamic instability. Readers have to be cautioned that this algorithm was not previously validated. V T tidal volume, P plat inspiratory plateau pressure, MAP mean arterial pressure, NOR norepinephrine, SvO 2 central venous oxygen saturation. Asterisk as re-emphasized in the text, this is currently not evidence-based data
All ECMO techniques carry hemodynamic risks and their use requires expertise, experience, careful adherence to routine, and an interdisciplinary approach [70]. Recommendations for hemodynamic monitoring and therapy in patients under ECMO with hemodynamic instability are still in development. Hemodynamic monitoring includes continuous monitoring of arterial blood pressure, repeated echocardiography [72], and continuous recording of extracorporeal blood flow, especially in the case of vaECMO. Of note, continuous thermodilution-based and pulse contour analysis-based cardiac output monitoring are not recommended in patients under ECMO, since the first may lead to erroneous results caused by indicator loss into the extracorporeal circuit [73] and the second may underestimate cardiac output [74]. Accurate recording of the fluid intake and output is important because a positive fluid balance has been identified as an independent predictor of outcome of patients receiving ECMO [75]. In general, hemodynamic therapy requires a careful approach regarding volume replacement and vasopressor use. Hypovolemia may induce venous collapse during extracorporeal extraction of blood, causing cannula ‘suctioning’ and ‘chatter’ that result in flow reduction and hemolysis [76]. On the other hand, volume overload can aggravate lung edema, which in turn worsens outcome [75]. Therefore, the hemodynamic support is optimized by a balanced strategy of fluid infusions (small boluses, e.g., 250 mL) and vasopressors under repeated monitoring (MAP, echocardiography, central venous oxygen saturation, and lactate).
Hemodynamic problems during ECMO and specific potential solutions are as follows: systemic vasodilation—start a vasoconstrictor (e.g., norepinephrine); left ventricular dysfunction—consider starting inotropes (e.g., epinephrine or levosimendan; note lack of an adequate evidence base for the latter recommendation in this specific setting); right ventricular dysfunction—optimize (reduce) preload, start pulmonary vasodilators (e.g., prostacyclin) or catecholamines (e.g., epinephrine, norepinephrine). Early evaluation and adequate management have the potential to improve outcome [77], and vaECMO could be considered a potentially useful intervention for severe cases of ACP-induced circulatory failure/shock syndrome (Fig. 3). ECCO2R has the capability to reduce hypercapnia/acidosis-induced ACP as shown in an experimental setting recently [78] and also may enable low or ‘supra-low’ tidal volume ventilation which in turn may attenuate the harmful effects of high inspiratory pressure and lung overinflation on the right ventricle. It is reasonable to consider ECCO2R as an advanced therapeutic option in ARDS patients who are at risk for decompensated shock due to severe RV failure, even though there is not yet convincing evidence in the literature; further studies are clearly required. In bypassing the failing right heart, vaECMO has potential to ‘buy time’ as a temporary but complete replacement for both lung and circulatory functions.
Conclusions
Both the underlying lung pathology and mechanical ventilation result in hemodynamic challenges for patients with ARDS. Acute lung injury restricts the functioning vascular bed, increases lung vascular permeability, and promotes vascular narrowing in response to inflammation, hypoxemia, and acidosis. Hemodynamic instability may arise from high airway pressures if they adversely alter the gradient for venous return, distend the ‘baby lung’, and raise the ejection impedance of the afterload-sensitive right ventricle. Higher lung stress and vascular flow, such as during vigorous spontaneous breathing, encourage the development of VILI. Although adequate diastolic filling is essential to maintain forward output, RV overdistension not only impedes venous return and reduces the functional compliance of the interdependent left ventricle but may also compromise its own perfusion adequacy. In passively ventilated patients in shock, monitoring signals linked to the tidal cycle and ventricular loading help predict preload and afterload dependence of the right ventricle. Interventions directed toward improving compensation of the compromised RV include reduction of unnecessary systemic oxygen demand, optimized fluid resuscitation, appropriate lung recruitment, prone positioning, avoidance of acidosis, maintenance of oxygenation, and well-selected pharmacologic agents. In severe cases, varied options for extracorporeal gas exchange can be deployed to reduce ventilatory and cardiac workloads while compensating for impaired oxygenation. Once shock is resolved, a fluid conservative protocol may reduce the duration of positive pressure ventilation. Successfully managing the complex hemodynamics of the ventilated patient with ARDS is key to patient survival. Doing so in this setting requires guidance from a deep understanding of the underlying principles of cardiopulmonary physiology, rendering it difficult to enumerate definitive, specific, and universally applicable guidelines.
