Abstract
Purpose
To evaluate the prevalence of and risk factors associated with anxiety, depression, and insomnia symptoms during the return-to-work period of coronavirus disease 2019 in China.
Methods
The authors conducted a large-scale, nationwide, multicenter, cross-sectional study in China. A population-based quota and snowball sampling were designed to recruit a representative sample. Online questionnaires and telephone reviews were used to collect characteristics and assess psychological and sleep problems. Anxiety, depression, and insomnia symptoms were measured by the generalized anxiety disorder-7, patient health questionnaire-9, and insomnia severity index tools.
Results
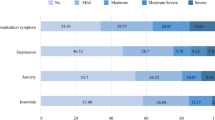
A total of 42,000 participants were recruited from 15 centers, and 36,795 valid questionnaires were received. Generally, 18.3, 14.9, and 17.9% of the participants had anxiety, depression, and insomnia symptoms, respectively, and 2.2–2.7% had severe symptoms. Engaging in outside activity once in ≥ 30 days (OR = 2.719, OR = 2.074, OR = 2.225) and age 50–64 years (OR = 2.431, OR = 1.936, OR = 2.036) were common risk factors for anxiety, depression and insomnia symptoms. Living in Hubei Province (OR = 1.304, OR = 1.242) was a common risk factor for anxiety and insomnia symptoms. Working as frontline medical staff (OR = 2.150) was another risk factor for anxiety symptoms. The health education rate of the samples reached 98.9%. However, the psychological intervention rate was only 16.2%, and 2.5% received targeted interventions.
Conclusions
An increasing number of people might have psychological and sleep problems. However, the current psychological interventions are not sufficient. Efforts should be made to strengthen interventions for high-risk populations.
Similar content being viewed by others
Introduction
The outbreak of infectious diseases is often accompanied by psychological problems, which may have serious long-term impacts [1]. In early 2020, coronavirus disease 2019 (COVID-19) began spreading in China and quickly became a global threat. Similar to previous epidemic diseases, COVID-19 is an infectious disease that is highly contagious and fatal to some patients, but it has spread quickly and widely around the world, which has caused a global pandemic and worries [2,3,4]. The Chinese government adopted a national restriction of outside activities since the time of the Spring Festival (i.e., 25 January 2020) [5]. During the outbreak of COVID-19, several studies alerted that the prevalence of psychological and sleep problems increased and was common among the general population [6,7,8,9]. However, due to a focus on epidemic control and a lack of professional practitioners in mental health, inadequate attention was paid to mental health, and psychological interventions are far from sufficient, a problem that has emerged as a serious challenge to the mental health of the general public [6, 10].
By 22 February 2020, the government had allowed the resumption of non-cross-regional work because of preliminary control of the epidemic [11]. Cross-regional outside activities and nonessential outside activities are still restricted [12]. During the return-to-work period of COVID-19, people are experiencing multiple pressures of concern related to infection, interpersonal isolation, and work resumption, which might have different influences on psychological and sleep problems [13]. However, there is a lack of studies on psychological conditions during the return-to-work period [13, 14]. Moreover, most previous cross-sectional studies on mental health only conducted online surveys for web users or applied only snowball or convenient sampling, and some studies did not perform sampling nationwide, which may decrease their representativeness for the entire Chinese population [7, 9, 15, 16].
Therefore, we conducted this nationwide cross-sectional study to evaluate the prevalence of anxiety, depression and insomnia symptoms and their influential factors in the return-to-work period during the outbreak of COVID-19 in China. A population-based quota and snowball sampling scheme were designed to recruit a representative sample. We hope that this study can evaluate the prevalence of and risk factors associated with psychological and sleep symptoms to target high-risk populations for further interventions. As COVID-19 remains still a global threat, this study can offer a model for the psychological conditions of a large population under isolation and facing epidemic stress during the return-to-work period and help to strengthen preparedness.
Methods
Study population and sampling process
This study is a nationwide, multicenter, cross-sectional study conducted to evaluate the psychological conditions and find the related influential factors during the return-to-work period. Because of the restriction on face-to-face communications and outside activities during the epidemic, the study required all participants or their guardians to provide informed consent by reading an online consent form and clicking an “agree to the consent” button for the online questionnaire or by offering oral consent before a telephone review. This study was reviewed, approved, and supervised by the ethics committee of SanBo Brain Hospital, Capital Medical University.
The protocol was previously established, and the study included pre-investigation and formal investigation. The inclusion criteria of the pre-investigation and formal investigation required all participants to supply informed consent and have an age of 11 years or older, because the scales used in this study are not validated for individuals less than 11 years [17]. The pre-investigation was launched from 10 March 2020 to 13 March 2020 to examine the applicability of the scales, foster multicenter collaboration, and determine the sample size using convenient sampling in several communities. A lucky draw (token amount) was set as the recruitment incentive for participants recruited. All participants were asked to complete several web-based scales, questions about characteristics, and items such as, “For yourself, which data are the most concerning data about COVID-19?”. Participants who finished all scales and questions were considered valid responses, and others who accepted recruiting but did not meet the inclusion criteria, did not respond, or did not finish all scales and questions were considered “drop-out samples”.
