Abstract
Purpose
This study of Australian and Dutch people with anxiety or depressive disorder aims to examine people’s perceived needs and barriers to care, and to identify possible similarities and differences.
Methods
Data from the Australian National Survey of Mental Health and Well-Being and the Netherlands Study of Depression and Anxiety were combined into one data set. The Perceived Need for Care Questionnaire was taken in both studies. Logistic regression analyses were performed to check if similarities or differences between Australia and the Netherlands could be observed.
Results
In both countries, a large proportion had unfulfilled needs and self-reliance was the most frequently named barrier to receive care. People from the Australian sample (N = 372) were more likely to perceive a need for medication (OR 1.8; 95% CI 1.3–2.5), counselling (OR 1.4; 95% CI 1.0–2.0) and practical support (OR 1.8; 95% CI 1.2–2.7), and people’s overall needs in Australia were more often fully met compared with those of the Dutch sample (N = 610). Australians were more often pessimistic about the helpfulness of medication (OR 3.8; 95% CI 1.4–10.7) and skills training (OR 3.0; 95% CI 1.1–8.2) and reported more often financial barriers for not having received (enough) information (OR 2.4; 95% CI 1.1–5.5) or counselling (OR 5.9; 95% CI 2.9–11.9).
Conclusions
In both countries, the vast majority of mental health care needs are not fulfilled. Solutions could be found in improving professionals’ skills or better collaboration. Possible explanations for the found differences in perceived need and barriers to care are discussed; these illustrate the value of examining perceived need across nations and suggest substantial commonalities of experience across the two countries.
Similar content being viewed by others
Introduction
Depressive and anxiety disorders are the most common and disabling mental health problems in modern society. In the Netherlands, 7.6 and 12.4% of the adult population suffered from depressive or anxiety disorders in the last 12 months [4], while in Australia these numbers were 6.6 and 5.6%, respectively [2]. Despite the fact that effective treatments are available for depressive and anxiety disorders, the actual use of care for these common mental disorders is low and many people fail to receive treatment meeting minimal standards for adequacy, even in economically advantaged countries such as the Netherlands and Australia [2, 4, 41].
To understand why service use is so low, more knowledge should be obtained about people’s perceived needs and barriers to receive care. The European Study of the Epidemiology of Mental Disorders (ESEMeD) has recently estimated the level of unmet need for mental health care. However, in this study, need was defined as having a 12-month mental disorder which was disabling or had led to use of health services in the year prior to the interview [1]. In our view, diagnosis and need for treatment are not the same. Perceived need and barriers to care, as measured from the patient’s perspective, have not been studied very often, except in Australia and the Netherlands [23, 24, 30]. Some earlier studies examined the perceived barriers to care for mental health problems from a physician’s [15, 28], an adolescent’s [6] or migrants’ point of view [11]. One study about mental health services in Chile [33] differentiated between direct (lack of available services, not knowing where to go for help) and indirect (belief that problem will solve on its own, negative beliefs about helpfulness of services) barriers to care. A Canadian study [40] showed that perceived barriers due to acceptability were more prevalent than barriers due to accessibility and availability. A cross-national comparison study about reasons for not seeking care for a mental health problem in Canada, United States and the Netherlands [34] concluded that the two most frequently endorsed reasons were “I wanted to solve the problem on my own” and “I thought that the problem would get better by itself”. Comparisons with newly derived data are difficult since, in these studies, no specific instrument was used to measure barriers to care.
Meadows and colleagues [25] designed the Perceived Need for Care Questionnaire (PNCQ) for the Australian National Survey of Mental Health and Well-Being (NSMHWB), which is to our knowledge the first and only validated instrument that measures people’s perceptions of service needs for mental health problems and barriers to receive care. In 1997 and 2007, the Australian NSMHWB used this questionnaire in a population-wide sample. From 2004, it was also used in the Netherlands Study of Depression and Anxiety (NESDA), a longitudinal study about depressive and anxiety disorders [29].
A cross-national comparison between Australia and the Netherlands could provide unique information on perceived care needs and barriers to mental health care, since this has never been measured by the same (validated) instrument in two different countries before. Combining these two data sets (NSMHWB and NESDA) will give us the opportunity to study a large sample of people with specific DSM-IV diagnoses. Specific characteristics of the health care system in Australia and the Netherlands might give explanations for possible differences and similarities between the two countries. In this study, the following research questions will be addressed:
-
1.
What perceived needs for care do people with a current anxiety or depressive disorder have in Australia and in the Netherlands, and what similarities and differences can be observed?
