Abstract
Purpose
To investigate safety and clinical findings of bilevel positive airway pressure (BiPAP) utilization in children 20 kg or less for asthma exacerbations.
Methods
Retrospective and prospective descriptive analysis of 165 enrolled subjects with moderate and severe asthma exacerbations who weighed 20 kg or less and who received BiPAP treatment at a large, urban children’s hospital pediatric emergency department (PED).
Results
Age was 0.6–8.27 years (mean 3.7 years, SD 1.6 years). None exhibited worsening hypoxia, pneumothorax, or death. Four progressed to intubation after significant period on BiPAP. Overall, BiPAP subjects showed improvement in pediatric asthma score (PAS). BiPAP initiation PAS range was 8–15 (mean 12.1, SD 1.6); BiPAP termination or 4 h PAS mean was 6.3 (SD 2.2); delta PAS showed improvement mean 5.8 (SD 2.4). Seventy-one had trial off BiPAP in PED for clinical improvement; seven were restarted. PED BiPAP duration range was 30–720 min (mean 210 min, SD 158 min); total hospitalization BiPAP duration was 1–90 h. Ninety-nine (60%) subjects were admitted to the PICU and continued BiPAP for 0–47 h (mean 6.6 h, SD 8.6 h). Fifty-seven (35%) required ward admission; none were transferred to PICU. Nine (5%) were discharged home from the PED; none returned within 72 h.
Conclusions
BiPAP utilization in acute pediatric asthma exacerbations for patients 20 kg or less is safe and may improve clinical outcomes. These findings warrant future prospective investigation of BiPAP efficacy in pediatric asthma patients.
Similar content being viewed by others
Introduction
The prevalence of asthma in young children has increased [1], and severe asthma exacerbations have become more resistant to standard therapies [2, 3]. Furthermore, reports note complications after intubation of the asthmatic patient [4–6]. When traditional therapies are insufficient, bilevel positive airway pressure (BiPAP) has been a safe and effective asthma therapeutic intervention in the pediatric emergency department (PED) and pediatric intensive care unit (PICU) [7–14].
BiPAP devices cycle between an inspiratory and expiratory positive airway pressure (IPAP and EPAP). BiPAP provides respiratory support by unloading the diaphragm and accessory muscles, increasing tidal volume and minute ventilation, opening obstructed or collapsed alveoli, and decreasing the frequency of occlusive apnea and hypopnea [15, 16]. Effective administration of BiPAP requires a well-fitted mask, optimal patient–ventilator synchrony (i.e., appropriate patient mental status and cooperation), and well-trained pediatric respiratory therapists to continuously monitor the circuit.
Traditionally, BiPAP has been used for pediatric patients with neuromuscular disorders, chronic lung disease, and obstructive airways [17]. Some recommendations have limited BiPAP use in pediatrics to children who weigh greater than 20 kg due to concern that small children are incapable of initiating a supported breath while on BiPAP.
However, use of BiPAP as a beneficial treatment modality for acute severe asthma exacerbations in children is becoming more widely described and accepted in children of all weights [6–19]. The purpose of this study is to assess and report the safety of BiPAP use with traditional therapies for the treatment of acute severe asthma exacerbations in children who weigh 20 kg or less in the PED population.
Methods
We selected the study sample from the population of patients admitted to the PED of an urban children’s hospital. The study was a segment of a quality assurance (Q/A) program for BiPAP use in PED asthma patients. The study was approved by the internal review board.
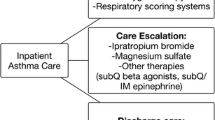
BiPAP was implemented solely by the PED attending physician, for the treatment of children with status asthmaticus who were in need of escalation in treatment, refractory to conventional medical management, resistant to aggressive therapy, progressing towards respiratory failure or considered to have a severe exacerbation based on a pediatric asthma score (PAS) (Table 1). The PAS was developed from expert consensus National Institutes of Health (NIH) asthma management guidelines [20, 21]. All medical personnel at our children’s hospital have used a modified version of this score for over 15 years in the PED, intensive care unit, and on the wards to measure acute asthma severity. Subjects are scored on a scale of 0–3 in five categories including respiratory rate, oxygen saturation, auscultation, retractions, and dyspnea. The individual component scores are summed to provide a total score. A total score of 5–7 signifies a mild exacerbation, 8–11 a moderate exacerbation, and 12–15 a severe exacerbation.