The pre-investigation recruited 500 participants in total, and 441 surveys (88.2%) were valid. The data on the daily number of new cases (DNC) were the most concerning (87.5%), which were treated as stratification of different epidemic areas. Based on the pre-investigation, the Generalized Anxiety Disorder-7 scale (GAD-7, scores from 0 to 21, Cronbach’s α = 0.90) [18], the Patient Health Questionnaire-9 (PHQ-9, scores from 0 to 27, Cronbach’s α = 0.86–0.89) [19, 20], and the Insomnia Severity Index (ISI, scores from 0 to 28, Cronbach’s α = 0.83) [21] were used to measure anxiety, depression, and insomnia symptoms in the formal investigation. All scales used were the Chinese versions and were revised for Chinese populations if needed [18,19,20,21]. The suitable classification standards were determined by the Chinese consensus and reviewed by neuropsychologists. These Chinese version scales and cutoff values were commonly used in psychological studies of the Chinese population [9, 22]. The sample size of the formal investigation was determined using the Clopper-Pearson formula (two-sided). According to the pre-investigation, the proportion was set as 0.180, the dropout rate was set as 20%, the confidence level was set as 0.950, and the permissible error was set as 0.005. The PASS (NCSS LLC., Kaysville, Utah, USA; version 15) was used for sample size calculation. The desired sample size was 22,879, and the desired dropout-inflated enrollment sample size was 28,599. Considering that each sampling area should represent people with different characteristics, the sample size was also calculated for each area. The results suggested that each area should recruit at least 3000 participants. After calculation based on the proportion of the population in each area, 42,000 participants were scheduled to be recruited for the formal investigation.
The formal investigation was conducted from March 16, 2020 (4 weeks after the government allowed non-cross-regional work resumption) to 29 March 2020. By 16 March 2020, a total of 3213 deaths and 80,860 confirmed patients were reported based on the National Health Committee daily report. The Chinese tradition is for people to return to their registered residences before the Spring Festival (i.e., 25 January 2020), and the government implemented control over outside activities beginning on 25 January 2020 [5]. Only non-cross-regional work resumption was permitted beginning on 22 February 2020 [11]. Thus, the population distribution was more representative during the survey. Because cross-regional outside activities were still restricted, probability sampling was not possible. A novel population-based nonprobability quota sampling combined with the snowball sampling method was designed to recruit a representative sample. First, we stratified the country into 4 regions (East, Center, West, Northwest) based on the National Economic Population Division (NEPD). The NEPD is a national stratification standard based on the characteristics of the population and the economy established by the National Bureau of Statistics [23]. We determined the quotas for the sample size based on the population proportion (East: recruit 15,000; Center: recruit 12,000; West: recruit 12,000; Northwest: recruit 3,000) provided by the newest Sixth China National Census [23]. The cross-control quota sampling method was used in the sampling centers of each region (first, stratification was based on subregion, gender, age, occupation, and epidemic status; second, cross-control was used to determine the proportion of each layer; and third, the number of participants to recruit with different characteristics was determined). Each center sent invitations to groups with different characteristics to recruit participants according to the quotas. The invitations were sent online, by telephone, via posters, and person-to-person introduction. This selection procedure did not recruit participants based on family to family contacts but was based on recruit groups with different characteristics. Only invited population groups could participate in quota sampling and represent populations with different characteristics. Finally, because some groups were difficult to access (e.g., cured patients, the elderly), snowball sampling was used as a supplement in each center when the center could not recruit the required number of participants with specific characteristics. In the snowball sampling procedure, the participants introduce others with the required characteristics. The recruitment incentive was set as a token payment (lucky draw) after all participants accepted the recruitment. The ethics committee approved the amount, form, and timing of payment for pre-investigation and formal investigation. These novel samples were designed to recruit a representative sample when random sampling could not be achieved. A previous study has been published using a similar sampling strategy [6].
In addition, the DNC (the most concerning data of COVID-19 in the pre-investigation) was collected during the survey period based on the National Health Committee daily report. Epidemic areas were stratified by average DNC during the formal investigation period (Area I: DNC ≥ 10; Area II: 10 > DNC > 0; Area III: DNC = 0) and set as a characteristic of the participants to explore the influence of the epidemic area. Figure 1 shows the regional division, sampling centers, and epidemic areas. Figure 2 shows the sampling process.
Measures
After recruiting enough participants, the survey procedure was performed. Participants who met the criteria were given a network or telephone survey. The online questionnaire and database were provided by WJX (Ranxing LLC., Changsha, Hunan, China). If the participants could not finish the questionnaire online, the investigators gave a telephone interview read by voice, which had the same contents as the online questionnaire to maintain equivalence. Each of the participants was required to answer only once by one type of survey (online or telephone). For the online survey, a network IP address restriction was set to prevent someone from answering multiple times.
