Abstract
Aims/hypothesis
The effect of n-3 fatty acid treatment on vibration perception thresholds (VPTs) and cutaneous microvascular reactivity is not known. We tested whether: (1) a 15–18 month treatment with high dose (4 g/day) docosahexaenoic (DHA) plus eicosapentaenoic (EPA) acid improved VPT and microvascular reactivity in patients with non-alcoholic fatty liver disease; and (2) there are associations between VPT, microvascular reactivity and metabolic variables.
Methods
In the completed single centre, randomised, parallel group, placebo controlled Wessex Evaluation of fatty Liver and Cardiovascular markers in non-alcoholic fatty liver disease with OMacor thErapy (WELCOME) trial, we tested the effect of DHA+EPA on VPT at 125 Hz (big toe) and the cutaneous hyperaemic response (forearm) to arterial occlusion (ratio of maximum to resting blood flux [MF/RF]). Allocation and dispensing was carried out by an independent research pharmacist; all participants and research team members were blinded to group assignment.
Results
In all, 51 and 49 patients were randomised to placebo and DHA+EPA, respectively (mean age 51.4 years). Of these, 32 had type 2 diabetes. Forty-six (placebo) and 47 (DHA+EPA) patients completed the study; there were no important adverse (or unexpected) effects or side effects. In multivariable-adjusted regression models (intention-to-treat analyses), DHA+EPA treatment was associated with an increase in VPT (β coefficient 1.49 [95% CI 0.04, 2.94], p = 0.04). For VPT, the adjusted mean differences (95% CIs) in the placebo and DHA+EPA treatment groups were −0.725 (−1.71, 0.25) and 0.767 (−0.21, 1.75) m/s2, respectively. With DHA+EPA treatment, there was no change in MF/RF (β coefficient 0.07 [95% CI −0.56, 0.70], p = 0.84), the adjusted mean differences (95% CIs) in the placebo and DHA+EPA treatment groups were −0.549 (−1.03, −0.07) and −0.295 (−0.77, 0.18) respectively. VPT was independently associated with age (β coefficient 0.019 [95% CI 0.010, 0.029], p < 0.0001) and MF/RF (β coefficient −0.074 [95% CI −0.132, −0.016], p = 0.013), but not with diabetes (p = 0.38).
Conclusions/interpretation
High dose n-3 fatty acid treatment did not improve measures of microvascular function or vibration perception. Ageing and microvascular reactivity are associated with a measure of peripheral nerve function.
Trial registration: ClinicalTrials.gov NCT00760513
Funding: The study was funded by the National Institute for Health Research UK and Diabetes UK.
Similar content being viewed by others
Introduction
Peripheral neuropathy and impaired microvascular function are strong risk factors for foot ulceration and impaired wound healing in people with diabetes [1], and both somatic cutaneous sensory fibre neuropathy and microvascular dysfunction are early complications of diabetes mellitus and/or insulin resistance (IR) in obese individuals [2]. Screening tests for neuropathy in the clinic include use of a 10 g monofilament and of a 128 Hz tuning fork [3]. Both tests reflect the function of large myelinated sensory nerve fibres; however, although the monofilament test has been widely adopted and is easy to use in clinical practice, its sensitivity to detect early impairment in nerve function is limited [4]. In contrast, use of vibration perception thresholds (VPTs) allows not only detection of neuropathy but also assessment of the severity of the sensory nerve impairment [5]. The prevalence of an abnormal VPT in patients with type 2 diabetes has been shown to be >11% [6], and an abnormal VPT is an excellent predictor of foot ulceration, limb amputation and mortality in patients with type 2 diabetes [7].
Non-invasive assessment of cutaneous microvascular reactivity (MR) has been widely used to assess microvascular endothelial and neurovascular function in patients at an increased risk of cardiometabolic disease [8] and is indicative of MR in other vascular beds [9]. Impaired skin MR strongly relates to impaired glucose tolerance, IR and obesity [10, 11]; whilst microvascular and neurological function are interlinked in diabetes [12], there is still controversy about whether early changes in microvascular function or changes in metabolic variables have the greater influence on peripheral nerve function [13].
