Abstract
Objective
To study the effects on volume expansion and myocardial function of colloids or crystalloids in the treatment of hypovolaemic hypotension after cardiac and major vascular surgery.
Design and setting
A single-centre, single-blinded, randomized clinical trial at the intensive care unit of a university hospital.
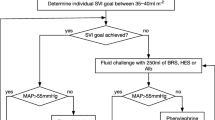
Patients and methods
Patients (n = 67) were subjected to a 90-min filling pressure-guided fluid challenge with saline 0.9% or the colloids gelatin 4%, hydroxyethyl starch 6% or albumin 5%. Biochemical variables and haemodynamics (transpulmonary thermodilution) were measured.
Results
An amount of 1800 (1300–1800) ml of saline or 1600 (750–1800) ml of colloid solution (P< 0.005) was infused. Colloid osmotic pressure (COP) decreased in the saline group and increased in the colloid groups (P< 0.001). Plasma volume increased by 3.0% (–18 to 24) in the saline versus 19% (–11 to 50) in the colloid groups (P< 0.001). Cardiac index increased by median 13% (ns) in the saline group and by 22% in the colloid groups (P< 0.005). The rise in left ventricular stroke work index was greater in the colloid than in the saline groups. The different colloids were equally effective. The rise in cardiac index related to the rise in plasma volume and global end-diastolic volume, confirming plasma volume and preload augmentation by the fluid loading.
Conclusion
After cardiac or major vascular surgery, the pressure- and time-guided fluid response is dependent on the type of fluid used. Colloid fluid loading leads to a greater increase in preload-recruitable cardiac and left ventricular stroke work indices than that with saline, because of greater plasma volume expansion following an increase in plasma COP.


Similar content being viewed by others
References
Boldt J (2000) Volume replacement in the surgical patient – does the type of solution make a difference? Br J Anaesth 84:783–793
Gan TJ, Soppitt A, Maroof M, El-Moalem H, Robertson KM, Moretti E, Dwane P, Glass PSA (2002) Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology 97:820–826
Diehl JT, Lester JL, Corgrove DM (1982) Clinical comparison of hetastarch and albumin in postoperative cardiac patients. Ann Thorac Surg 34:674–677
Moggio RA, Chan Rha C, Somberg ED, Praeger PI, Pooley RW, Reed GE (1983) Hemodynamic comparison of albumin and hydroxyethyl starch in postoperative cardiac surgery patients. Crit Care Med 11:943–945
Kirklin JK, Lell WA, Kouchoukos NT (1984) Hydroxyethyl starch versus albumin for colloid infusion following cardiopulmonary bypass in patients undergoing myocardial revascularization. Ann Thorac Surg 37:40–46
Gallagher JD, Moore RA, Kerns D, Jose AB, Botros SB, Flicker S, Naidech H, Clark DL (1985) Effects of colloid or crystalloid administration on pulmonary extravascular lung water in the postoperative period after coronary artery bypass grafting. Anesth Analg 64:753–758
Karanko MS (1987) Effects of three colloid solutions on plasma volume and hemodynamics after coronary bypass surgery. Crit Care Med 15:1015–1022
Karanko MS, Klossner JA, Laaksonen VO (1987) Restoration of volume by crystalloid versus colloid after coronary artery bypass: hemodynamics, lung water, oxygenation, and outcome. Crit Care Med 15:559–566
London MJ, Ho JS, Triedman JK, Verrier ED, Levin J, Merrick SH, Hanley FL, Browner WS, Mangano DT (1989) A randomized clinical trial of 10% pentastarch (low molecular weight hydroxyethyl starch) versus 5% albumin for plasma volume expansion after cardiac operations. J Thorac Cardiovasc Surg 97:785–797
Ley SJ, Miller K, Skow P, Preisig P (1990) Crystalloid versus colloid fluid therapy after cardiac surgery. Heart Lung 19:31–40
Mastroianni L, Low HBC, Rollman J, Wagle M, Bleske B, Chow MSS (1994) A comparison of 10% pentastarch and 5% albumin in patients undergoing open-heart surgery. J Clin Pharmacol 34:34–40
Wahba A, Sendtner E, Strotzer M, Birnbaum DE (1996) Fluid therapy with Ringer's solution versus Haemaccel following coronary artery bypass surgery. Acta Anaesthesiol Scand 40:1227–1233
Magder S, Lagonidis D (1999) Effectiveness of albumin versus normal saline as a test of volume responsiveness in post-cardiac surgery patients. J Crit Care 14:164–171
Ernest D, Belzberg AS, Dodek PM (2001) Distribution of normal saline and 5% albumin infusions in cardiac surgical patients. Crit Care Med 29:2299–2302
Virgilio RW, Rice CL, Smith DE, James DR, Zarins CK, Hobelmann CF, Peters RM (1979) Crystalloid vs. colloid resuscitation: Is one better? Surg 85:129–139
Boutros AR, Ruess R, Olson L, Hoyt JL, Baker WH (1979) Comparison of hemodynamic, pulmonary, and renal effects of use of three types of fluid after major surgical procedures on the abdominal aorta. Crit Care Med 7:9–13
Zetterström H (1981) Albumin treatment following major surgery. II. Effects on postoperative lung function and circulatory adaptation. Acta Anaesth Scand 25:133–141