The survey included three main sections. The first section addressed demographic characteristics, including gender, age, occupation, education experience, and marriage status. The second section dealt with experience related to COVID-19. The question set included “COVID-19 epidemic status (E1: Cured patient; E2: Confirmed patient; E3: Suspected infection; E4: Close contact, except for frontline medical staff; E5: Frontline medical staff; E6: Others, i.e., noncontacts)”, “outside activity (i.e., working, entertainment, shopping and other outdoor activities which last for some time) since the Spring Festival (once in 1–7 days; once in 8–14 days; once in 15–29 days; once in 30 days or more)”, “memory of similar epidemic experiences (SARS, severe acute respiratory syndrome, outbreak in 2003, China; H1N1, H1N1 flu, outbreak in 2009, China; both; none)”, “return-to-work status (R1: On-site work resumption; R2: Off-site work resumption; R3: No work resumption; R4: On-site study resumption; R5: Off-site study resumption; R6: No study resumption)”, “received health education on COVID-19 (public; target; both; none)”, and “received psychological intervention during COVID-19 outbreak (public, i.e., public psychological education, guiding, or broadcasting, et al.; targeted, i.e., psychological counseling, treatment, et al. which was special for a person; both; none)”. The third section included the standard scales, including the GAD-7, the PHQ-9, and the ISI. According to the introduction of these three scales, participants were asked to answer mainly based on the past 2 weeks. The GAD-7, PHQ-9, and ISI are self-reporting screening measures of anxiety, depression, and insomnia symptoms, and higher scores indicate more likelihood of severe symptoms. GAD-7, PHQ-9, and ISI scores ≥ 10, ≥ 10, and ≥ 15 indicate symptoms, and scores ≥ 15, ≥ 15, and ≥ 22 indicate severe symptoms. For participants of age less than 18, PHQ-9 total scores of 11 or higher are considered to be most specific and sensitive to diagnosis, and these scales have been validated for ages ≥ 11 [24]. Furthermore, a trust test question “did you answer truthfully” was used to evaluate general trust at the end of the survey. Invalid surveys included questionnaires with “no” responses on the trust test, those that did not finish completely, and short response times (i.e., less than 1 min). Participants who accepted recruitment but did not respond to valid questionnaires were considered “drop-out samples”.
Statistical analysis
Continuous variables were presented as the mean ± standard deviation (SD) or ranges and interquartile ranges (IQRs) depending on whether the data distribution was normal (Kolmogorov–Smirnov test; K–S test). Categorical variables were reported as a number and percentage. After the survey, the proportion of demographic characteristics (i.e., age, gender, occupation, regional population, and status of participants) of the participants was compared with the protocol and the Sixth China National Census [25] to check the influence of the drop-out samples and to verify whether the distribution matched the protocol and general Chinese population. After the K–S test was used to explore the distributions of the paired differences, the t test or Wilcoxon signed-rank test was used to compare the continuous variables. Categorical variables were compared by Pearson’s χ2 test.
Pearson’s χ2 test was used to compare the prevalence of anxiety, depression, and insomnia symptoms in different populations. Logistic regression was used to examine the association among independent factors and mental health symptoms. First, univariate unadjusted logistic analyses of variables were performed. Second, variables showing p < 0.05 in the univariate analysis were entered into the multiple logistic regression (backward) to adjust for confounding effects of other variables. Additionally, multicollinearity diagnostics were analyzed for variables that were included in the multivariate analysis to exclude related variables. The variance inflation factor (VIF) < 10 suggested that the variables did not have significant multicollinearity. The correlations of the GAD-7, PHQ-9, and ISI scores were also analyzed by Pearson’s correlation after the K-S normality test. All statistical tests were two-sided, and significance was defined as p < 0.05. The analyses were performed in SPSS (IBM Crop., Armonk, New York, USA; version 26).
Results
Characteristics of the participants
A total of 42,000 participants (quota sampling n = 39,973, 95.2%; snowball sampling n = 2,027, 4.8%) were recruited from 15 centers (East: 5 centers; Center: 3 centers; West: 5 centers; Northwest: 2 centers). A total of 36,795 (response rate = 87.61%) valid questionnaires were received, and others were excluded, because the respondents had ages under 11 (n = 81), refused consent or did not answer (n = 2,562), did not pass the trust question (n = 198), had incomplete answers (n = 2,075), and had short response times (n = 289). Among these participants, 81.3% (n = 34,146) were investigated online, and the other 18.7% (n = 7,854) were surveyed by telephone. The proportion of demographic characteristics (i.e., age, gender, occupation, region, and epidemic status) of the participants was compared with the protocol and the Sixth China National Census [25], and no significant difference was found (p > 0.05), indicating that the drop-out samples did not significantly influence the proportion of the characteristics and that the distribution satisfactorily matched the Chinese population. Table 1 shows the basic characteristics of the participants, and the detailed characteristics are provided in Supplementary Table S1.
The ages of the included participants were 11–86 (IQR 26–56), 50.9% (18,732) of the participants were male, and 49.1% (18,063) were female. A total of 2337 (6.4%) cured patients, 374 (1.0%) confirmed patients, 201 (0.5%) suspected infected, 529 (1.4%) close contacts, and 892 (2.4%) frontline medical staff completed valid questionnaires. After analysis, 86.6% of the participants had resumed work or study, and 39.8% and 100% of these had adopted off-site work or study. Because on-site studies were limited nationwide by the government at the time of sampling, no on-site study participants were recruited.
According to the survey, 7,165 (19.5%) participants engaged in outside activities once every 15 days or more under the control of outside activities. During the COVID-19, a total of 36,388 (98.9%) participants had received health education, but only 5,970 (16.2%) participants had received psychological intervention. Supplementary Table S2 shows the detailed experience of participants related to the epidemic.
Furthermore, the scales used in this study were also tested for reliability of the samples with valid responses. Cronbach’s α values for the GAD-7, PHQ-9, and ISI were 0.87, 0.92, and 0.85, respectively. The acceptable Cronbach’s α for psychometric scales is 0.70 or more, suggesting satisfactory internal consistency [20]. Additionally, the internal consistency of these scales in this study was similar to that of previous studies for the general Chinese population [18,19,20,21].