References
Mekontso-Dessap A, Boissier F, Charron C, Bégot E, Repessé X, Legras A, Brun-Buisson C, Vignon P, Vieillard-Baron A (2015) Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med. doi:10.1007/s00134-015-4141-2
McAuley DF, Laffey JG, O’Kane CM, Perkins GD, Mullan B, Trinder TJ, Johnston P, Hopkins PA, Johnston AJ, McDowell C, McNally C, HARP-2 Investigators, Irish Critical Care Trials Group (2014) Simvastatin in the acute respiratory distress syndrome. N Engl J Med 371:1695–1703
Vieillard-Baron A, Girou E, Valente E, Brun-Buisson C, Jardin F, Lemaire F, Brochard L (2000) Predictors of mortality in acute respiratory distress syndrome. Focus on the role of right heart catheterization. Am J Respir Crit Care Med 161:1597–1601
Magder S, Guerard B (2012) Heart-lung interactions and pulmonary buffering: lessons from a computational modeling study. Respir Physiol Neurobiol 182:60–70
Marini JJ, Culver BH, Butler J (1981) Mechanical effect of lung distention with positive pressure on cardiac function. Am Rev Respir Dis 124:382–386
Magder SA, Lichtenstein S, Adelman AG (1983) Effects of negative pleural pressure on left ventricular hemodynamics. Am J Cardiol 52:588–593
Nanas S, Magder S (1992) Adaptations of the peripheral circulation to PEEP. Am Rev Respir Dis 146:688–693
Permutt S, Bromberger-Barnea B, Bane HN (1962) Alveolar pressure, pulmonary venous pressure, and the vascular waterfall. Med Thorac 19:239–260
Jardin F, Vieillard-Baron A (2003) Right ventricular function and positive pressure ventilation in clinical practice: from hemodynamic subsets to respirator settings. Intensive Care Med 29:1426–1434
Tomashefski JF Jr, Davies P, Boggis C, Greene R, Zapol WM, Reid LM (1983) The pulmonary vascular lesions of the adult respiratory distress syndrome. Am J Pathol 112:112–126
Brigham KL, Woolverton WC, Blake LH, Staub NC (1974) Increased sheep lung vascular permeability caused by pseudomonas bacteremia. J Clin Invest 54:792–804
Marini JJ, Ravenscraft SA (1992) Mean airway pressure: physiologic determinants and clinical importance—Part 1: physiologic determinants and measurements. Crit Care Med 20:1461–1472
Petersson J, Ax M, Frey J, Sánchez-Crespo A, Lindahl SG, Mure M (2010) Positive end-expiratory pressure redistributes regional blood flow and ventilation differently in supine and prone humans. Anesthesiology 113:1361–1369
Frennaux M, Williams L (2007) Ventricular-arterial and ventricular-ventricular interaction and their relevance to diastolic filling. Prog Cardiovasc Dis 49:252–262
Loring SH, O’Donnell CR, Behazin N, Malhotra A, Sarge T, Ritz R, Novack V, Talmor D (2010) Esophageal pressures in acute lung injury: do they represent artifact or useful information about transpulmonary pressure, chest wall mechanics, and lung stress? J Appl Physiol 108:515–522
Fessler HE, Brower RG, Shapiro EP, Permutt S (1993) Effects of positive end-expiratory pressure and body position on pressure in the thoracic great veins. Am Rev Respir Dis 148:1657–1664
Quintel M, Pelosi P, Caironi P, Meinhardt JP, Luecke T, Herrmann P, Taccone P, Rylander C, Valenza F, Carlesso E, Gattinoni L (2004) An increase of abdominal pressure increases pulmonary edema in oleic acid-induced lung injury. Am J Respir Crit Care Med 169:534–541
Protti A, Andreis DT, Monti M, Santini A, Sparacino CC, Langer T, Votta E, Gatti S, Lombardi L, Leopardi O, Masson S, Cressoni M, Gattinoni L (2013) Lung stress and strain during mechanical ventilation: any difference between statics and dynamics? Crit Care Med 41:1046–1055