Treatment with high dose long chain n-3 polyunsaturated fatty acids such as eicosapentaenoic acid (EPA, 20:5 n-3) and docosahexaenoic acid (DHA, 22:6 n-3) improves endothelial function [14]. These fatty acids enhance nerve blood flow [15], may improve vibration perception and clinical symptoms of neuropathy in patients with type 2 diabetes [16], and have been shown to be protective against paclitaxel-induced peripheral neuropathy [17]. However, although there is some preliminary evidence of benefit of long chain n-3 fatty acids in patients with neuropathy, it remains uncertain whether these fatty acids have beneficial effects on VPTs and maximum flux (MF).
Patients with IR and non-alcoholic fatty liver disease (NAFLD) have an increased risk of type 2 diabetes and its complications, including macrovascular disease [18, 19]. Additionally, NAFLD is associated with impaired coronary microvascular function [20], increased risk of retinal microvascular disease and prevalence of peripheral neuropathy [21]. Since the effect of high dose n-3 fatty acid treatment on nerve function and microvascular function in high risk patients for type 2 diabetes and its complications is not known, we tested whether high dose n-3 fatty acid treatment has beneficial effects on VPTs and MF in this patient group. Specifically, we tested whether an 15–18 month treatment with high dose DHA+EPA (4 g/day as ethyl esters) produced improvements in VPTs and MR in patients with NAFLD, some of whom had type 2 diabetes; however, all patients were without clinical evidence of peripheral neuropathy or microvascular disease. In a pre-specified substudy of the Wessex Evaluation of fatty Liver and Cardiovascular markers in NAFLD with OMacor thErapy (WELCOME) trial (ClinicalTrials.gov registration no. NCT00760513) [22, 23], a randomised, double blind, placebo controlled trial, we tested the effect of DHA+EPA treatment on VPT and MR.
Methods
Study design
A cohort of 105 individuals (60 men and 45 women; mean age 51.4 years) was studied. The participants formed part of the WELCOME study, a randomised, double blind, placebo controlled trial [22] (approved by the local research ethics committee [REC: 08/H0502/165]). Participants were block randomised by an independent clinical trials pharmacist to treatment with identical capsules by mouth of either n-3 fatty acid ethyl esters (4 g/day Omacor; Pronova, Sandefjord, Norway) or placebo (4 g/day olive oil) for a minimum of 15 months and a maximum of 18 months. Only the clinical trials pharmacist was unblinded, and randomisation group allocation was concealed from all study members throughout the trial. One gram of Omacor contains 460 mg EPA and 380 mg DHA 380 mg as ethyl esters. Omacor is approved by the Food and Drug Administration and the European Medicines Agency at a dose of 2–4 g/day for the treatment of hypertriglyceridaemia. Olive oil placebo contained ~67% oleic acid, ~15% linoleic acid, ~15% palmitic acid. ~2% stearic acid and ~1% α-linolenic acid. Participants were unpaid and gave written informed consent. Inclusion criteria were a diagnosis of NAFLD based on liver biopsy or the presence of hepatic steatosis on ultrasound, and exclusion of other liver diseases. Participants were excluded from the final analyses if they had evidence of distal peripheral neuropathy in their feet (n = 4), as suggested by their failure to detect a 10 g monofilament [24], or if they had evidence of diabetic eye disease at retinal screening (n = 0).
All tests for peripheral neurological and microvascular function were conducted in a temperature controlled room (22–24°C). Skin temperature at the toe, if below 25°C, was raised with a heat pad to 25°C prior to vibration testing. Mean ± SD skin temperature measured at the toe was 28.3 ± 2.5°C (range 25.0–35.1°C) and at the forearm was 29.3 ± 0.7°C (range 27.5–31.1°C). Participants refrained from caffeine-containing drinks, smoking and exercise for ≥2 h prior to testing. Measurements were made at baseline and at the end of the study.