Anxiety
A total of 18.3% (6,749) of the participants had anxiety symptoms, and 2.6% (975) had severe symptoms. Univariate analysis showed that area, age, occupation, epidemic status, outside activities, and return-to-work status were associated with anxiety symptoms (Supplementary Tables S1 and S2.). After multivariate analysis, engaging in outside activity once in ≥ 30 days (OR = 2.719), age 50–64 years (OR = 2.431), working as frontline medical staff (OR = 2.150), and living in Area I (OR = 1.304) were risk factors for anxiety symptoms (Supplementary Tables S3. and Table 2).
Depression
The PHQ-9 scale showed that 14.9% (5,497) of the participants had depression symptoms, and 2.2% had severe symptoms (scores ≥ 15). In the univariate analysis, the following factors were found to be associated with depression symptoms: age, occupation, marriage status, outside activities, and health education (Supplementary Tables S1 and S2). Multivariate analysis showed that age 50–64 years (OR = 1.936) and engaging in outside activity once in ≥ 30 days (OR = 2.074) were risk factors for depression symptoms (Supplementary Tables S3 and Table 2).
Insomnia
In total, 17.9% (6,581) of the participants had insomnia symptoms, and 2.7% (981) of the participants had severe symptoms. The univariate analysis revealed that area, age, occupation, outside activities, and return-to-work status were associated with insomnia symptoms (Supplementary Tables S1. and S2). The multivariate analysis revealed that engaging in outside activity once in ≥ 30 days (OR = 2.225), age 50–64 years (OR = 2.036), and living in Area I (OR = 1.242) were risk factors for insomnia symptoms (Supplementary Tables S3 and Table 2).
Subgroup analyses and correlations
The participants were stratified by epidemic area, epidemic status, and return-to-work status to explore the risk factors for anxiety, depression, and insomnia symptoms in different subgroups to guide target interventions for specific groups. The detailed information is shown in Table 3. In addition, the prevalence of psychological and sleep problems in different subgroups is presented in Supplementary Table S1 and S2. The GAD-7 and ISI scores were positively correlated in these samples (r = 0.780, p < 0.001). The PHQ-9 and ISI scores were also positively correlated (r = 0.652, p = 0.005). Conversely, the correlation between the GAD-7 and PHQ-9 scores did not show statistical significance (r = 0.415, p = 0.178).
Discussion
This study examined the psychological conditions of individuals during the return-to-work period of COVID-19 in China. Psychological and sleep problems, including anxiety, depression, and insomnia, are common mental health symptoms when epidemics occur [26]. During the COVID-19 epidemic, it is difficult to finish a follow-up study. The authors decided to conduct cross-sectional studies in different time periods with a similar sampling strategy to find potential changes and provide timely directions for target intervention. This research series contained three independent studies. The first study in this research series was a nationwide study for the outbreak period [6]. The second study was a provincial-wide study for the preliminary work resumption period with a resumption proportion of 69.9% [13]. The current nationwide study was the third stage of this research series, which was conducted for a further return-to-work period with a resumption proportion of 86.6%. In addition, the first study stratified the country by the number of confirmed patients to represent the status of different epidemic statuses, the second study stratified Shandong Province according to the geographical division. As the epidemic was preliminary controlled [11], this study applied a novel and complete strategy based on the characteristics of the population and the economy, which was more appropriate for representing the conditions in China in this study. Furthermore, the DNC was set as a characteristic of the participants to explore the influence of the epidemic area.
This study found that 18.3, 14.9, and 17.9% of the participants had anxiety, depression, and insomnia symptoms, respectively, and 2.2–2.7% of them had severe symptoms. Anxiety symptoms were the most common class of problems, followed by insomnia and depression. According to a previous report during the normal period of the Chinese population using similar screening scales, approximately 5.3%, 6.0%, and 8.7% of the general population had anxiety, depression, and insomnia symptoms, respectively [9, 27,28,29,30]. These baseline epidemiological studies suggested that the prevalence of psychological and sleep problems increased during the return-to-work period of COVID-19 in China. Several previous studies used web-based surveys using screening tools to explore the status of psychological status during the COVID-19 epidemic in China and suggested that 16.5–31.6% of people had psychological and sleep problems [7, 9, 15, 16, 31]. Most of these studies suggested a higher prevalence of psychological and sleep problems during different time periods of COVID-19 than during the normal period. However, these studies used different survey areas, sampling strategies, and survey procedures. In addition, most of these studies might not have great representativeness, because they only focused on web users, were not performed nationwide and did not consider the distribution of people with different characteristics. For example, Le et al. conducted a large-sample, cross-sectional, population-based, online survey study using the GAD-7, PHQ-9, and ISI from February 28, 2020 to March 11, 2020 for the Chinese population through the health page on the Chinese website Joybuy, an ecommerce and information service platform. Those researchers suggested that the rates of mental health symptoms were 27.9% for depression, 31.6% for anxiety, and 29.2% for insomnia, values that were higher than ours [9]. Although their study had extensive geographic coverage across China and a large sample size, it was conducted among internet users who were young and highly educated. The people who were willing to participate might pay more attention to the epidemic, which might explain a higher prevalence than in the present study. Thus, it was difficult to conclude the appropriate prevalence and potential changes of psychological and sleep problems based on simple integration of existing data. Although current studies have provided important information for different regions and time periods, the precise prevalence of psychological problems and potential changes of different time periods of the epidemic still have to be concluded, necessitating further cross-sectional studies with random sampling designs and well-designed follow-up studies.