-
2.
If there is any perceived need for care, are people’s perceived need for care in Australia more often or less often fully met compared with people’s perceived need for care in the Netherlands?
-
3.
What barriers to care do people with perceived unmet or partially met need experience, and what similarities and differences can be observed between Australia and the Netherlands?
Comparing Australia and the Netherlands
The Netherlands and Australia are both high income group countries (based on World bank 2004 criteria) and show comparable numbers with respect to gross national income (GNI) per capita, life expectancy at birth, and health expenditure per capita [42, 43]. Both countries have formulated a mental health policy that includes advocacy, promotion, prevention, treatment and rehabilitation. The care provided is demand-driven and aiming to assure the rights of people with mental disorders [42]. Mental health is part of the primary health care system in both countries, and general practitioners (GPs) provide the bulk of medical care; they are the first point of medical contact, and act as gatekeepers to the rest of the health care system.
Apart from these similarities, the two countries have health care systems that differ and could be divided into two broad categories. The Australian health care system has many similarities with a National Health Services (NHS) system, and the Dutch health care system mainly fits criteria for a Social Security (based) Health care (SSH) system. A NHS system is funded by means of general taxation and is strongly influenced by the state, while a SSH system is funded by means of earmarked premiums, has less state influence but strong influence from health care providers and (social) insurers [44]. A complexity of the Australian system is that the State and Federally funded systems employ different funding models and the Federal route allows co-payment. Nevertheless, as in an NHS system, the influence of Government on entitlements is strong.
For many years, the Netherlands had a fragmented system of health insurance, with compulsory social health insurance for people with an income below a certain ceiling point, and a voluntary private health insurance section for people with a higher income [13]. From the 1 January 2006, a single statutory insurance regime was introduced, which covers all residents of the Netherlands. All residents have a legal obligation to take out health insurance, for which they have to pay, and everybody has the option of taking out supplementary insurance [26]. As a result of the reform, price competition between health insurers became very fierce, there was more transparency for consumers, and 20% of all consumers changed to another health insurer [13]. As measured in 2005 and 2008, approximately 99% of Dutch citizens had taken out their (basic) health insurance, which covers GP care, primary care psychological care, and more specialized services (for which a referral from a GP is needed) [8, 26].
Though the Australian health system is built on the British model, it has evolved into something of a hybrid system. An Australian federal insurance provision is known as Medicare [22]. Medicare provides tax funded health care insurance which covers much of the cost of care to the user. Most medical services are provided by private GPs and specialists on a fee for service basis that is indemnified by Medicare. However, the funded items have been predominantly medical ones. So, while GPs and psychiatrists have provided psychological treatments (which were covered), care from psychologists through this route was limited. Services funded through Australian states are free to the user—in mental health these typically have developed with continuity from psychiatric hospital establishments now with considerable community care activity, and a concentration on care of people with low prevalence disorders of high impact such as typically schizophrenia and bipolar disorder. Some funding for psychological services has been made progressively available with capped funding introduced for some services from 2002, and then more free availability of fee for service reimbursement since late 2006. Next to Medicare, Australia has also a significant private sector, with around 30% of the population having a private health insurance [22].
While keeping this information about Australia and the Netherlands in mind, we aim to examine people’s perceived needs and barriers to care, and to identify similarities and differences in the two countries.
Methods
This study involved secondary data analyses of two national surveys: NESDA [29] and the Australian NSMHWB [36]. Both NESDA and NSMHWB used comparable methodology for the assessment of mental disorders, general disability, and comparable questions were asked about service use and perceived need for mental health treatment. The data were collected around the same time.
The Dutch study
NESDA is a multisite naturalistic cohort study following 2,981 participants aged 18 through 65 years over 8 years. This sample consists of 1,701 persons with a current (6-month recency) diagnosis of depressive and/or anxiety disorder (except for obsessive compulsive disorder and post-traumatic stress disorder), 907 persons with lifetime diagnoses or at risk because of a family history or subthreshold symptoms, and 373 healthy controls [29]. The survey aims to examine the course of depressive and anxiety disorders and their combined presence. For the current study, we did not consider respondents recruited through specialized mental care settings, but used the primary care sample (i.e., the participants who were recruited through general practices). People were selected via a three-stage screening procedure between 2004 and 2007.