The BiPAP (Q/A) program was started in 2005 with revisions in July 2009. In 2005, patient charts including BiPAP ventilatory records were reviewed for BiPAP treatment failure, intubations for respiratory failure, poor outcomes such as pneumothorax and aspiration, dispositions (discharge to PICU, hospital ward or home), lengths of hospital stay, and deaths. This Q/A process was refined in July 2009 to include patients’ medical history and disease course, a detailed asthma history, physical examination findings, recurrent PAS calculations, treatments prior to initiation of BiPAP, BiPAP settings and duration, PED disposition, and lengths of stay in either PICU or the ward.
Using billing data, we performed a retrospective chart review analysis of pediatric patients placed on BiPAP from January 2005 to July 2009. During the interval from August 2009 to November 2010, BiPAP data sheets were completed at the bedside by the treating PED respiratory therapist at time of BiPAP therapy. Additional information after disposition for PED was collected retrospectively.
Patient charts were reviewed for the following inclusion criteria: (a) received BiPAP therapy while admitted to the PED, (b) weight of 20 kg or less, and (c) a diagnosis of asthma, status asthmaticus, reactive airway disease or acute bronchospasm. We excluded subjects who had: (a) BiPAP therapy duration of less than 30 min, (b) routine home BiPAP therapy, (c) chronic lung disease, (d) neuromuscular disorders, (e) cardiovascular disorders, (f) gestational age less than 28 weeks, and (g) PAS <8.
Data collected from the subject’s chart included: age; gender; weight; past medical history; history of present illness; physical examination characteristics; triage vital signs; time of BiPAP initiation with machine settings; PAS upon BiPAP initiation, at 4 h on BiPAP when applicable, and upon termination if removed in PED; treatments received prior to and while on BiPAP; duration on BiPAP; disposition of the subject; and length of stay if hospitalized. Charts were reviewed for intubation, worsening hypoxia, pneumothorax, death, and other complications.
Our protocol employed BiPAP masks covering the patient’s nose and mouth applied by a specially trained PED respiratory therapist who frequently assessed for leaks, malfunctions or subjects not triggering the BiPAP cycle. BiPAP administration was via either a BiPAP Vision or Vision V60 ventilator (Respironics Inc., Carlsbad, CA). Subjects concurrently received traditional aerosols through the circuit.
Results
During the study period, 165 subjects met the inclusion and exclusion criteria. Data were collected prospectively for 53 (32%) subjects and retrospectively for 112 (68%). Subjects ranged in weight from 7.5 to 20 kg (average 15.7 kg, SD 3.4 kg). Age ranged from 0.6 to 8.27 years (average 3.7 years, SD 1.6 years); 64% were male.
None of the following complications were reported in the PED or PICU: death or pneumothorax. Three subjects were intubated in the PED after a significant period of time on BiPAP. One was intubated during the retrospective phase of the study, and two during the prospective phase. One subject was intubated in the PICU during the prospective phase of the study after a total of 3 h on BiPAP; duration of BiPAP in PED was 1.5 h and in the PICU was 1.5 h (2.4% total subjects intubated) (Table 2). Three were intubated for a decline in mental status; two of these three had concurrent hypoxia. Three of these subjects were extubated in less than 24 h. One remained intubated for 3.5 days. Vomiting was documented for one subject (0.6%), who was 5.4 years old; he removed his mask before vomiting. He was given one dose of ondansetron and continued on BiPAP therapy for more than 7 h without complication. There was no resultant aspiration pneumonia or pneumonitis for this subject. Six subjects were excluded from the study for a BiPAP time of less than 30 min; all were excluded for agitation. These six subjects ranged in age from 1 to 4 years. Four were admitted to the general ward and two to the PICU after receiving traditional therapies in the PED; none were intubated.