Marini JJ, Hotchkiss JR, Broccard AF (2003) Bench to bedside review: microvascular and airspace linkage in ventilator-induced lung injury. Crit Care 7:435–444
Albert RK (2012) The role of ventilation-induced surfactant dysfunction and atelectasis in causing acute respiratory distress syndrome. Am J Respir Crit Care Med 185:702–708
Broccard A, Vannay C, Feihl F, Schaller MD (2002) Impact of low pulmonary vascular pressure on ventilator-induced lung injury. Crit Care Med 30:2183–2190
López-Aguilar J, Piacentini E, Villagrá A, Murias G, Pascotto S, Saenz-Valiente A, Fernández-Segoviano P, Hotchkiss JR, Blanch L (2006) Contributions of vascular flow and pulmonary capillary pressure to ventilator-induced lung injury. Crit Care Med 34:1106–1112
Hotchkiss JR, Blanch LL, Murias G, Adams AB, Olson D, Wangensteen OD, Leo PH, Marini JJ (2000) Effects of decreased respiratory frequency on ventilator induced lung injury. Am J Respir Crit Care Med 161:463–468
Hotchkiss JR, Simonson DA, Marek DJ, Marini JJ, Dries DJ (2002) Pulmonary microvascular fracture in a patient with acute respiratory distress syndrome. Crit Care Med 30:2368–2370
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Yang X, Du B (2014) Does pulse pressure variation predict fluid responsiveness in critically ill patients? A systematic review and meta-analysis. Crit Care 18:650
Michard F, Chemla D, Richard C, Wysocki M, Pinsky MR, Lecarpentier Y, Teboul JL (1999) Clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP. Am J Respir Crit Care Med 159:935–939
Lhéritier G, Legras A, Caille A, Lherm T, Mathonnet A, Frat JP, Courte A, Martin-Lefèvre L, Gouëllo JP, Amiel JB, Garot D, Vignon P (2013) Prevalence and prognostic value of acute cor pulmonale and patent foramen ovale in ventilated patients with early acute respiratory distress syndrome: a multicenter study. Intensive Care Med 39:1734–1742
Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F (2002) Echo-Doppler demonstration of acute cor pulmonale at the bedside in the medical intensive care unit. Am J Respir Crit Care Med 166:1310–1319
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A (2014) Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med 40:1795–1815
Teboul JL, Pinsky MR, Mercat A, Anguel N, Bernardin G, Achard JM, Boulain T, Richard C (2000) Estimating cardiac filling pressure in mechanically ventilated patients with hyperinflation. Crit Care Med 28:3631–3636
Bull TM, Clark B, McFann K, Moss M, National Institutes of Health/National Heart, Lung, and Blood Institute ARDS Network (2010) Pulmonary vascular dysfunction is associated with poor outcomes in patients with acute lung injury. Am J Respir Crit Care Med 182:1123–1128
Jozwiak M, Silva S, Persichini R, Anguel N, Osman D, Richard C, Teboul JL, Monnet X (2013) Extravascular lung water is an independent prognostic factor in patients with acute respiratory distress syndrome. Crit Care Med 41:472–480
Pinsky MR (2014) My paper 20 years later: effect of positive end-expiratory pressure on right ventricular function in humans. Intensive Care Med 40:935–941
Ghignone M, Girling L, Prewitt RM (1984) Volume expansion versus norepinephrine in treatment of a low cardiac output complicating an acute increase in right ventricular afterload in dogs. Anesthesiology 60:132–135