First, patients who attended their GP in the last 4 months, irrespective of the reason for consultation, were sent a screening questionnaire containing the Kessler-10 (K-10), and five additional questions asking for the presence (yes/no) of anxiety symptoms to measure the presence of depressive or anxiety disorders [19]. Second, patients with a K-10 score of 20 or higher or a positive score on any of the additional anxiety questions were interviewed by phone with the short form of the Composite Interview Diagnostic Instrument (CIDI). Third, patients who fulfilled the CIDI short-form criteria for a current depressive or anxiety disorder were invited for a baseline assessment, including a full CIDI (version 2.1) interview, conducted by trained clinical research staff. Ultimately, 743 patients fulfilled CIDI and DSM-IV criteria for a current depressive [major depressive disorder (MDD), dysthymia] or anxiety disorder [generalized anxiety disorder, social phobia, panic disorder, agoraphobia]. Patients with a primary diagnosis of psychotic disorder, bipolar disorder, obsessive compulsive disorder, post-traumatic stress disorder or severe addiction disorder were excluded since the course trajectory can be strongly affected by these disorders. A second exclusion criterion of NESDA was lack of fluency in Dutch since language problems would harm the validity and reliability of collected data. Of the 23,750 persons who were sent a screening questionnaire, 10,706 (45%) returned it. Women and older people were more likely to return the screener and participate in NESDA, but there were no differences in psychopathology between responders and non-responders [29, 39]. Nearly half (4,592) of the screeners returned were screen positive and the individuals concerned were interviewed by phone. Since 1,172 persons refused and 425 could not be contacted anymore, finally 2,995 persons were actually interviewed by phone. Of the 1,162 phone screen positives, 264 refused to participate in NESDA. Further details about the recruitment flow of NESDA respondents in the primary care sample can be found in Penninx et al. [29].
The Australian survey
The NSMHWB was commissioned by the Department of Health and Ageing and carried out by the Australian Bureau of Statistics (ABS) in 2007. Respondents were selected at random from a stratified, multistage area probability sample of private dwellings [36]. Data were collected on the person level and the household level, and (replicate) weights, based on age and other characteristics, were used to account for selection bias [3]. 14,805 persons aged 16–85 years who were usual residents of private dwellings across Australia were invited to complete a personal interview. Of these, 8,841 participated, representing a 60% response rate. Of the non-responses, about 88% refused (including 61% complete refusals and 27% were some information provided at household level) and 12% provided incomplete information or were non-contacts. A follow-up short-form interview was taken among non-responders in two metropolitan areas, which indicated the impact of non-response to be small at the aggregated level [36]. Participation was voluntary and not remunerated, and those who were not fluent in English were excluded. The NSMHWB collected data on the lifetime and 12-month prevalence of mental disorders, the disability associated with these disorders and what services, if any, people use [36]. The World Mental Health Survey Initiative version of the World Health Organization (WHO) CIDI 3.0 version was used at the baseline interview to produce diagnostic information on depressive, anxiety, and substance use disorders according to DSM-IV and ICD-10. Interviews were carried out by ABS interviewers with extensive prior experience in conducting household surveys, and CIDI interviewers had followed the official WMH-CIDI training program [36].
Health service use and perceived needs
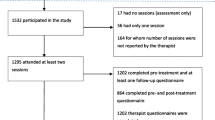
Health service use was measured in both surveys with the PNCQ. There were questions about whether people have had contact with a range of health professionals such as GPs, psychiatrists, psychologists, other (mental) health professionals (like mental health nurses and medical specialists). NESDA had collected this information about the past 6 months, while NSMHWB had measured it of the past 12 months. The PNCQ also assessed whether people had a perceived need for specific health care services and whether these needs were fully met, partially met or unmet. The categories of perceived need or possible services were: (1) information about mental illness, its treatment and available services; (2) medication; (3) counselling or psychotherapy to talk about causes of symptoms and learn to cope with emotional problems; (4) practical support or help to sort out housing and money problems; (5) skills training to improve one’s ability to work, or use one’s time in another way. Figure 1 presents the flow of the instrument in assessing perceived need.
Perceived barriers
If people reported to have a perceived unmet need or partially met need, they were asked about the reason(s) for not receiving (enough of) this specific service. Possible barriers to care were self-reliance (I’d rather solve it myself), pessimism (I thought it would not help), ignorance (I did not know where to get help), stigma (I was afraid of what others would think of me), finance (I could not afford the money), non-response (I asked for it but did not get any help), and alternative provision (I got help in another manner). The same questions were used in both Dutch and Australian studies.