Of the patients enrolled, 144 (87%) patients reported a prior diagnosis of asthma. One hundred twenty-two (74%) patients reported at least one asthma-related emergency department visit in the past year, 92 (56%) patients had a history of an asthma-related hospital admission to a general pediatrics ward, and 41 (25%) patients had been admitted to PICU for asthma-related complications in the past. Thirteen (8%) had a prior history of intubation, and 16 (10%) had a prior history of BiPAP use. Nine subjects were enrolled more than once on separate PED visits. These individual events were spaced by 1–24 months. No subjects enrolled had more than three events on BiPAP during the study period.
The analysis revealed a recent history, as reported by the family and a standard question in our PED asthma assessment tool, of cough in 88% of subjects for 2.3 (SD 2.9) days, increased work of breathing in 86% for 1.2 (SD 0.6) days, wheeze in 89% for 1.5 (SD 0.8) days, and congestion in 70% for 2.6 (SD 3.3) days. Fifty-nine percent of subjects admitted to home rescue inhaler use. Fever was reported in 20% of subjects, vomiting in 22%, and chest pain in 7%.
On initial physical examination, the common findings were retractions (99%), wheezing (94%), abdominal breathing (72%), and diminished air entry (64%). Other less commonly documented physical examination findings included nasal flaring (59%), grunting (16%), tripoding (14%), and rales (10%).
The average time from PED presentation to BiPAP initiation was 142 (SD 104) min. All subjects received inhaled beta-2 agonists and either oral or intravenous steroids prior to or at initiation of BiPAP. Other asthma therapies received by the patients prior to or during BiPAP therapy included magnesium sulfate, epinephrine aerosols, and subcutaneous terbutaline or epinephrine (Table 3). Intravenous salbuterol is not available at our institution. BiPAP settings were determined by the treating physician and were recorded for 157 subjects (Table 4). The eight subjects for whom we do not have data were part of the retrospective cohort, and we could not find documentation of settings.
One hundred nine (66%) of the subjects had a documented PAS after 4 h on BiPAP or upon discontinuation of BiPAP (Fig. 1). The PAS upon BiPAP initiation ranged from 8 to 15 (mean 12.1, SD 1.6), while the PAS upon BiPAP termination ranged from 0 to 15 (mean 6.3, SD 2.2). This was an average improvement of BiPAP PAS from initiation to termination with mean of 5.8 (SD 2.4). Of these 109 subjects, 86 (79%) had an improvement in their PAS as compared with the BiPAP start time of greater than four points, 2 (1.8%) had no change, and 1 (0.9%) had an increase in their calculated score (increased three points).
Subjects remained on BiPAP from 1 to 90 h during their total hospital stay. The duration on BiPAP in only the PED ranged from 30 to 720 min (mean 210 min, SD 158 min). Seventy-one (43%) subjects were trialed off BiPAP in the PED as the result of an improvement in clinical status as determined by the treating PED physician; seven were replaced on BiPAP after being off for 30–140 min. None progressed to intubation in this group. Five subjects were taken off after having been on for 60–130 min because they stopped tolerating it due to agitation; none progressed to intubation. Ninety-nine (60%) subjects were admitted to the PICU and, once there, remained on BiPAP for another 0–47 h (mean 6.6 h, SD 8.6 h). Fifty-seven (35%) subjects were admitted to the general pediatrics ward. None of the patients admitted to the general pediatrics floor required transfer to the PICU. Nine (5%) patients were discharged from the PED. Seven of these nine subjects were admitted to the observation unit in the PED. Two (1.2%) patients were not admitted but discharged to home from the PED; they were on BiPAP 90 and 114 min with total length of stay in the PED of 11 and 9 h, respectively. These patients were re-evaluated by either the PED or the admitting physician and deemed appropriate for discharge to home. None returned to our PED within 72 h of discharge.
Discussion
To our knowledge, this study is the first detailed descriptive analysis of therapeutic application of BiPAP in pediatric patients who weigh 20 kg or less with severe asthma exacerbation. There has been hesitation by some healthcare providers to utilize BiPAP treatment in pediatric patients with severe asthmatic exacerbations and especially in children who weigh less than 20 kg. Our results indicate that BiPAP is safe and well tolerated in asthmatic children who weigh 20 kg or less during moderate and severe exacerbations. Children as young as 7 months of age and weighing as little as 7.5 kg tolerated the BiPAP circuit without death or pneumothorax.