Schneider AJ, Teule GJ, Groeneveld AB, Nauta J, Heidendal GA, Thijs LJ (1988) Biventricular performance during volume loading in patients with early septic shock, with emphasis on the right ventricle: a combined hemodynamic and radionuclide study. Am Heart J 116:103–112
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Grissom CK, Hirshberg EL, Dickerson JB, Brown SM, Lanspa MJ, Liu KD, Schoenfeld D, Tidswell M, Hite RD, Rock P, Miller RR 3rd, Morris AH (2015) Fluid management with a simplified conservative protocol for the acute respiratory distress syndrome. Crit Care Med 43:288–295
Guyton AC, Lindsey AW, Gilluly JJ (1954) The limits of right ventricular compensation following acute increase in pulmonary circulation resistance. Circ Res 2:326–332
Vlahakes GJ, Turley K, Hoffman JI (1981) The pathophysiology of failure in acute right ventricular hypertension: hemodynamic and biochemical correlations. Circulation 63:87–95
Morelli A, Teboul JL, Maggiore SM, Vieillard-Baron A, Rocco M, Conti G, De Gaetano A, Picchini U, Orecchioni A, Carbone I, Tritapepe L, Pietropaoli P, Westphal M (2006) Effects of levosimendan on right ventricular afterload in patients with acute respiratory distress syndrome: a pilot study. Crit Care Med 34:2287–2293
Dzierba AL, Abel EE, Buckley MS, Lat I (2014) A review of inhaled nitric oxide and aerosolized epoprostenol in acute lung injury or the acute respiratory distress syndrome. Pharmacotherapy 34:279–290
Liu KD, Levitt J, Zhuo H, Kallet RH, Brady S, Steingrub J, Tidswell M, Siegel MD, Soto G, Peterson MW, Chesnutt MS, Phillips C, Weinacker A, Thompson BT, Eisner MD, Matthay MA (2008) Randomized clinical trial of activated protein C for the treatment of acute lung injury. Am J Respir Crit Care Med 178:618–623
Duggan M, McCaul CL, McNamara PJ, Engelberts D, Ackerley C, Kavanagh BP (2003) Atelectasis causes vascular leaks and lethal right ventricular failure in uninjured rat lungs. Am J Respir Crit Care Med 167:1633–1640
Mekontso Dessap A, Voiriot G, Zhou T, Marcos E, Dudek SM, Jacobson JR, Machado R, Adnot S, Brochard L, Maitre B, Garcia JG (2012) Conflicting physiological and genomic cardiopulmonary effects of recruitment maneuvers in murine acute lung injury. Am J Respir Cell Mol Biol 46:541–550
Naeje R, Brimioulle S (2001) Physiology in medicine: importance of hypoxic vasoconstriction in maintaining arterial oxygenation during acute respiratory failure. Crit Care 5:67–71
Rabinovitch M, Gamble W, Nadas AS, Miettinen OS, Reid L (1979) Rat pulmonary circulation after chronic hypoxia: hemodynamic and structural features. Am J Physiol 236:H818–H827
Mekontso Dessap A, Charron C, Devaquet J, Aboab J, Jardin F, Brochard L, Vieillard-Baron A (2009) Impact of acute hypercapnia and augmented positive end-expiratory pressure on right ventricle function in severe acute respiratory distress syndrome. Intensive Care Med 35:1850–1858
Vieillard-Baron A, Price L, Matthay MA (2013) Acute cor pulmonale in ARDS. Intensive Care Med 39:1836–1838
West JB, Dollery CT, Naimark A (1964) Distribution of blood flow in isolated lung; relation to vascular and alveolar pressures. J Appl Physiol 19:713–724
Jardin F, Brun-Ney D, Cazaux P, Dubourg O, Hardy A, Bourdarias JP (1989) Relation between transpulmonary pressure and right ventricular isovolumetric pressure change during respiratory support. Catheter Cardiovasc Diagn 16:215–220