Psychopathology
In Australia, the WMH-CIDI version 3.0 was used whereas in the Netherlands an earlier CIDI version 2.1 was used. The CIDI version 3.0 has a number of modifications from the CIDI 2.1 with the goal to improve problems with underreporting in the CIDI 2.1 [20]. Based on earlier studies, it seemed that CIDI 2.1 respondents quickly learn the logic of the stem-branch structure after a few sections and recognize that they can shorten the interview if they say no to the stem questions. Therefore, version 3.0 had included a screener in the beginning of the interview to alleviate the effects of learned responses [20]. Furthermore, in the Australian survey, respondents had to meet the CIDI 3.0 criteria for lifetime disorder before they were asked a subset of the diagnostic questions for 12-month (or less) recency. Therefore, the threshold for a diagnosis of 12 months (or less) would be somewhat lower with the CIDI 3.0 than with the CIDI 2.1. Studies that compared separately each of the CIDI versions 2.1 and 3.0 with the Structured Clinical Interview for DSM-IV (SCID) showed generally good individual level CIDI-SCID concordance for lifetime prevalence estimates of most disorders [5, 14]. The CIDI instrument has shown to be a valid and reliable instrument to detect depressive and anxiety disorders according to DSM-IV criteria.
Covariates
Since both surveys have collected a wide range of sociodemographic and clinical status data, we included age, gender, education level, type of diagnosis and disability as covariates in order to control for any differences within and between the two countries. Both surveys used the World Health Organization Disability Assessment Schedule (WHODAS) to assess general disability. NESDA used the WHODAS-II version that consists of 36 Likert formatted questions [9], while the NSMHWB used a shortened 12-item version [7]. The total scores of both WHODAS versions could range from 0 (no disability) to 100 (maximal impairment). Final WHODAS scores in NESDA could be calculated using two SPSS syntax versions (available through the WHO)—the 36 version if the person had a job, and the 32 version if people did not have a job (and work items were excluded). This latter version was used for the current study since the NSMHWB did not include items about work in their WHODAS total score.
Combining the two data sets
The most important difference between the two data sets was that the Australian one is a nationally representative sample of the Australian population, while the NESDA respondents were recruited from three different settings and thus are not representative to the Dutch general population. To make the two data sets as comparable as possible, we used NESDA’s primary care sample and included only people with a current anxiety (generalized anxiety disorder, social phobia, panic disorder, agoraphobia) or depressive disorder (MDD, dysthymia), those who completed the PNCQ, and those who had K-10 scores [19] of 20 or higher, since this was a selection criteria in the recruitment of the primary care sample in NESDA. The K-10 has proven screening qualities for affective disorders [12, 19]. Accordingly, a NSMHWB data set was created to fit the NESDA sample as well as possible, by making selections with regard to age (18–65 years), the presence of one of the above named DSM-IV disorders selected for NESDA with a 6-month recency, having had contact with a GP in the last year, and having K-10 scores of 20 or higher (see Fig. 2).
A model-based approach was used to compare the NSMHWB and NESDA data, and a pooled data set was created. Notwithstanding the methodological differences, these two national surveys are the best available recourses to study perceived need for care and barriers to care in people with anxiety and depressive disorders in the two countries.
Statistical analysis
First, descriptive statistics were used to outline the sociodemographic and clinical characteristics of the two selected samples. To compare the two samples on categorical data, cross-tabs with Pearson–Chi-square were used. Since the WHODAS and K-10 scores were not normally distributed, the non-parametric Mann–Whitney U test was used to compare the two countries.
In order to test the first research question, binary logistic regression analysis was performed on the total sample (N = 982) to compare people with any need for care (see light gray boxes in Fig. 2) with those who had no need for care, with country (Australia vs. the Netherlands) as the independent variable. Age, gender, education level, type of disorder and disability score (WHODAS) were added to the model as covariates. This analysis was also performed separately for each of the five needs for care (information, medication, counselling, practical support, and skills training).
To test the second research question, another binary logistic regression analysis was performed only on those people with any perceived need for care (N = 803) to compare people with a fully met need with those with partially or unmet need for care (see dark gray boxes in Fig. 2), with the same independent variable (country) and covariates. Again, this analysis was also performed separately for each of the five need categories named above.
Finally, in order to test the third research question, binary logistic regression analyses were performed on only those people with a partially met or unmet need to investigate whether each of the seven perceived barriers to care was different between the two countries. Again, the same control variables were used here. All analyses were performed using SPSS for Windows version 16.0 and P values were considered significant if ≤0.05.