Vibrotactile perception
VPTs at 125 Hz were measured (Vibrotactile Perception Meter; HVLab Diagnostics Instruments, Southampton, UK) with a 6 mm diameter probe and a 2 mm gap to a 10 mm diameter surround [25]. VPTs were determined using the von Békésy method [25]. For this, the vibration magnitude was alternately increased and decreased by 3 dB/s according to whether the participant felt the vibration. A response button was pressed when the vibration was felt and released when the vibration was not felt. Measurements continued for 30 s or until a minimum of six pairs of reversals had been obtained, after excluding the first pair. Thresholds (m/s2) were determined from the arithmetic averages of the logarithms of the root mean square vibration acceleration at the reversals [26]. Tests were performed on the pulp of the left great toe at baseline and the end of the study. The intra-individual CV was 22% as measured in 20 volunteers on two occasions.
Microvascular function
Cutaneous MR was assessed on the ventral surface of the non-dominant forearm arm using laser Doppler fluximetry (Moor VMS LDF2 and DP1T probe; Moor Instruments, Axminster, UK) [27]. Blood flux was recorded continuously before and during the dilator response to transient ischaemia (180 mmHg for 3 min; MoorVMS-PRES). The post-occlusive hyperaemic response is an integrated vascular response involving neural, endothelial and vascular smooth muscle activity, and is analogous to that used to assess endothelial function in conduit arteries [8]. Values for microvascular perfusion in arbitrary perfusion units (PUs) were determined at rest (i.e. resting flux [RF]: mean value over the final 5 min before perturbation) and at maximum value after release of the pressure cuff (MF) using the manufacturer’s software (MoorVMS-PC software; Moor Instruments). MR was expressed as the ratio of maximum to resting blood flux (MF/RF). The intra-individual CV measured in the forearm of 10 volunteers on two occasions, 7 days apart, was 15% for the RF and 19% for the MF/RF.
Biochemical and anthropometric measurements
Measurements were made at baseline and at the end of the intervention period. Glucose, insulin, total cholesterol, HDL-cholesterol and triacylglycerol concentrations were measured in fasting serum or plasma using commercially available kits according to the manufacturers’ instructions. HbA1c was measured by high pressure liquid chromatography (Bio-Rad Laboratories, Irvine, CA, USA). HOMA-IR was calculated from fasting insulin and fasting glucose concentrations [28]. Blood pressure was measured in the non-dominant arm after participants had become acclimatised and had rested for at least 60 min; the mean of three measurements was calculated. Dual energy x-ray absorptiometry (DXA), MRI and magnetic resonance spectroscopy (MRS) were undertaken to assess body fat (total body fat, regional body fat and visceral fat) and quantify liver fat [22]. Liver fibrosis was assessed using the NAFLD fibrosis score [29] and an additional validated liver fibrosis score [30]. Carotid intima–media thickness (CIMT) was measured at both carotid arteries with B-mode ultrasound and a mean value was calculated. This measure is a recognised marker of subclinical atherosclerosis [31] and has prognostic value in cardiovascular disease [32]. The overall 10 year risk of cardiovascular disease was calculated using the QRISK 2011 online calculator (www.qrisk.org).
Statistical analysis
Statistical analyses were undertaken using IBM SPSS Statistics software (version 21.0, Chicago, IL, USA). Data are reported as the mean ± SD for normally distributed variables, or the median and interquartile range for non-normally distributed variables. Where possible, variables that were not normally distributed were normalised by log transformation for parametric statistical analyses. Pearson and Spearman rank r coefficients were used to investigate associations between normally and non-normally distributed variables, respectively. In all cases, a p value of <0.05 was taken to indicate significance.