The current research team conducted a series of studies using similar sampling strategies and geographic areas [6, 13]. The prevalence values for anxiety, depression, and insomnia symptoms in these studies were 12.2, 11.0, and 13.3% during the outbreak; 20.8, 19.5, and 21.7% during the preliminary work resumption period (the resumption proportion was 69.9%); and 18.3, 14.9, and 17.9% during the further return-to-work period (in this study, the resumption proportion was 86.6%). These findings suggested potential changes in psychological status, which could be summarized as follows: the prevalence of psychological and sleep problems was higher during the preliminary work resumption period than during the initial outbreak status and was lower after a further increase in the resumption rate. These observations might relate to further economic recovery, personal contact, and epidemic control. Furthermore, the main public news and topics have changed to normal subjects, which might provide confidence and optimism for the public [32]. However, it should also be noted that the prevalence of psychological and sleep problems during the further return-to-work period was still higher than that during the outbreak period [6]. Tan et al. suggested that when psychological measures were administered effectively, returning to work did not cause a high level of mental health symptoms in the workforce, which indicated the importance of psychological interventions during the resumption period.
This study also showed that 98.9% of participants received COVID-19 health education, and 45.0% received targeted education. Large-scale health education is important for disease control, especially for epidemic disease. Using health education, knowledge of the main transmission routes can be improved, and person-to-person transmission can be reduced [33]. However, only 16.2% of the participants had received psychological interventions during COVID-19, and 2.5% had received targeted interventions, which is not sufficient considering the number of people with potential psychological problems and might be related to the restrictions on outdoor activities. Although face-to-face counseling and individualized treatment may be limited, because of the epidemic, a pilot study in Hong Kong during SARS suggested that online or telephone interventions could also be effective [33]. Previous studies that conducted interventions online or via mobile phones for people who experienced mental health problems also showed acceptable efficacy [34,35,36]. We suggest that additional efforts are needed to strengthen psychological interventions in any way that may be effective and to launch individualized interventions in time if possible.
The epidemic area was stratified by average DNC during the formal investigation period. Living in Area I was a risk factor for anxiety and insomnia symptoms. Area I consisted of Hubei Province, which mainly includes Wuhan city. Hubei Province was the place of the early transmission of COVID-19 in China and had higher rates of infection and death reports [37]. Three days before the national outside activity restriction, the Wuhan government decided to conduct strict blocking from other cities and prohibit outdoor activities [38]. Although the epidemic situation in Hubei Province has improved significantly, outside activities were still restricted in this area during the survey period. This study found that 37.0% of the participants in Area I had engaged in outside activity once in ≥ 30 days, which was significantly higher than that reported by participants living in other areas. However, no significant difference was found in psychological intervention between Area I and other areas. Under the long-term pressure of isolation and concerning infection, psychological interventions among Hebei Province residents should be treated as important and prioritized. For Area I, working as frontline medical staff (OR = 2.964) and age 50–64 years (OR = 1.837) were risk factors for anxiety symptoms, and engaging in outside activity once in ≥ 30 days (OR = 2.453) and having only accepted public psychological intervention (OR = 2.031) were risk factors for depression symptoms, which could indicate the high-risk group for interventions.
Age factors were also found to be associated with psychological problems. Age 50–64 years was a risk factor for anxiety, depression and insomnia symptoms. According to the epidemiology study by Huang et al. [39], 50- to 64-year-old individuals have a slightly higher prevalence of anxiety and depression disorders (4.5%) than other adult groups (3.8–4.1%) in China, which might be an important explanation for this factor. Previous studies suggested that elderly individuals could be more susceptible and had severe symptoms of COVID-19, which might be lethal [40], a factor that might increase the concerns of this age group. Work as frontline medical staff was also found to be associated with anxiety symptoms. Previous reports suggested that medical staff had higher possibilities of psychological distress after an epidemic outbreak [1, 41]. For a group at high risk of infection and with stressful work, efforts should be made to strengthen psychological interventions among frontline medical staff. Furthermore, several studies suggested that the brutal death of loved individuals from COVID-19 might promote a high risk of psychological problems [42, 43]. However, the Chinese culture is sensitive in asking about death around Spring Festival. Furthermore, considering that it might cause more suffering for participants who had close loved ones who contracted or died from COVID-19, especially when there might not be sufficient resources for timely psychological intervention after the investigation, the research team and ethics committee decided not to include this question in the present study, which could be the next research direction when available.
Participants engaging in outside activity once in ≥ 30 days were found to be associated with anxiety, depression and insomnia symptoms. Because of the epidemic, a large number of people reduced interpersonal communication or even observed complete isolation. Isolation and lack of interpersonal communication can have a significant impact on mental health. Reiter et al. [44] suggested that half of solitary incarcerated people had symptoms of anxiety and depression, a rate significantly higher than that among general prison populations. A meta-analysis conducted by Purssell et al. showed that isolated patients had higher levels of anxiety and depression than nonisolated patients [45]. Another study of patients infected with MERS obtained similar conclusions [46]. In this study, confirmed patients, patients suspected of infection, or others formally isolated by the administration did not present significant differences from other participants in anxiety, depression or insomnia symptoms, and these participants had a higher rate of experiencing psychological intervention than the others. It also should be noted that, as Chinese government adapted strict long-term isolation and observation of close contacts of patients, most of the people who lost their loved ones from COVID-19 were identified as close contacts in the present study. People with loved ones who contracted or died from COVID-19 has been reported to significantly contribute to pandemic stress and psychological symptoms, which should receive timely interventions [42, 43]. In contrast, a large number of participants with psychological problems were noncontacts of confirmed patients, which was not reported in previous studies [6, 13]. For participants indicating epidemic status E6 (i.e., noncontacts), having experienced no psychological intervention and having engaged in outside activity once in ≥ 30 days were risk factors for depression (OR = 2.128; OR = 1.916). These self-isolated noncontacts had a lower rate of psychological interventions and a higher rate of psychological problems, which should be considered.