Results
Table 1 shows the sociodemographic and clinical characteristics of the 610 people who were included in the Dutch sample and 372 people in the Australian sample. People in the Dutch sample were significantly more often in the oldest age group and were higher educated than the people in the Australian sample. There was no significant difference with regard to the sex distribution in the two samples. The Australian sample had significantly less people with a panic disorder but more with a social phobia compared to the Dutch sample, but there were no differences found for depressive disorders. The disability scores as measured by the WHODAS and K-10 differed significantly with higher mean scores in the Netherlands, and showed different distributions in the two countries. Both WHODAS (0.81 vs. 0.38) and K-10 (0.97 vs. 0.33) scores showed a more skewed distribution in Australia than the Netherlands, indicating that the Dutch sample contained more severely distressed and disabled people.
Service use
In both countries, two-thirds had used services for a mental health problem (64.1% in Neth and 65.3% in Aus). In the Netherlands, 22.6% had only seen a GP for their mental health problems in the past 6 months, while in Australia 20.7% had seen a GP only in the past 12 months. Nearly the same part of both samples had seen a GP and a mental health professional for their mental health problem (3.6% in Neth and 4.0% in Aus). Since we did not have information on the same time frames, real comparisons could not be made, but it seemed that service use was reported as about the same in the two countries although with different timeframes.
Perceived need: any need versus no need
Table 2 shows the percentages of any need for care, and the odds ratios (ORs) and confidence intervals (CIs) for six binary logistic regression models, with “any need” for care as the dependent variable (vs. “no need”) and country being the independent variable. The results indicate that people from both countries were most likely to feel a need for counselling followed by a need for information. People from Australia had higher chances of perceiving a need for medication, counselling and practical support than people from the Netherlands.
Perceived need: fully met need versus partially met need and unmet need
Of those people who had any need for care, only a minority had all their needs fully met (30.8% in Australia and 25.1% in the Netherlands), while the great majority had unmet or partially met care needs. When further analysing the people who had any need for care with a binary logistic model, with fully met need for care as the dependent variable (versus partially met need and unmet need taken together), Australians showed significantly higher chances of having fully met needs for medication, counselling and skills training (Table 3). People from both countries felt most often that their medication needs were fully met.
Perceived barriers
Australian and Dutch people gave multiple reasons for not having received (enough of) a certain service if they had perceived partially met or unmet care needs, but most often they wanted to solve the problem themselves (self-reliance; Table 4). The second most frequently named barrier for information, medication and counselling was pessimism. Ignorance was the most frequently named reason for not having received (enough of) practical support and the second most frequently named barrier for skills training.
The results from the logistic regression analyses on the seven barriers to care are shown in Table 5. People from Australia had significantly greater chances of being pessimistic about medication and skills training compared with those from the Netherlands. Australians were significantly more likely to experience stigma about skills training and to report more financial barriers for information and counselling than the Dutch people. Finally, Dutch people seemed to report more “alternative provisions” for getting counselling.
Discussion
Perceived need for treatment
Results of this comparison study between Australia and the Netherlands show that the extent to which people with anxiety or depressive disorder perceive a need for treatment is quite similar. Need for counselling and information is most frequently expressed in both countries, and the majority of people have unfulfilled care needs. This reveals that perceived needs of people with anxiety or depressive disorder are generally high and many needs stay partially met or unmet, which makes in worthwhile to further explore options to better reach patients’ needs.
However, people with anxiety or depressive disorder in Australia more often expressed any perceived need for medication, counselling and practical support as compared to Dutch people. Further, Australian people have their medication, counselling and skills training needs more often fully met. So, it seems that people in Australia seek and receive help more frequently for common mental disorders than their counterparts in the Netherlands, and more often feel to have received enough of it, especially for medication, counselling and skills training. Perhaps Australians have more knowledge about possible services or have better access to care. A literature review describes multiple “mental health literacy” initiatives in Australia but none in the Netherlands [18]. It might also be the case that Dutch people have a more critical attitude towards or higher expectation of mental health services available in the Netherlands, since that seemed the case in an earlier national comparison study [34] and in cancer patients [31].
Barriers to treatment
With regard to the barriers, both countries had similar percentages on self-reliance as an important reason for not receiving care, which was found before [34]. This might contribute to longer delays between onset of a mental disorder and initial contact with a (mental) health professional. (Online) Self-help services are freely available nowadays [27, 37], and might be used instead of the more “real-life” services by those who choose to deal with their mental illness alone [21].