Additionally, our data demonstrate that BiPAP can be a noninvasive therapeutic adjunct in moderate and severe asthma exacerbation in patients who weigh 20 kg or less and might reduce the need for endotracheal intubation. Four subjects in the study cohort progressed to endotracheal intubation after a significant period of time on BiPAP. This occurred primarily in the prospective phase of our study as a result of the PED attending physician’s increase in clinical experience and comfort level with BiPAP therapy. Physicians at our institution are utilizing BiPAP earlier and more often in an attempt to prevent intubation of asthmatic patients. However, it was probably inevitable that subjects would progress to intubation. This was delayed in time by utilizing BiPAP. Three of our four intubated subjects experienced a decline in mental status, which is a contraindication to BiPAP use and a compelling reason to proceed with intubation. The other had progression to clinical respiratory failure. Unfortunately, we are unable to quantify how many subjects escaped intubation as a result of treatment with BiPAP; however, during our chart review, we noted that PED physician’s would comment in the patient chart that BiPAP may have prevented intubation of several of the study subjects.
Other complications we observed included vomiting and agitation. The subject who vomited did not experience pneumonitis or aspiration pneumonia and did well on BiPAP after a dose of ondansetron. For subjects with documented emesis on the circuit, our suggestion is to premedicate with an antiemetic such as ondansetron. Furthermore, for agitated subjects, sedation medications such as ketamine boluses or an infusion may be an appropriate choice. Further investigation is warranted for these suggestions.
Finally, our results indicate that the smaller tidal volumes and negative inspiratory pressures in children who weigh 20 kg or less are able to trigger the BiPAP circuit and receive a therapeutic benefit. It bears noting that our BiPAP protocol includes dedicated PED pediatric respiratory therapists who initiate, titrate, and continuously monitor the process and are trained to notice clinical improvement as well as signs of BiPAP circuit intolerance or worsening respiratory distress. This degree of expertise and monitoring is warranted for this relatively new mode of airway management.
Despite being such an acutely ill study population, more than 79% of the subjects demonstrated clinical improvement based on a decrease in the PAS of at least four points after 4 h or at termination of BiPAP treatment. With the increasing trends in asthma severity, these data suggest that broader use of BiPAP may help reduce progression to intubation for severe asthma exacerbations. These aspects warrant more detailed scientific investigation.
There are several limitations to this study. The primary limitation is the comparison of retrospective with prospective data. There are multiple selection biases that occur with this process. The first is that the use of BiPAP in the early data collection phase or during the retrospective portion of the study provided a more restricted data set. However, in later years (or during the prospective portion of the study), BiPAP had gained more clinical acceptance, application, and knowledge for the PED attending physician. We believe this is evident from the three subjects who proceeded to intubation in the prospective phase of our study. We suspect that these subjects may have been intubated had they presented to the PED earlier in the study period. To continue, two-thirds of our data collection is limited to only what is documented in the medical record; for example, we are missing BiPAP setting data for eight patients enrolled in the study. However, due to an adjustment in our quality analysis program unveiled in July 2009, patients were identified in a prospective manner, so a more complete data set was available for analysis after that time. Despite the limitation due to selection bias, we felt it was important to include all data in an effort to increase our sample size.
Another limitation is that the patients included were those given a diagnosis of asthma, status asthmaticus, reactive airway disease or acute bronchospasm by the treating physician. As this is often a more difficult diagnosis to make in younger patients, some patients who should have been included may have been missed and others who were included may not actually have a reactive airway but instead another respiratory process (i.e., viral induced). Finally, BiPAP was initiated at different points in a patient’s clinical course based on the treating physician’s discretion; therefore, it is difficult to discern if the subject’s clinical course was the result of BiPAP initiation or other treatment modalities.