Vieillard-Baron A, Prin S, Augarde R, Desfonds P, Page B, Beauchet A, Jardin F (2002) Increasing respiratory rate to improve CO2 clearance during mechanical ventilation is not a panacea in acute respiratory failure. Crit Care Med 30:1407–1412
Orde SR, Behafar A, Stalboerger PG, Barros-Gomes S, Kane GC, Oh JK (2015) Effect of positive end-expiratory pressure on porcine right ventricle function assessed by speckle tracking echocardiography. BMC Anesthesiol 15:49
Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P, OSCILLATE Trial Investigators, Canadian Critical Care Trials Group et al (2013) High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med 368:795–805
Guervilly C, Forel JM, Hraiech S, Demory D, Allardet-Servent J, Adda M, Barreau-Baumstark K, Castanier M, Papazian L, Roch A (2012) Right ventricular function during high-frequency oscillatory ventilation in adults with acute respiratory distress syndrome. Crit Care Med 40:1539–1545
Dreyfuss D, Soler P, Basset G, Saumon G (1988) High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 137:1159–1164
Raj JU, Bland RD, Lai-Fook SJ (1986) Microvascular pressures measured by micropipettes in isolated edematous rabbit lungs. J Appl Physiol 60:539–545
Yoshida T, Uchiyama A, Matsuura N, Mashimo T, Fujino Y (2012) Spontaneous breathing during lung-protective ventilation in an experimental acute lung injury model: high transpulmonary pressure associated with strong spontaneous breathing effort may worsen lung injury. Crit Care Med 40:1578–1585
Vieillard-Baron A, Prin S, Schmitt JM, Augarde R, Page B, Beauchet A, Jardin F (2002) Pressure-volume curves in acute respiratory distress syndrome: clinical demonstration of the influence of expiratory flow limitation on the initial slope. Am J Respir Crit Care Med 165:1107–1112
Tabuchi A, Nickless HT, Kim M, Semple JW, Koch E, Brochard L, Slutsky AS, Pries AR, Kuebler WM (2015) Acute lung injury causes asynchronous alveolar ventilation which can be corrected by individual sighs. Am J Respir Crit Care Med 193:396–406
Vieillard-Baron A, Rabiller A, Chergui K, Peyrouset O, Page B, Beauchet A, Jardin F (2005) Prone position improves mechanics and alveolar ventilation in acute respiratory distress syndrome. Intensive Care Med 31:220–226
Broccard A, Shapiro RS, Schmitz LL, Adams AB, Nahum A, Marini JJ (2000) Prone positioning attenuates and redistributes ventilator-induced lung injury in dogs. Crit Care Med 28:295–303
Vieillard-Baron A, Charron C, Caille V, Belliard G, Page B, Jardin F (2007) Prone position unloads the right ventricle in severe ARDS. Chest 132:1440–1446
Joszwiak M, Teboul JL, Anguel N, Persichini R, Silva S, Chemla D, Richard C, Monnet X (2013) Beneficial hemodynamic effects of prone positioning in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 188:1428–1433
Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, PROSEVA Study Group et al (2013) Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 368:2159–2168
Albert RK, Keniston A, Baboi L, Ayzac L, Guérin C, Proseva Investigators (2014) Prone position-induced improvement in gas exchange does not predict improved survival in the acute respiratory distress syndrome. Am J Respir Crit Care Med 189:494–496
Del Sorbo L, Cypel M, Fan E (2014) Extracorporeal life support for adults with severe acute respiratory failure. Lancet Respir Med 2:154–164
Reis Miranda D, van Thiel R, Brodie D, Bakker J (2015) Right ventricular unloading after initiation of venovenous extracorporeal membrane oxygenation. Am J Respir Crit Care Med 191:346–348