There were also significant differences between perceived barriers to receive care in Australia and the Netherlands. Firstly, Australian people reported more financial barriers to receive information and counselling for their mental problems compared with the Dutch people, where none of the respondents had reported financial barriers for receiving medication. A recent survey of chronically ill patients (incl. depression) in Australia, Canada, France, Germany, the Netherlands, New Zealand, UK and the US found that Dutch patients were most protected against out-of-pocket costs, while Australia ranked in the middle [35]. So probably, people in Australia more often have to pay (extra) for mental health services while in the Netherlands the insurance system covers most, especially in case of medication and counselling. Still, Australians have most of their perceived needs more often fully met than the Dutch have. So, lack of finance might be a problem in some specific groups in Australia, but it does not prevent others of perceiving their needs being fully met.
Furthermore, Australian people were more likely to see stigma as a barrier to receive skills training and were more pessimistic about the helpfulness of medication and skill training when compared with the Dutch people. The Dutch, on the other hand, reported more often to see alternatives for their counselling needs. Possible explanations for these findings could be found in subtle national cultural differences. Hoftstede [16] studied cultural differences of people from over 50 countries around the world and found that people in Australia and the Netherlands have very similar attitudes about “power distance” (social inequality) and “individualism” (vs. collectivism). However, the countries differed markedly on the dimension “masculinity” (vs. femininity). The Netherlands were among the three most “feminine” countries, meaning that both men and women are supposed to be modest, tender, concerned with quality of life, and social gender roles overlap. Australia scored relatively high on masculinity, which means that social gender roles distinct more clearly and men are supposed to be more assertive, tough and focused on success than women [16]. Feelings of shame (stigma) and pessimism about treatment may fit the more “tough” (male) values of Australians while seeing alternatives may fit the more “tender” (female) values of the Dutch.
Now that we know what barriers prevent people to seek help for their anxiety or depressive symptoms, we should look for possible ways to overcome these barriers to care. Initiatives that aim to educate individuals about anxiety and depression, different treatment options and their effectiveness could be helpful. GPs could play a crucial role here.
Strengths and limitations
One important limitation is that the two studies used different ways for recruiting respondents, which should be kept in mind when interpreting the results. The use of different versions of the CIDI is also a limitation that should be mentioned. It is likely that people in the Australian sample had a slightly higher chance of having a diagnosis according to the WMH-CIDI because this latter CIDI version had a modified question flow, intended to promote episode recall and reduce opportunities to purposively influence the interview duration with strategies that would lead to false negatives [20, 38], and because respondents were only assessed for the presence of some 6-month symptoms of the disorder once they had met lifetime criteria for the disorder. Service use was assessed with different timeframes in the two surveys, with a longer timeframe in Australia and this cannot be excluded as a source of bias possibly making a contribution to the higher levels of need found in Australia. Consideration of recall bias effects would mean however that this effect is likely to be somewhat less than the proportional timeframe differences. For future work where cross-national comparison is a primary aim standardization of timeframes would be worthwhile. To overcome some of these limitations, we have made similar respondent selections based on certain CIDI diagnoses, 6-month recency and K-10 scores of 20 or higher, which increase comparability of respondents of both studies. Further, it could be that non-responders experienced greater or different barriers to care compared with responders, which might have influenced the results in both countries. This also counts for individuals with other diagnoses. Finally, we have no information about other perceived barriers such as time constrains, lack of trust in health care providers and accessibility. The most important strength is the use of the PNCQ in both studies, giving us the largest data set ever so far collected containing comparable information about perceived needs and barriers to care of people suffering from specific anxiety and depressive disorders and for the first time enabling some international comparisons.
Conclusion
The findings from this study suggest that, whatever the health care system characteristics, in both countries the vast majority of mental health care needs of people with common mental disorders are not fulfilled. Self-reliance and pessimism are the most important reasons for not having received (enough of) a certain service. So solutions for this problem should not be found in refinement of the organizational or financial arrangements, but for example in improvements in GP skills to provide counselling themselves or refer to other mental health care professionals or self-help-methods. At the same time, initiatives to inform and encourage people to seek help via their GP in case of anxiety or depressive symptoms might increase the amount of well-informed choices to either use mental health care services or not. A collaborative care model for treatment for anxiety and depression in the primary care setting could be helpful as well. The combination of allied health professionals, educational tools and follow-up sessions to monitor medication and cognitive behaviour therapy has been shown effective before [10, 17, 32]. Notwithstanding the differences in perceived barriers to care, Australian patients with anxiety or depressive disorder more often perceive their needs as being fully met than Dutch patients do. Further research is needed to unravel the exact mechanisms behind this.