We tested the independence of associations between baseline factors and the two primary outcomes (VPT and MF/RF) at baseline by multivariable linear regression. We tested the effects of DHA+EPA treatment on both key outcomes of interest (change in VPT at 125 Hz and change in MF/RF from baseline to the end of the study) using multivariable linear regression; and logistic regression for dichotomous outcomes of VPT difference (increased/decreased) and MF/RF (increased/decreased). ANCOVA was also used to assess adjusted mean differences (95% CIs) for both outcomes of interest in the placebo and DHA+EPA groups. These analyses included all participants with complete data (i.e. baseline and end of study measurements). For all regression models and for ANCOVA, there was also adjustment for baseline measurement of the outcome variable in question, and adjustment also for key covariates and confounders. We also explored the effect of medication usage (statins, metformin, antidepressants and antihypertensive drugs, including calcium antagonists; no patients were taking hydralazine).
Results
Characteristics of the trial participants
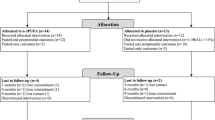
Figure 1 shows the CONSORT diagram for recruitment into the study and the reasons for withdrawal. Table 1 shows the baseline characteristics of participants without overt neuropathy or microvascular disease, stratified by diabetes status and by randomisation status. The mean ± SD age was 51.7 ± 10.9 years for the 69 individuals (38 men) without diabetes and 50.1 ± 10.3 years for the 32 individuals (20 men) with type 2 diabetes. Thirteen participants were current smokers and three had suffered from ischaemic heart disease. Of the participants, 41 were taking statins, 36 were taking antihypertensive drugs (nine calcium antagonists) and 27 were taking metformin. The VPT at 125 Hz and MF/RF did not differ between individuals with and without diabetes (Table 1). Of the participants without diabetes, ~50% had impaired fasting glucose or impaired glucose tolerance.
Associations of VPT at 125 Hz and MF/RF with cardiovascular and metabolic risk factors at baseline
In univariate analyses, VPT was associated with age (r = 0.507, p = 0.0001) and MF/RF (r = −0.301, p = 0.002; Table 2). The scatter plot for the association between VPT and MF/RF is shown in Fig. 2. The VPT was positively associated with CIMT (r = 0.358, p = 0.0001). An increase in VPT and a decline in MF/RF were both associated with an increase in QRISK (r = 0.416, p = 0.0001 and r = −0.229, p = 0.023, respectively).
There was no significant association between either VPT at 125 Hz or MF/RF and measures of obesity, glycaemic status or IR; however, in individuals without diabetes, MF/RF was negatively correlated with HOMA-IR (r = −0.326, p = 0.006, n = 69). Stratification by diabetes status suggested that in individuals with diabetes, an increase in VPT was associated with an increase in duration of diabetes (r = 0.485, p = 0.005).
A multivariable regression model with baseline VPT as the outcome variable, and age, sex, MF/RF, diabetes status, liver fibrosis score and CIMT as exposure variables, showed that all of these together explained ~35% of the variance in VPT (R 2 = 0.35, p < 0.001, adjusted R 2 = 0.30; Table 3). The use of statins, metformin, antidepressants or all antihypertensive drugs (including calcium antagonists) was not independently associated with VPT at 125 Hz. The model was also unaffected by adjustment for skin temperature (data not shown). We repeated the model replacing diabetes status with IR (HOMA-IR). In this model, age, sex, MF/RF, HOMA-IR, liver fibrosis score and CIMT explained ~33% of the variance in sensory nerve function (R 2 = 0.325, p = 0.0001, adjusted R 2 = 0.276) in the whole cohort.
We repeated the regression model, with VPT replacing MF/RF as the new outcome (in Table 3). In a model that included VPT, age, diabetes status, liver fibrosis score, use of calcium antagonists and CIMT as exposure variables, female sex (p = 0.010), VPT (p = 0.011) and use of calcium antagonists (p < 0.0001) were significant (R 2 = 0.27, adjusted R 2 = 0.21, p < 0.001). Use of other antihypertensive agents was not associated with MF/RF. Replacing diabetes status with HOMA-IR as an exposure variable did not improve the model (R 2 = 0.23, adjusted R 2 = 0.17, p = 0.003), and HOMA-IR was not independently associated with MF/RF (p = 0.97).