For return-to-work status, off-site work resumption and no study resumption were found to have a higher proportion of psychological and sleep symptoms than other return-to-work statuses. Subgroup analyses of different return-to-work statuses showed that having an enterprise management job could be a risk factor for psychological problems across different return-to-work statuses. This observation may be related to the pressure of unstable economic status caused by the epidemic. During the return-to-work period, multiple factors may have different complex effects on people with different return-to-work statuses. Targeted psychological interventions should focus not only on those resuming on-site work but also on those engaging in off-site work or not back to work, and individualized interventions should be conducted.
Limitations
First, because of the restriction on cross-regional outside activities during the survey time, probability sampling was not available. Nonprobability sampling may have inherent limitations in accurately representing the entire population. Therefore, the authors adopted a population-based stratification and quota sampling method to improve the overall representation. Second, although we used the snowball sampling method to recruit hard-to-find samples, due to strict isolation, some sample sizes might be small (e.g., cured and confirmed patients), which could limit the representation of these groups. Third, due to cultural restriction and epidemic concerns, whether people had loved ones who contracted or died from COVID-19 were not asked in this study. The bereavement of COVID-19 could be a significant contributor to pandemic stress and psychological symptoms, which might confound the findings of the present study. We analyzed the rates of COVID-19 diagnosis/deaths in different regions of China and did not find statistically significant difference, indicating possibly limited influence on this study. However, this factor deserves further exploration when available. Finally, selection bias was inevitable because of the hybrid nonrandom resampling and dropout cases. A study with random sampling should be carried out when possible. Additionally, a follow-up study can better analyze the changes in the prevalence and severity of psychological symptoms, which might be a further direction for this topic.
Conclusions
This study suggested that 18.3 14.9, and 17.9% of the participants had anxiety, depression, and insomnia symptoms, respectively, and 2.2–2.7% had severe problems. Engaging in outside activity once in ≥ 30 days (OR = 2.719, OR = 2.074, OR = 2.225) and age 50–64 years (OR = 2.431, OR = 1.936, OR = 2.036) were common risk factors for anxiety, depression and insomnia symptoms. Living in Hubei Province (OR = 1.304, OR = 1.242) was a common risk factor for anxiety and insomnia symptoms. Working as frontline medical staff (OR = 2.150) was another risk factor for anxiety symptoms. These high-risk populations should receive timely assistance in psychological health. The health education rate reached 98.9%, and 45.0% of the participants had received targeted education. However, the psychological intervention rate was only 16.2%, and 2.5% of the participants received target interventions, which is not sufficient. Efforts should be made to strengthen interventions for populations with a high risk of psychological and sleep symptoms.
Availability of data and material
The data that support the findings of this study are included in the article/supplementary material.
Abbreviations
- GAD-7:
-
Generalized anxiety disorder-7 scale
- PHQ-9:
-
Patient health questionnaire-9
- ISI:
-
Insomnia severity index
- EVD:
-
Ebola virus disease
- COVID-19:
-
Coronavirus disease 2019
- SARS:
-
Severe acute respiratory syndrome
- MERS:
-
Middle East respiratory syndrome
- H1N1:
-
H1N1 flu
- NEPD:
-
National economic population division
- DNC:
-
Daily number of new cases
References
Kelly JD, Hoff NA, Spencer D, Musene K, Bramble MS, McIlwain D, Okitundu D, Porco TC, Rutherford GW, Glymour MM, Bjornson Z, Mukadi P, Okitolonda-Wemakoy E, Nolan GP, Muyembe-Tamfum JJ, Rimoin AW (2019) Neurological, cognitive, and psychological findings among survivors of ebola virus disease from the 1995 Ebola Outbreak in Kikwit, Democratic Republic of Congo: a cross-sectional study. Clin Infect Dis 68(8):1388–1393. https://doi.org/10.1093/cid/ciy677
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF (2019) Tan W (2020) A novel coronavirus from patients with pneumonia in China. N Engl J Med 382(8):727–733. https://doi.org/10.1056/NEJMoa2001017
Ghinai I, McPherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K, Rubin R, Morales-Estrada S, Black SR, Pacilli M, Fricchione MJ, Chugh RK, Walblay KA, Ahmed NS, Stoecker WC, Hasan NF, Burdsall DP, Reese HE, Wallace M, Wang C, Moeller D, Korpics J, Novosad SA, Benowitz I, Jacobs MW, Dasari VS, Patel MT, Kauerauf J, Charles EM, Ezike NO, Chu V, Midgley CM, Rolfes MA, Gerber SI, Lu X, Lindstrom S, Verani JR, Layden JE (2020) First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. https://doi.org/10.1016/s0140-6736(20)30607-3
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W (2020) Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395(10224):565–574. https://doi.org/10.1016/s0140-6736(20)30251-8