References
Alonso J, Codony M, Kovess V, Angermeyer MC, Katz SJ, Haro JM et al (2007) Population level of unmet need for mental healthcare in Europe. Br J Psychiatry 190:299–306
Andrews G, Henderson S, Hall W (2001) Prevalence, comorbidity, disability and service utilization: overview of the Australian National mental Health Survey. Br J Psychiatry 178:145–153
Australian Bureau of Statistics (ABS) (2007) Technical manual: National Survey of Mental Health and Wellbeing, confidentialised unit record files. ABS, Australia
Bijl RV, Ravelli A (2000) Psychiatric morbidity, service use, and need for care in the general population: results of the Netherlands Mental Health Survey and Incidence Study. Am J Public Health 90:602–607
Booth BM, Kirchner JE, Hamilton G, Harrell R, Smith GR (1998) Diagnosing depression in the medically ill: validity of a lay-administered structured diagnostic interview. J Psychiatr Res 32:353–360
Boyd C, Francis K, Aisbett D, Newnham K, Sewell J, Dawes G et al (2007) Australian rural adolescents’ experiences of accessing psychological help for a mental health problem. Aust J Rural Health 15:196–200
Buist-Bouwman MA, Ormel J, de Graaf R, Vilagut G, Alonso J, van Sonderen E et al (2008) The ESEMeD/MHEDEA 2000 investigators. Psychometric properties of the World Health Organization Disability Assessment Schedule used in the European Study of the Epidemiology of Mental Disorders. Int J Methods Psychiatr Res 17:185–197
Centraal Bureau voor de Statistiek (CBS) [Statistics Netherlands] [Online] (cited 2009 June). Available from: http://www.cbs.nl/nl-NL/menu/themas/gezondheid-welzijn/cijfers/default.htm
Chwastiak LA, von Korff M (2003) Disability in depression and back pain: evaluation of the World Health Organization Disability Assessment Schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol 56:507–514
Craske MG, Roy-Byrne P, Stein MB, Donald-Shelbourne C, Bystritsky A, Katon W et al (2002) Treating panic disorder in primary care: a collaborative care intervention. Gen Hosp Psychiatry 24:148–155
Fassaert T, de Wit MAS, Tuinebreijer WC, Verhoeff AP, Beekman ATF, Dekker J (2008) Perceived need for mental health care among non-western labour immigrants. Soc Psychiatry Psychiatr Epidemiol 44(3):208–216
Furukawa TA, Kessler RC, Slade T, Andrews G (2003) The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med 33:357–362
Gress S, Manouguian M, Wasem J (2007) Health insurance reform in the Netherlands. CESifo DICE (Database for Institutional Comparisons Europe) Report 1, pp 63–67
Haro JM, Arbabzadeh-Bouchez S, Brugha TS et al (2006) Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health Surveys. Int J Methods Psychiatr Res 15:176–180
Henke RM, Chou AF, Chanin JC, Zides A, Hudson Scholle S (2008) Physician attitude toward depression care interventions: implications for implementation of quality improvement initiatives. Implic Sci 3:40
Hofstede G (1991) Cultures and organizations: software of the mind. McGraw-Hill Book Company, London
Katon W, Von Korff M, Lin E (1995) Collaborative management to achieve treatment guidelines: impact on depression in primary care. JAMA 273:1026–1031
Kelly CM, Jorm AF, Wright A (2007) Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. MJA 187:S26–S30
Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E et al (2003) Screening for serious mental illness in the general population. Arch Gen Psychiatry 60:184–189
Kessler RC, Üstün TB (2004) The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 13(2):93–121
Leach LS, Christensen H, Griffiths KM, Jorm AF, Mackinnon AJ (2007) Websites as a mode of delivering mental health information: perceptions from the Australian public. Soc Psychiatry Psychiatr Epidemiol 42(2):167–172
McDonald PJ (1998) The NHS’s 50th anniversary: a social experiment that keeps adapting. BMJ 317:55–56
Meadows G, Burgess P (2009) Perceived need for mental health care: findings from the 2007 Australian Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 43:624–634
Meadows G, Burgess P, Fossey E, Harvey C (2000) Perceived need for mental health care, findings from the Australian National Survey of Mental Health and Wellbeing. Psychol Med 30:645–656
Meadows G, Harvey C, Fossey E, Burgess P (2000) Assessing perceived need for mental health care in a community survey: development of the Perceived Need for Care Questionnaire (PNCQ). Soc Psychiatry Psychiatr Epidemiol 35:427–435