Pellegrino V, Hockings LE, Davies A (2014) Veno-arterial extracorporeal membrane oxygenation for adult cardiovascular failure. Curr Opin Crit Care 20:484–492
Combes A, Brodie D, Bartlett R, Brochard L, Brower R, Conrad S, De Backer D, Fan E, Ferguson N, Fortenberry J, Fraser J, Gattinoni L, Lynch W, MacLaren G, Mercat A, Mueller T, Ogino M, Peek G, Pellegrino V, Pesenti A, Ranieri M, Slutsky A, Vuylsteke A, International ECMO Network (ECMONet) (2014) Position paper for the organization of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am J Respir Crit Care Med 190:488–496
Richard C, Argaud L, Blet A, Boulain T, Contentin L, Dechartres A, Dejode JM, Donetti L, Fartoukh M, Fletcher D, Kuteifan K, Lasocki S, Liet JM, Lukaszewicz AC, Mal H, Maury E, Osman D, Outin H, Richard JC, Schneider F, Tamion F (2014) Extracorporeal life support for patients with acute respiratory distress syndrome: report of a consensus conference. Ann Intensive Care 24(4):15
Lazzeri C, Cianchi G, Bonizzoli M, Batacchi S, Peris A, Gensini GF (2015) The potential role and limitations of echocardiography in acute respiratory distress syndrome. Ther Adv Respir Dis 10:136–148
Haller M, Zöllner C, Manert W, Briegel J, Kilger E, Polasek J, Hummel T, Forst H, Peter K (1995) Thermodilution cardiac output may be incorrect in patients on venovenous extracorporeal lung assist. Am J Respir Crit Care Med 152:1812–1817
Rauch H, Müller M, Fleischer F, Bauer H, Martin E, Böttiger BW (2002) Pulse contour analysis versus thermodilution in cardiac surgery patients. Acta Anaesthesiol Scand 46:424–429
Schmidt M, Bailey M, Kelly J, Hodgson C, Cooper DJ, Scheinkestel C, Pellegrino V, Bellomo R, Pilcher D (2014) Impact of fluid balance on outcome of adult patients treated with extracorporeal membrane oxygenation. Intensive Care Med 40:1256–1266
Choi SW, Nam KW (2008) Venous pressure regulation during pulsatile extracorporeal life support. Artif Organs 32:822–827
Repessé X, Charron C, Vieillard-Baron A (2015) Acute cor pulmonale in ARDS: rationale for protecting the right ventricle. Chest 147:259–265
Morimont P, Guiot J, Desaive T, Tchana-Sato V, Janssen N, Cagnina A, Hella D, Blaffart F, Defraigne JO, Lambermont B (2015) Veno-venous extracorporeal CO2 removal improves pulmonary hemodynamics in a porcine ARDS model. Acta Anaesthesiol Scand 59:448–456
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, Ranieri M, Rubenfeld G, Thompson BT, Wrigge H, Slutsky AS, Pesenti A, Lung Safe Investigators, ESICM Trials Group (2016) Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care unit in 50 countries. JAMA 315:788–800
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
AVieillard-Baron declares no conflict of interest. M. Matthay declares no conflict of interest. J. L. Teboul is a member of the medical advisory board of Pulsion Medical systems (Germany) and gave lectures for Edwards Lifesciences (USA) and Masimo (USA). T. Bein is member of the medical advisory board of Novalung, Heilbron, Germany and he received honoraria. S. Magder declares no conflict of interest. J. J. Marini declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Vieillard-Baron, A., Matthay, M., Teboul, J.L. et al. Experts’ opinion on management of hemodynamics in ARDS patients: focus on the effects of mechanical ventilation. Intensive Care Med 42, 739–749 (2016). https://doi.org/10.1007/s00134-016-4326-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4326-3