National-Health-Committee-of-the-People's-Republic-of-China (2020) Notification on strengthening community prevention and control of new coronavirus infection (in Chinese). http://www.nhc.gov.cn/xcs/zhengcwj/202001/dd1e502534004a8d88b6a10f329a3369.shtml. Accessed 9 Feb 2020
Wang S, Zhang Y, Ding W, Meng Y, Hu H, Liu Z, Zeng X, Wang M (2020) Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. Eur Psychiatry 63(1):e77. https://doi.org/10.1192/j.eurpsy.2020.78
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17051729
Liu X, Luo WT, Li Y, Li CN, Hong ZS, Chen HL, Xiao F, Xia JY (2020) Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect Dis Poverty 9(1):58. https://doi.org/10.1186/s40249-020-00678-3
Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, Gong YM, Yuan K, Yan W, Sun YK, Shi J, Bao YP, Lu L (2020) Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open 3(7):e2014053. https://doi.org/10.1001/jamanetworkopen.2020.14053
Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, Cheung T, Xiang YT (2020) Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci 16(10):1732–1738. https://doi.org/10.7150/ijbs.45120
State-Council-of-People's-Republic-of-China (2020) Notification of prevention and control measures for resuming production in enterprises and institutions (in Chinese). http://www.gov.cn/gongbao/content/2020/content_5488911.htm. Accessed 22 Feb 2020
National-Health-Committee-of-the-People’s-Republic-of-China (2020) Update on the epidemic situation of novel coronavirus pneumonia at 24:00 on February 22 (in Chinese). http://www.nhc.gov.cn/xcs/yqtb/202002/07e5b22758364f2482d83537ef3975d2.shtml. Accessed 22 Feb 2020
Zhang Y, Wang S, Ding W, Meng Y, Hu H, Liu Z, Zeng X, Guan Y, Wang M (2020) Status and influential factors of anxiety depression and insomnia symptoms in the work resumption period of COVID-19 epidemic: a multicenter cross-sectional study. J Psychosom Res 138:110253. https://doi.org/10.1016/j.jpsychores.2020.110253
Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, Zhao X, Zou Y, Hu Y, Luo X, Zhang Z, Lai A, Ho R, Tran B, Ho C, Tam W (2020) Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun 87:84–92. https://doi.org/10.1016/j.bbi.2020.04.055
Li S, Wang Y, Xue J, Zhao N, Zhu T (2020) The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17062032
Zhu Z, Liu Q, Jiang X, Manandhar U, Luo Z, Zheng X, Li Y, Xie J, Zhang B (2020) The psychological status of people affected by the COVID-19 outbreak in China. J Psychiatr Res 129:1–7. https://doi.org/10.1016/j.jpsychires.2020.05.026
Moyer DN, Connelly KJ, Holley AL (2019) Using the PHQ-9 and GAD-7 to screen for acute distress in transgender youth: findings from a pediatric endocrinology clinic. J Pediatr Endocrinol Metab 32(1):71–74. https://doi.org/10.1515/jpem-2018-0408
He XY, Li C, Qian J, Cui HS, Wu WY (2010) Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch Psychiatry 22:200–203. https://doi.org/10.3969/j.issn.1002-0829.2010.04.002
Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, Zhang G, Zhou Q, Zhao M (2014) Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry 36(5):539–544. https://doi.org/10.1016/j.genhosppsych.2014.05.021
Chen S, Fang Y, Chiu H, Fan H, Jin T, Conwell Y (2013) Validation of the nine-item patient health questionnaire to screen for major depression in a Chinese primary care population. Asia Pac Psychiatry 5(2):61–68. https://doi.org/10.1111/appy.12063
Chung KF, Kan KK, Yeung WF (2011) Assessing insomnia in adolescents: comparison of Insomnia Severity Index, Athens Insomnia Scale and sleep quality index. Sleep Med 12(5):463–470. https://doi.org/10.1016/j.sleep.2010.09.019
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S (2020) Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 3(3):e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976
National-Bureau-of-Statistics-of-People's-Republic-of-China (2011) Center, west, east and northeast division standard (in Chinese). http://www.stats.gov.cn/ztjc/zthd/sjtjr/dejtjkfr/tjkp/201106/t20110613_71947.htm. Accessed 22 Feb 2020
Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, Rockhill C, Katon W (2010) Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics 126(6):1117–1123. https://doi.org/10.1542/peds.2010-0852
National-Bureau-of-Statistics-of-People's-Republic-of-China (2010) Summary data of the Sixth National Census (in Chinese). http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm. Accessed 9 Feb 2020
Mohammed A, Sheikh TL, Gidado S, Poggensee G, Nguku P, Olayinka A, Ohuabunwo C, Waziri N, Shuaib F, Adeyemi J, Uzoma O, Ahmed A, Doherty F, Nyanti SB, Nzuki CK, Nasidi A, Oyemakinde A, Oguntimehin O, Abdus-Salam IA, Obiako RO (2015) An evaluation of psychological distress and social support of survivors and contacts of Ebola virus disease infection and their relatives in Lagos, Nigeria: a cross sectional study–2014. BMC Public Health 15:824. https://doi.org/10.1186/s12889-015-2167-6
Zhan Y, Chen R, Zhang F, Wang J, Sun Y, Ding R, Hu D, Yu J (2014) Insomnia and its association with hypertension in a community-based population in China: a cross-sectional study. Heart Asia 6(1):88–93. https://doi.org/10.1136/heartasia-2013-010440
Gupta S, Goren A, Dong P, Liu D (2016) Prevalence, awareness, and burden of major depressive disorder in urban China. Expert Rev Pharmacoecon Outcomes Res 16(3):393–407. https://doi.org/10.1586/14737167.2016.1102062
Zhou X, Bi B, Zheng L, Li Z, Yang H, Song H, Sun Y (2014) The prevalence and risk factors for depression symptoms in a rural Chinese sample population. PLoS ONE 9(6):e99692. https://doi.org/10.1371/journal.pone.0099692