Shires GT, Peitzman AB, Albert SA, Illner H, Silane MF, Perry MO, Shires GT (1983) Response of extravascular lung water to intraoperative fluids. Ann Surg 197:515–519
Marik PE, Iglesias J, Maini B (1997) Gastric intramucosal pH changes after volume replacement with hydroxyethyl starch or crystalloid in patients undergoing elective abdominal aortic aneurysm repair. J Crit Care 12:51–55
McKendry M, McGloin H, Saberi D, Caudwell L, Brady AR, Singer M (2004) Randomised controlled trial assessing the impact of a nurse delivered, flow monitored protocol for optimisation of circulatory status after cardiac surgery. Br Med J 329:258–261
Schierhout G, Robert I (1998) Fluid resuscitation with colloid or crystalloid solutions in critically ill patients: a systematic review of randomised trials. Br Med J 316:961–964
Choi PT-L, Yip G, Quinonez L, Cook D (1999) Crystalloids versus colloids in fluid resuscitation: a systematic review. Crit Care Med 27:200–210
Roberts I, Alderson P, Bunn F, Chinnock P, Ker K, Schierhout G (2004) Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev
The SAFE Study Investigators (2004) A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 350:2247–2256
Gödje O, Peyerl M, Seebauer T, Lamm P, Mair H, Reichart B (1998) Central venous pressure, pulmonary capillary wedge pressure and intrathoracic blood volume as preload indicators in cardiac surgery patients. Eur J Cardiothorac Surg 13:533–540
Gödje O, Peyerl M, Seebauer T, Dewald O, Riechart B (1998) Reproducibility of double indicator dilution measurements of intrathoracic blood volume compartments, extravascular lung water and liver function. Chest 113:1070–1077
Hinder F, Poelaert JI, Schmidt C, Hoeft A, Möllhoff T, Loick HM, Van Aken H (1998) Assessment of cardiovascular volume status by transoesophageal echocardiography and dye dilution during cardiac surgery. Eur J Anaesthesiol 15:633–640
Reuter DA, Felbinger TW, Moerstedt K, Weis F, Schmidt C, Kilger E, Goetz AE (2002) Intrathoracic blood volume index measured by thermodilution for preload monitoring after cardiac surgery. J Cardiothorac Vasc Anesth 16:191–196
Combes A, Berneau J-B, Luyt C-E, Trouillet J-L (2004) Estimation of left ventricular systolic function by single transpulmonary thermodilution. Intensive Care Med 30:1377–1383
Groeneveld ABJ, Breukers RMBGE, Verheij J (2004) Clinical value of intrathoracic volumes from transpulmonary dilution. In: Pinsky MR, Payen D (eds) Functional hemodynamic monitoring. Springer, Berlin Heidelberg New York, pp 153–165
Boldt J, Heesen M, Müller M, Pabsdorf M, Hempelmann G (1996) The effects of albumin versus hydroxyethyl starch solution on cardiorespiratory and circulatory variables in critically ill patients. Anesth Analg 83:254–261
Dahn MS, Ledgerwood AM, Higgins RF (1979) Negative inotropic effect of albumin resuscitation for shock. Surgery 86:235–240
Zikria BA, Subbarao C, Oz MC, Popilkis SJ, Sachdev R, Chauban P, Freeman HP, King TC (1990) Hydroxyethyl starch macromolecules reduce myocardial reperfusion injury. Arch Surg 125:930–934
Weil MH, Henning RJ (1979) New concepts in the diagnosis and fluid treatment of circulatory shock. Thirteenth annual Becton, Dickinson and Company Oscar Schwidetsky Memorial Lecture. Anesth Analg 58:124–132
Verheij J, van Lingen A, Raijmakers PGHM, Rijnsburger ER, Veerman DP, Wisselink W, Girbes ARJ, Groeneveld ABJ (2005) Effect of fluid loading with saline or colloids on pulmonary permeability, oedema and lung injury score after cardiac and major vascular surgery. Br J Anaesth 96:21–30
Johansen LB, Bie P, Warberg J, Christensen NJ, Hammerum M, Videbaek R, Norsk P (1997) Hemodilution, central blood volume, and renal responses after an isotonic saline infusion in humans. Am J Physiol 272:R549–R556
Geissler HJ, Allen SJ (1998) Myocardial fluid balance: pathophysiology and clinical applications. Thorac Cardiovasc Surg 46:242–247
Eising GP, Niemeyer M, Günther T, Tassani P, Pfauder M, Schad H, Lange R (2001) Does a hyperoncotic cardiopulmonary bypass prime affect extravascular lung water and cardiopulmonary function in patients undergoing coronary artery bypass surgery ? Eur J Cardiothorac Surg 20:282–289
Squara P (2004) Matching total body oxygen consumption and delivery: a crucial objective. Intensive Care Med 30:2170–2179
Reinhart K, Bloos F (2005) The value of venous oximetry. Curr Opin Crit Care 11:259–263
Acknowledgements
We are indebted to Leo Stokkel, Pieter G.H.M. Raijmakers, G.J. Jaap Teule, Kees H. Polderman, Jan Jaap Spijkstra, Rob J.M. Strack van Schijndel and Arie C. van Loenen, and to B. Braun Medical for an unrestricted research grant supporting the first author.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Verheij, J., van Lingen, A., Beishuizen, A. et al. Cardiac response is greater for colloid than saline fluid loading after cardiac or vascular surgery. Intensive Care Med 32, 1030–1038 (2006). https://doi.org/10.1007/s00134-006-0195-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0195-5