Effect of n-3 polyunsaturated fatty acid treatment on VPT at 125 Hz and MF/RF
Table 1 shows the baseline characteristics of those participants without overt neuropathy or microvascular disease, by randomisation status. By chance, VPT was higher in participants randomised to placebo compared with DHA+EPA at baseline; to take account of this difference, the regression models were adjusted for baseline measurement. Table 4 shows the results of multivariable regression modelling to test the effects of the DHA+EPA intervention on both outcomes (i.e. change in VPT or change in MF/RF). In regression modelling with adjusting for key potential confounders (age, sex, VPT at baseline, MF/RF, diabetes [yes/no], a liver fibrosis marker and mean CIMT), there was a small increase (i.e. worsening) in the VPT difference with DHA+EPA treatment. The model explained ~33% of the variance in VPT difference (R 2 = 0.33, p < 0.0001, adjusted R 2 = 0.27). The model was slightly improved when diabetes (yes/no) was replaced with HOMA-IR as a measure of IR (R 2 = 0.37, p < 0.0001, adjusted R 2 = 0.29). None of the medications tested affected the model or were associated with either outcome. Since there was a significant (and unexpected) effect of DHA+EPA in increasing VPT at the end of the study, we assessed adjusted mean differences in placebo and DHA+EPA treatment groups. The adjusted mean differences (95% CIs) in the placebo and DHA+EPA treatment groups were −0.725 (−1.71, 0.25) and 0.767 (−0.21, 1.75), respectively. These data are in keeping with the unstandardised β coefficient from the regression modelling analyses, showing the treatment effect (i.e. 1.492; Table 4). We also assessed the OR (95% CI) for a worsening of VPT difference with DHA+EPA treatment. These data (OR 2.47 [95% CI 0.97, 6.32], p = 0.058) were also consistent with the results from multivariable linear regression modelling and ANCOVA. Next, we tested whether there was an interaction between DHA+EPA treatment and the baseline VPT measurement. These analyses showed a significant association between the interaction term and change in VPT (Table 4).
We repeated the regression model with VPT difference replacing MF/RF difference as the outcome (Table 4). Variables included in the model explained 35% of the variance in MF/RF difference (R 2 = 0.35, p < 0.0001, adjusted R 2 = 0.28), but there was no effect of the DHA+EPA intervention (p = 0.84; Table 4). The adjusted mean differences (95% CIs) in the placebo and DHA+EPA treatment groups were −0.549 (−1.03, −0.07) and −0.295 (−0.77, 0.18) respectively. Figure 3 shows individual baseline and end of study measurements for VPT and MF/RF for each participant. Stratifying by diabetes status showed there was no specific benefit of DHA+EPA treatment on VPT (p = 0.36) or MF/RF (p = 0.53) in people with diabetes.
Effect of 15–18 month treatment with DHA+EPA ethyl esters (4 g/day) or placebo on cutaneous microvascular dilator capacity and VPT at 125 Hz. (a) and (c) show the placebo group and (b) and (d) show the treatment group. Baseline and end of study (End) median measurements for each group are indicated by a horizontal line
Discussion
Our study is the first randomised, double blind, placebo controlled trial to examine the effects of the highest licensed dose of n-3 fatty acids on measures of vibration perception and microvascular function. Our novel data show that there was no benefit of high dose DHA+EPA treatment for 15–18 months on VPT or MR. In fact, our results show that with DHA+EPA treatment there was a small, albeit significant, increase in VPT between baseline and the end of the study (Table 4) that is unlikely to be of clinical relevance. Although we show an independent association between VPT and MF/RF at baseline (Table 3), this association was weaker at the end of the study (data not shown). We consider that the change in association between these two variables (between baseline and end of study) may have been caused by two factors (illustrated in Table 4): (1) the significant interaction between DHA+EPA treatment and baseline VPT, and the association of both factors with the change in VPT during the study; and (2) the DHA+EPA treatment-mediated increase in the end of study VPT.
