Abstract
Purpose
The response of the hypothalamic–pituitary–adrenal (HPA) axis to the sustained stress of sepsis has been the focus of study in recent years because the early phase of sepsis is known to be dominated by major alterations in the HPA axis. This prospective observational study aimed at assessing the predictive values of copeptin and HPA hormones in determining sepsis progression and mortality in the emergency department (ED).
Methods
Serum arginine vasopressin (AVP) and copeptin concentrations were measured upon ED admission. Baseline levels of total and free cortisol and adrenocorticotrophic hormone (ACTH) were measured within 24 h of ED admission. Mortality in Emergency Department Sepsis (MEDS) score was calculated at enrollment.
Results
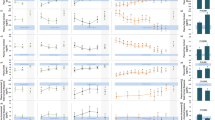
Our findings demonstrated that serum copeptin, baseline total cortisol, baseline free cortisol and baseline ACTH concentrations gradually increased, based upon the increasing severity of the disease (p < 0.001). Multivariate logistic regression analysis showed that copeptin and total cortisol baseline concentrations were independent predictors of septic shock (odds ratio = 1.034 and 1.355, respectively) and 28-day mortality (odds ratio = 1.039 and 1.499, respectively). The areas under the receiver operating characteristic curve (AUC) for copeptin level in prediction of septic shock was 0.856 and 28-day mortality was 0.826. Importantly, AUC analysis of the combination of copeptin, total cortisol baseline, MEDS score, and procalcitonin level resulted in a more significant prognostic ability than analysis of each parameter alone (p < 0.001).
Conclusions
Increased copeptin and HPA hormones baseline levels may provide crucial information for risk stratification in a variety of septic states in the ED. Furthermore, measurements of copeptin level and serum baseline cortisol concentration are promising independent prognostic markers for mortality in patients with severe sepsis or septic shock.



Similar content being viewed by others
References
Martin GS, Mannino DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 348:1546–1554
Antonelli M, Bonten M, Chastre J, Citerio G, Conti G, Curtis JR, De Backer D, Hedenstierna G, Joannidis M, Macrae D, Mancebo J, Maggiore SM, Mebazaa A, Preiser JC, Rocco P, Timsit JF, Wernerman J, Zhang H (2012) Year in review in Intensive Care Medicine 2011. II Cardiovascular, infections, pneumonia and sepsis, critical care organization and outcome, education, ultrasonography, metabolism and coagulation. Intensive Care Med 38(3):345–358
Marik PE, Pastores SM, Annane D, Meduri GU, Sprung CL, Arlt W, Keh D, Briegel J, Beishuizen A, Dimopoulou I, Tsagarakis S, Singer M, Chrousos GP, Zaloga G, Bokhari F, Vogeser M, American College of Critical Care Medicine (2008) Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: consensus statements from an international task force by the American college of critical care medicine. Crit Care Med 36:1937–1949
Molenaar N, Johan Groeneveld AB, Dijstelbloem HM, de Jong MF, Girbes AR, Heijboer AC, Beishuizen A (2011) Assessing adrenal insufficiency of corticosteroid secretion using free versus total cortisol levels in critical illness. Intensive Care Med 37:1986–1993
Annane D, Sébille V, Troché G, Raphaël JC, Gajdos P, Bellissant E (2000) A 3-level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA 283(8):1038–1045
Moreno R, Sprung CL, Annane D, Chevret S, Briegel J, Keh D, Singer M, Weiss YG, Payen D, Cuthbertson BH, Vincent JL (2011) Time course of organ failure in patients with septic shock treated with hydrocortisone: results of the Corticus study. Intensive Care Med 37(11):1765–1772
Annane D, Sébille V, Charpentier C, Bollaert PE, François B, Korach JM, Capellier G (2002) Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 288(7):862–871
Boonen E, Vervenne H, Meersseman P, Andrew R, Mortier L, Declercq PE (2013) Reduced cortisol metabolism during critical illness. N Engl J Med 368(16):1477–1488
Kumar V, Sharma A (2010) Is neuroimmunomodulation a future therapeutic approach for sepsis? Int Immunopharmacol 10(1):9–17
Aguilera G, Rabadan-Diehl C (2000) Vasopressinergic regulation of the hypothalamic-pituitary-adrenal axis: implications for stress adaptation. Regul Pept 96:23–29
Struck J, Morgenthaler NG, Bergmann A (2005) Copeptin, a stable peptide derived from the vasopressin precursor, is elevated in serum of sepsis patients. Peptides 26:2500–2504
Manglik S, Flores E, Lubarsky L, Fernandez F, Chhibber VL, Tayek JA (2003) Glucocorticoid insufficiency in patients who present to the hospital with severe sepsis: a prospective clinical trial. Crit Care Med 31(6):1668–1675
