Abstract
Purpose
The aim of this work was to explore the risk factors for distal radius fracture in postmenopausal women.
Patients and methods
A total of 611 postmenopausal women with distal radius fractures were included. In all, 173 patients with unstable distal radius fractures were included (unstable fracture group), while there were 438 patients with stable distal radius fractures (stable fracture group). The control group comprised 800 postmenopausal women with no fracture. A questionnaire survey was conducted.
Results
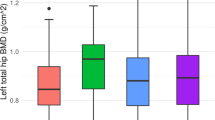
Compared with the control group, the 611 postmenopausal women with distal radius fractures had a higher body mass index (BMI). Advanced age and higher BMI were more common in the unstable fracture group than in the stable fracture group (P <0.05). A higher proportion of the 611 postmenopausal women with a distal radius fracture had fallen in the last 12 months than in the control group. Comorbidities and the frequency of falls in the last 12 months were higher in the unstable fracture group than in the stable fracture group (P < 0.05). A higher proportion of the control group was taking calcium supplements, while the proportion taking calcium supplementation in the unstable fracture group was lower than that in the stable fracture group (P < 0.05). Osteoporosis in the two fracture groups (P < 0.05) was significantly higher than in the control group and was the highest in the unstable fracture group (P < 0.05).
Conclusions
In postmenopausal women, obesity, falls, unknown osteoporosis status, and osteoporosis are associated with high risk of distal radius fracture. If comorbidities and advanced age are also present, this group of persons may be at higher risk for unstable distal radius fractures.
Zusammenfassung
Ziel
Ziel der Arbeit war es, die Risikofaktoren für eine distale Radiusfraktur bei postmenopausalen Frauen zu untersuchen.
Patienten und Methoden
An der Studie nahmen 611 postmenopausale Frauen mit einer distalen Radiusfraktur teil. Dabei wurden 173 Patientinnen mit instabiler (instabile Frakturgruppe) und 438 mit stabiler distaler Radiusfraktur (stabile Frakturgruppe) in die Studie aufgenommen. Die Kontrollgruppe umfasste 800 postmenopausale Frauen ohne Fraktur. Es wurde eine Fragebogenerhebung durchgeführt.
Ergebnisse
Gegenüber der Kontrollgruppe war der Körpermassenindex (BMI) bei den 611 postmenopausalen Frauen mit distaler Radiusfraktur höher. Fortgeschrittenes Alter und höherer BMI waren in der instabilen Frakturgruppe häufiger als in der stabilen (p <0,05). Von den 611 postmenopausalen Frauen mit distaler Radiusfraktur war ein größerer Anteil in den letzten 12 Monaten gestürzt als in der Kontrollgruppe. Komorbiditäten und die Stürze in den letzten 12 Monaten waren häufiger in der instabilen als in der stabilen Frakturgruppe (p < 0,05). Ein größerer Anteil der Kontrollgruppe nahm Kalziumpräparate ein, dagegen war der Anteil derjenigen, die Kalziumpräparate einnahmen, in der instabilen Frakturgruppe niedriger als in der stabilen (p < 0,05). In beiden Frakturgruppen kam eine Osteoporose signifikant häufiger vor als in der Kontrollgruppe (p < 0,05), am häufigsten trat sie in der instabilen Frakturgruppe auf (p < 0,05).
Schlussfolgerung
Bei postmenopausalen Frauen gehen Adipositas, Stürze, unbekannter Osteoporosestatus und Osteoporose mit einem höheren Risiko für eine distale Radiusfraktur einher. Liegen zusätzlich noch Komorbiditäten und fortgeschrittenes Alter vor, so weist diese Personengruppe möglicherweise ein hohes Risiko für eine instabile distale Radiusfraktur auf.
Similar content being viewed by others
References
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(Suppl 2):3–7
Kanis JA, Oden A, Johnell O, Jonsson B (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–427
Roy DK, O’Neill TW, Finn JD (2003) Determinants of incident vertebral fracture in men and women: results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int 14:19–26
Willig R, Luukinen H, Jalovaara P (2003) Factors related to occurrence of hip fractures during a fall on the hip. Public Health 117:25–30
Ismail AA, Pye SR, Cockerill WC (2002) Incidence of limb fracture across Europe: results from the European prospective osteoporosis study (EPOS). Osteoporos Int 13:565–571
Turner RG, Faber KJ, Athwal GS (2007) Complications of distal radius fractures. Orthop Clin North Am 38:217–228
Rosengren BE, Ahlborg HG, Gärdsell P (2010) Bone mineral density and incidence of hip fracture in Swedish urban and rural women 1987–2002. Acta Orthop 81:453–459
Ilyas AM, Jupiter JB (2007) Distal radius fractures: classification of treatment and indications for surgery. Orthop Clin North Am 38:167–173
Tejwani NC, Takemoto RC, Nayak G (2010) Who is lost to followup?: A study of patients with distal radius fractures. Clin Orthop Relat Res 468:599–604
Waris E, Paavola M (2012) Current treatment of distal radius fractures. Duodecim 128:386–398
Brogren E, Wagner P, Petranek M (2013) Distal radius malunion increases risk of persistent disability 2 years after fracture. Clin Orthop Relat Res 471:1691–1697
Nesbitt KS, Failla JM, Les C (2004) Assessment of instability factors in adult distal radius fractures. J Hand Surg Am 29:1128–1138
De Laet C, Kanis JA, Odén A (2005) Body mass index as a predictor of fracture risk: A meta-analysis. Osteoporos Int 16:1330–1338
Lee KH, Kim JY, Yim SJ (2014) Incidence and risk factors of subsequent hip fractures in Korea: multicenter study. J Korean Med Sci 29:992–994
No authors listed (1987) The prevention of falls in later life. A report of the Kellogg International Work Group on the prevention of falls by the elderly. Dan Med Bull 34(Suppl 4):1–24
Dontas IA, YiannakopouIos CK (2007) Risk factors and prevention of osteoporosis-related fractures. J Musculoskelet Neuronal Interact 7:268–272
Luz Rentero M, Carbonell C, Casillas M (2008) Risk factors for osteoporosis and fractures in postmenopausal women between 50 and 65 years of age in a primary care setting in Spain: A questionnaire. Open Rheumatol J 2:58–63
Baim S, Leslie WD (2012) Assessment of fracture risk. Curr Osteoporos Rep 10:28–41
Lane JM, Russel L, Khan SN (2000) Osteoporosis. Clin Orthop Relat Res 372:139–150
Kanis JA, Johansson H, Oden A (2005) A meta-analysis of milk intake and fracture risk: low utility for case finding. Osteoporos Int 16:799–804
Bischoff HA, Stähelin HB, Dick W (2003) Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Res 18:343–351
Padegimas EM, Osei DA (2013) Evaluation and treatment of osetoporotic distal radius fracture in the elderly patient. Curr Rev Musculoskelet Med 6:41–46
Marques EA, Mota J, Carvalho J (2012) Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. Age (Dordr) 34:1493–1515
Martyn-St. James M, Carroll S (2008) Meta-analysis of walking for preservation of bone mineral density in postmenopausal women. Bone 43:521–531
Acknowledgements
This research was supported by grant from Shanghai Municipal Health Bureau (2010146) and Shanghai Hongkou district Board of health (1402–09).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
W. Xu, C. Ni, R. Yu, G. Gu, Z. Wang, and G. Zheng declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Xu, W., Ni, C., Yu, R. et al. Risk factors for distal radius fracture in postmenopausal women. Orthopäde 46, 447–450 (2017). https://doi.org/10.1007/s00132-017-3403-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-017-3403-9