Whilst there is general agreement that microvascular and neurological function are interlinked in diabetes, there is still controversy over the pathogenesis of neuropathy and uncertainty as to whether metabolic or vascular risk factors (including impaired MR) are more important in influencing VPTs in people at risk of diabetic foot ulceration [13]. In addressing this uncertainty, our results suggest that ageing and early changes in microvascular function have a greater influence on peripheral nerve function than metabolic variables.
We do not have measurements of DHA or EPA tissue enrichment in nerves or the microvasculature. However, we have shown that the DHA+EPA treatment caused excellent enrichment in erythrocytes and there was good adherence to the intervention (all participants consumed ~75% of their allocated capsules) [23]. Whilst we did not undertake prior sample size calculations for this pre-specified substudy, our results provided no hint of improvement with the intervention (Table 4). A retrospective power calculation showed that with the number of patients completing the trial and α = 0.05, we had 99% power to detect a 20% change in MF/RF. Although, it has been previously suggested that a 6 week treatment with DHA had beneficial effects on forearm blood flow in obese individuals [14] and that n-3 fatty acid treatment (in a non-randomised study) improved vibration perception in 21 patients with type 2 diabetes [16], prior to our study these benefits of DHA+EPA had not been tested in randomised, double blind, placebo controlled trials lasting over 12 months.
Importantly, the association between VPT and MF/RF at baseline remained significant after adjusting for potential confounders such as age, sex, diabetes status, obesity, NAFLD severity or CIMT. In our study, stratifying by diabetes status showed that there was no association between VPT and IR (HOMA-IR) in people with diabetes. There was also no association between VPT and current glycaemic control (HbA1c), but there was a significant association between VPT and HOMA-IR in people who did not have diabetes (r = 0.342, p = 0.005; n = 67). This latter finding most likely reflects the fact that HOMA-IR measurements are an inaccurate estimate of IR in people with diabetes who have pancreatic beta cell failure. Our findings are also consistent with the results of a study of 156 individuals with peripheral neuropathy and diabetes, which showed no association between neuropathy and glycaemic control [12]. These findings and our data, taken together, suggest strongly that peripheral neurological function is more closely associated with a measure of microvascular health than with metabolic risk factors, with the exception of IR. Microvascular dysfunction has been proposed to be a link between obesity, IR and hypertension [33], and a reduced microvascular dilator and exchange capacity has consistently been reported by us and by others in individuals with features of the metabolic syndrome [34–37]. With respect to a link between VPT and HOMA-IR, it is important to note that the DHA+EPA intervention did not improve HOMA-IR (data not shown but available from the authors).
Peripheral neuropathy is associated with cardiovascular disease [38], and increased vibration thresholds have been shown to be a risk factor for mortality with diabetes [39]. We showed for the first time a strong association between VPT at 125 Hz and CIMT (Table 2). CIMT is a reliable marker of preclinical atherosclerosis, and NAFLD is an independent predictor of an increased CIMT [40]. Endothelial dysfunction may occur early in NAFLD [41] and it has been suggested that the mechanisms associated with arterial thickening could impair blood flow and initiate endoneurial hypoxia, which is thought to play a significant role in causing peripheral neuropathy in diabetes [42].
We are not able to explain what aspect of ageing underpins the association between age and VPT. Sensory perception decreases with age, and higher mechanical and thermal sensory perception thresholds have been observed in older people [43]; however, whether any decrease in perception occurs as a result of changes in the brain, spinal cord, or peripheral nerves or receptors is uncertain. Our finding that higher VPTs were associated with an increased duration of diabetes is consistent with results reported by Shun et al [44] in people with type 2 diabetes. These authors additionally reported that diabetes duration was negatively associated with epidermal denervation, an early event in people with diabetes [45]. It is plausible that IR and advanced protein glycation [46] combine with deleterious changes in nerve perfusion through components of inflammation and oxidative stress [47] and may be responsible for the increase in VPT, but this is speculation and further research is needed.