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G, International Sepsis Definitions Conference (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International sepsis definitions conference. Intensive Care Med 29(4):530–538
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL (2012) Moreno R; Surviving sepsis campaign guidelines committee including The Pediatric Subgroup (2013) surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care Med 39(2):165–228
Oda S, Hirasawa H, Sugai T, Shiga H, Nakanishi K, Kitamura N, Sadahiro T, Hirano T (2000) Comparison of sepsis-related organ failure assessment (SOFA) score and CIS (cellular injury score) for scoring of severity for patients with multiple organ dysfunction syndrome (MODS). Intensive Care Med 26(12):1786–1793
Lesu Olivier, Roussy Jean-Francois, Chagnon Frederic, Gallo-Payet Nicole, Dumaine Robert, Sarret Philippe (2010) Proven infection-related sepsis induces a differential stress response early after ICU admission. Crit Care 14(4):R131
Calandra T, Cohen J, International Sepsis Forum Definition of Infection in the ICU Consensus Conference (2005) The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med 33(7):1538–1548
Guignant C, Voirin N, Venet F, Poitevin F, Malcus C, Bohé J, Lepape A, Monneret G (2009) Assessment of pro-vasopressin and pro-adrenomedullin as predictors of 28-day mortality in septic shock patients. Intensive Care Med 35(11):1859–1867
Dimopoulou I, Stamoulis K, Ilias I, Tzanela M, Lyberopoulos P, Orfanos S, Armaganidis A (2007) A prospective study on adrenal cortex responses and outcome prediction in acute critical illness: results from a large cohort of 203 mixed ICU patients. Intensive Care Med 33:2116–2121
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden Index and its associated cutoff value. Biom J 47:458–472
Pepe MS, Cai T, Longton G (2006) Combining predictors for classification using the area under the receiver operating characteristic curve. Biometrics 62:221–229
Jochberger S, Morgenthaler NG, Mayr VD, Luckner G, Wenzel V, Ulmer H, Schwarz S, Hasibeder WR, Friesenecker BE, Dunser MW (2006) Copeptin and arginin vasopressin concentrations in critically ill patients. J Clin Endocrinol Metab 91:4381–4386
Morgenthaler Nils G, Muller Beat, Struck Joachim, Bergmann Andreas, Redl Heinz, Christ-Crain Mirjam (2007) Copeptin, a stable peptide of the arginine vasopressin precursor, is elevated in hemorrhagic and septic shock. Shock 28(2):219–226
Lee Jan Hau, Chan Yoke Hwee, Lai Oi Fah, Puthucheary Janil (2013) Vasopressin and copeptin levels in children with sepsis and septic shock. Intensive Care Med 39:747–753
Purhonen AK, Vänskä M, Hämäläinen S, Pulkki K, Lehtikangas M, Kuittinen T, Nousiainen T, Koivula I, Jantunen E, Juutilainen A (2012) Plasma copeptin in the assessment of febrile neutropenia. Peptides 36(1):129–132
Hamrahian AH, Oseni TS, Arafah B (2004) Measurements of serum free cortisol in critically ill patients. N Engl J Med 350:1629–1638
Finlay WE, McKee JI (1982) Serum cortisol levels in severely stressed patients. Lancet I:1414–1415
Arafah Baha M (2006) Hypothalamic pituitary adrenal function during critical illness: limitations of current assessment methods. J Clin Endocrinol Metab 91:3725–3745
Ugarte H, Silva E, Mercan D, De Mendonca A, Vincent JL (1999) Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med 26:498–504
de Kruif MD, Lemaire LC, Giebelen IA, Struck J, Morgenthaler NG, Papassotiriou J, Elliott PJ, van der Poll T (2008) The influence of corticosteroids on the release of novel biomarkers in human endotoxemia. Intensive Care Med 34:518–522
Acknowledgments
This study was supported by the National Clinical Key Specialty Construction Project Funds (No. 2012-649) and 2012 Beijing City Outstanding Doctoral Dissertation Funds (No. 2012-1002501).
Conflicts of interest
All authors declare that there are no actual or potential conflicts of interest, including any financial, personal, or other relationships.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message:
Copeptin and serum cortisol levels may provide crucial information for risk stratification in a variety of septic states in the ED. A probability of clinical risk parameter combined with serum copeptin, total cortisol baseline and PCT concentrations was the best biological predictor of sepsis diagnosis and offered substantial added value to each parameter individually.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Q., Dong, G., Zhao, X. et al. Prognostic significance of hypothalamic–pituitary–adrenal axis hormones in early sepsis: a study performed in the emergency department. Intensive Care Med 40, 1499–1508 (2014). https://doi.org/10.1007/s00134-014-3468-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3468-4