Yu W, Singh SS, Calhoun S, Zhang H, Zhao X, Yang F (2018) Generalized anxiety disorder in urban China: prevalence, awareness, and disease burden. J Affect Disord 234:89–96. https://doi.org/10.1016/j.jad.2018.02.012
Wu M, Han H, Lin T, Chen M, Wu J, Du X, Su G, Wu D, Chen F, Zhang Q, Zhou H, Huang D, Wu B, Wu J, Lai T (2020) Prevalence and risk factors of mental distress in China during the outbreak of COVID-19: a national cross-sectional survey. Brain Behav. https://doi.org/10.1002/brb3.1818
Klemm C, Hartmann T, Das E (2019) Fear-mongering or fact-driven? illuminating the interplay of objective risk and emotion-evoking form in the response to epidemic news. Health Commun 34(1):74–83. https://doi.org/10.1080/10410236.2017.1384429
Chan SS, So WK, Wong DC, Lee AC, Tiwari A (2007) Improving older adults’ knowledge and practice of preventive measures through a telephone health education during the SARS epidemic in Hong Kong: a pilot study. Int J Nurs Stud 44(7):1120–1127. https://doi.org/10.1016/j.ijnurstu.2006.04.019
Berry N, Lobban F, Emsley R, Bucci S (2016) Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: a systematic review. J Med Internet Res 18(5):e121. https://doi.org/10.2196/jmir.5250
Cipolletta S, Mocellin D (2018) Online counseling: an exploratory survey of Italian psychologists’ attitudes towards new ways of interaction. Psychother Res 28(6):909–924. https://doi.org/10.1080/10503307.2016.1259533
Hammond GC, Croudace TJ, Radhakrishnan M, Lafortune L, Watson A, McMillan-Shields F, Jones PB (2012) Comparative effectiveness of cognitive therapies delivered face-to-face or over the telephone: an observational study using propensity methods. PLoS ONE 7(9):e42916. https://doi.org/10.1371/journal.pone.0042916
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Li M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JTK, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z (2020) Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. https://doi.org/10.1056/NEJMoa2001316
Wuhan-People's-Government (2020) Disease Prevention and Control Notification of New Coronavirus Infection (in Chinese). http://www.wuhan.gov.cn/hbgovinfo/zwgk_8265/tzgg/202001/t20200123_304065.html. Accessed 9 Feb 2020
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, Yu Y, Kou C, Xu X, Lu J, Wang Z, He S, Xu Y, He Y, Li T, Guo W, Tian H, Xu G, Xu X, Ma Y, Wang L, Wang L, Yan Y, Wang B, Xiao S, Zhou L, Li L, Tan L, Zhang T, Ma C, Li Q, Ding H, Geng H, Jia F, Shi J, Wang S, Zhang N, Du X, Du X, Wu Y (2019) Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 6(3):211–224. https://doi.org/10.1016/s2215-0366(18)30511-x
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223):507–513. https://doi.org/10.1016/s0140-6736(20)30211-7
Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, Liu X, Fuller CJ, Susser E, Lu J, Hoven CW (2009) The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 54(5):302–311. https://doi.org/10.1177/070674370905400504
Dutheil F, Mondillon L, Navel V (2020) PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol Med. https://doi.org/10.1017/s0033291720001336
Morris SE, Moment A, Thomas JD (2020) Caring for bereaved family members during the COVID-19 pandemic: before and after the death of a patient. J Pain Symptom Manage 60(2):e70–e74. https://doi.org/10.1016/j.jpainsymman.2020.05.002
Reiter K, Ventura J, Lovell D, Augustine D, Barragan M, Blair T, Chesnut K, Dashtgard P, Gonzalez G, Pifer N, Strong J (2020) Psychological distress in solitary confinement: symptoms, severity, and prevalence in the United States, 2017–2018. Am J Public Health 110(S1):S56-s62. https://doi.org/10.2105/ajph.2019.305375
Purssell E, Gould D, Chudleigh J (2020) Impact of isolation on hospitalised patients who are infectious: systematic review with meta-analysis. BMJ Open 10(2):e030371. https://doi.org/10.1136/bmjopen-2019-030371
Kim HC, Yoo SY, Lee BH, Lee SH, Shin HS (2018) Psychiatric findings in suspected and confirmed middle east respiratory syndrome patients quarantined in hospital: a retrospective chart analysis. Psychiatry Investig 15(4):355–360. https://doi.org/10.30773/pi.2017.10.25.1
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Collecting data: SW, YZ, WD, YM, HH, ZL, XZ, YG, MW. Statistical analysis: SW, YZ, MW. Preparing manuscript: SW, YZ, WD, YM, YG. Revision manuscript: SW, YZ, WD, YM, HH, ZL, XZ, YG, MW. Supervision: MW.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
Because of the restriction on face-to-face communications and outside activities during the epidemic, the study required all participants or their guardians to provide informed consent by reading an online consent form and clicking an “agree to the consent” button for the online questionnaire or by offering oral consent before a telephone review. This study was reviewed, approved, and supervised by the ethics committee of SanBo Brain Hospital, Capital Medical University. All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, S., Zhang, Y., Guan, Y. et al. A nationwide evaluation of the prevalence of and risk factors associated with anxiety, depression and insomnia symptoms during the return-to-work period of coronavirus disease 2019 in China. Soc Psychiatry Psychiatr Epidemiol 56, 2275–2286 (2021). https://doi.org/10.1007/s00127-021-02046-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-021-02046-4