In conclusion, our study supports that BiPAP is a safe mode of noninvasive respiratory support when used in children who weigh 20 kg or less. These results are consistent with the findings from prior BiPAP studies in children. No mortality, pneumothoraces, aspirations or morbidity were demonstrated in this study. Overall, the study group improved clinically, and nine were even safely discharged to home from the PED. A further prospective and randomized scientific investigation is warranted to assess the efficacy of BiPAP in the treatment of all children with asthma exacerbations, and based on this scientific validation, children who weigh 20 kg or less should not be excluded from such studies.
References
Akinbami LJ, Schoendorf KC (2002) Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics 110:315–322
Busse WW, Banks-Schlegel S, Wenzel SE (2000) Pathophysiology of severe asthma. J Allergy Clin Immunol 106:1033–1042
McFadden ER Jr (2003) Acute severe asthma. Am J Respir Crit Care Med 168:740–759
Roberts JS, Bratton SL, Brogan TV (2002) Acute severe asthma: differences in therapies and outcomes among pediatric intensive care units. Crit Care Med 30:581–585
Tuxen D, Lane S (1989) The effects of ventilator pattern on hyperinflation, airway pressures, and circulation in mechanical ventilation of patients with severe air-flow obstruction. Am Rev Respir Dis 140:5–9
Zimmerman JL, Dellinger RP, Shah AN, Taylor RW (1993) Endotracheal intubation and mechanical ventilation in severe asthma. Crit Care Med 21:1727–1730
Beers SL, Abramo TJ, Bracken A, Wiebe RA (2007) Bilevel positive airway pressure in the treatment of status asthmaticus in pediatrics. Am J Emerg Med 25:6–9
Carroll CL, Schramm CM (2006) Noninvasive positive airway pressure ventilation for the treatment of status asthmaticus in children. Ann Allergy Asthma Immunol 96:454–459
Joshi G, Tobias JD (2007) A five-year experience with the use of BiPAP in a pediatric intensive care unit population. J Intensive Care Med 22:38–43
Akingbola OA, Simakajornboon N, Hadley EF Jr, Hopkins RL (2002) Noninvasive positive-pressure ventilation in pediatric status asthmaticus. Pediatr Crit Care Med 3:181–184
Thill PJ, McGuire JK, Baden HP, Green TP, Checchia PA (2004) Noninvasive positive-pressure ventilation in children with lower airway obstruction. Pediatr Crit Care Med 5:337–342
Needleman JP, Sykes JA et al (2004) Noninvasive positive pressure ventilation in the treatment of status asthmaticus. Pediatr Asthma Allergy Immunol 17:272–277
Fortenberry JD, Del Toro J, Jefferson LS, Evey L, Haase D (1995) Management of pediatric acute hypoxemic repiratory insufficiency with bilevel positive airway pressure (BiPAP) nasal mask ventilation. Chest 108:1059–1061
Padman R, Lawless ST, Kettrick RG (1998) Noninvasive ventilation via bilevel positive airway pressure support in pediatric practice. Crit Care Med 26:169–173
Deis JN, Abramo TJ, Crawley L (2008) Noninvasive respiratory support. Pediatr Emerg Care 5:331–341
Akingbola OA, Hopkins RL (2001) Pediatric noninvasive positive pressure ventilation. Pediatr Crit Care Med 2:164–169
Hostetler MA (2008) Use of noninvasive positive-pressure ventilation in the emergency department. Emerg Med Clin North Am 26:929–939
Schramm CM, Carroll CL (2009) Advances in treating acute asthma exacerbations in children. Curr Opin Pediatr 21:326–332
Levine DA (2008) Novel therapies for children with severe asthma. Curr Opin Pediatr 20:261–265
Qureshi F, Pestian J, Davis P, Zaritsky A (1998) Effect of nebulized ipratropium on the hospitalization rates of children with asthma. N Engl J Med 339:1030–1035
Guidelines for the diagnosis and management of asthma (1991) Bethesda, Md. National Heart, Lung and Blood Institute (NIH publication no. 91–3042)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Williams, A.M., Abramo, T.J., Shah, M.V. et al. Safety and clinical findings of BiPAP utilization in children 20 kg or less for asthma exacerbations. Intensive Care Med 37, 1338–1343 (2011). https://doi.org/10.1007/s00134-011-2238-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2238-9