Ministry of Health, Welfare, and Sport (MinVWS) (2005) Health insurance in the Netherlands: the new health insurance system from 2006. MinVWS, The Hague, September 2005
Morgan AJ, Jorm AF (2009) Outcomes of self-help efforts in anxiety disorders. Expert Rev Pharmacoecon Outcomes Res 9(5):445–459
Nutting PA, Rost K, Dickinson M, Werner JJ, Dickinson P, Smith JL, Gallovic B (2002) Barriers to initiating depression treatment in primary care practice. J Gen Intern Med 17(2):103–111
Penninx BWJH, Beekman AT, Smit JH, Zitman FG, Nolen WA, Spinhoven P et al (2008) The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods. Int J Methods Psychiatr Res 17:121–140
Prins MA, Verhaak PFM, van der Meer K, Penninx BWJH, Bensing JM (2009) Primary care patients with anxiety and depression: need for care from the patient’s perspective. J Affect Disord 119:163–171
Reubsaet A, Lechner L, de Vries H (2006) The Dutch cancer information helpline: more critical patients after 10 years. Patient Educ Couns 63:215–222
Roy-Byrne PP, Craske MG, Stein MB, Sullivan G, Bystritsky A, Katon W et al (2005) A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry 62(3):290–298
Saldivia S, Vicente B, Kohn R, Rioseco P, Torres S (2004) Use of mental health services in Chile. Psychiatr Serv 55:71–76
Sareen J, Jagdeo A, Cox BJ, Clara I, ten Have M, Belik S-L et al (2007) Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatr Serv 58(3):357–364
Schoen C, Osborn R, How SKH, Doty MM, Peugh J (2008) In chronic condition: experiences of patients with complex health care needs, in eight countries, 2008. Health Aff 28(1):w1–w16
Slade T, Johnston A, Oakley Browne MA, Andrews G, Whiteford H (2009) 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Aust N Z J Psychiatry 43:594–605
Stjernswärd S, Ostman M (2006) Potential of e-health in relation to depression: short survey of previous research. J Psychiatr Ment Health Nurs 13(6):698–703
Tempier R, Meadows GN, Vasiliadis H, Mosier KE, Lesage A, Stiller A et al (2009) Mental disorders and mental health care in Canada and Australia: comparative epidemiological findings. Soc Psychiatry Psychiatr Epidemiol 44(1):63–72
Van der Veen WJ, van der Meer K, Penninx BW (2009) Screening for depression and anxiety: correlates of non-response and cohort attrition in the Netherlands study of depression and anxiety (NESDA). Int J Methods Psychiatr Res 18:229–239
Wang J (2006) Perceived barriers to mental health service use among individuals with mental disorders in the Canadian general population. Med Care 44(2):192–195
Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ et al (2007) Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 370:841–850
World Health Organization (WHO) (2005) Project atlas: resources for mental health and neurological disorders. Mental Health Atlas 2005 [Online] [cited 2009 June]. Available from: http://apps.who.int/globalatlas/predefinedReports/default.asp
World Health Organization (WHO) (2009) Statistics [Online] [cited 2009 June]. Available from: http://www.who.int/countries/nld/en/ and http://www.who.int/countries/aus/en/
Van der Zee J, Kroneman MW (2007) Bismarck or Beveridge: a beauty contest between dinosaurs. BMC Health Serv Res 7:94
Acknowledgments
The infrastructure for the NESDA study (http://www.nesda.nl) is funded through the Geestkracht program of the Netherlands Organisation for Health Research and Development (ZonMw, grant number 10-000-1002) and is supported by participating universities and mental health care organizations [VU University Medical Center, GGZ inGeest, Arkin, Leiden University Medical Center, GGZ Rivierduinen, University Medical Center Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Scientific Institute for Quality of Healthcare (IQ healthcare), Netherlands Institute for Health Services Research (NIVEL) and Netherlands Institute of Mental Health and Addiction (Trimbos)]. The 2007 NSMHWB was funded by the Australian Government Department of Health and Ageing, and conducted by the Australian Bureau of Statistics.
All authors would like to thank all those who participated in both studies and declare to have no conflict of interests.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Prins, M., Meadows, G., Bobevski, I. et al. Perceived need for mental health care and barriers to care in the Netherlands and Australia. Soc Psychiatry Psychiatr Epidemiol 46, 1033–1044 (2011). https://doi.org/10.1007/s00127-010-0266-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0266-3