Limitations
The current study has strengths and limitations. The main strength is that we have undertaken a randomised, double blind, placebo controlled trial testing the effects of highly purified long chain n-3 fatty acids lasting 15–18 months. We cannot overlook the fact that perfusion of skin capillaries primarily serves the purpose of thermoregulation, whereas those in deeper tissues (e.g. skeletal muscle) are much more closely linked to metabolic demand; nevertheless, the ability to perform minimally invasive in vivo mechanistic studies in human skin can inform our understanding of how disease states adversely affect vascular function. There is no ideal biomarker for diagnosis of neuropathy in diabetes. We have used neurothesiometry (VPT) to derive a quantitative measurement of peripheral nerve function and VPT at 125 Hz that is neuroselective for large myelinated sensory nerve fibres. Recently, it has been shown that nerve dysfunction in large nerve fibres occurs in individuals with impaired glucose tolerance compared with health controls [48]. Dysfunction in small nerve fibres may precede large nerve fibre dysfunction in diabetic neuropathy [13, 49]. However, since we measured VPT, we cannot comment on the effect of DHA+EPA on small nerve fibre function or on the relationship between MR, ageing and HOMA-IR and small nerve fibre function. We also cannot be sure of the effect of duration of diabetes on VPT in our cohort because identification of the date of onset of type 2 diabetes is often imprecise. Additionally, we undertook assessment of VPT in the foot and microvascular function in the arm. It was technically challenging in this obese cohort to measure microvascular function in the lower leg, and it is well accepted that the cutaneous arm microcirculation provides a well-validated index of microvascular function indicative of MR in other, less accessible vascular beds [9, 50].
Conclusion
Treatment with the highest licensed dose of DHA+EPA (as Omacor/Lovaza) did not improve VPT or MR in patients with NAFLD. In a high risk patient group without evidence of overt peripheral neuropathy, both ageing and a measure of MR were independently associated with VPT. VPT is more strongly related to a measure of microvascular health than to metabolic risk factors, with the exception of IR.
Abbreviations
- CIMT:
-
Carotid intima–media thickness
- DXA:
-
Dual energy x-ray absorptiometry
- DHA:
-
Docosahexaenoic acid
- EPA:
-
Eicosapentaenoic acid
- IR:
-
Insulin resistance
- MF:
-
Maximum flux
- MR:
-
Microvascular reactivity
- MRS:
-
Magnetic resonance spectroscopy
- NAFLD:
-
Non-alcoholic fatty liver disease
- NIHR:
-
National Institute for Health Research
- PU:
-
Perfusion units (arbitrary)
- RF:
-
Resting flux
- VPT:
-
Vibration perception threshold
- WELCOME:
-
Wessex Evaluation of fatty Liver and Cardiovascular markers in NAFLD with OMacor thErapy
References
Abbott CA, Malik RA, van Ross ER, Kulkarni J, Boulton AJ (2011) Prevalence and characteristics of painful diabetic neuropathy in a large community-based diabetic population in the U.K. Diabetes Care 34:2220–2224
Herman RM, Brower JB, Stoddard DG et al (2007) Prevalence of somatic small fiber neuropathy in obesity. Int J Obes (Lond) 31:226–235
Tan LS (2010) The clinical use of the 10g monofilament and its limitations: a review. Diabetes Res Clin Pract 90:1–7
Richard JL, Reilhes L, Buvry S, Goletto M, Faillie JL (2014) Screening patients at risk for diabetic foot ulceration: a comparison between measurement of vibration perception threshold and 10-g monofilament test. Int Wound J 11:147–151
Young MJ, Breddy JL, Veves A, Boulton AJ (1994) The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds. A prospective study. Diabetes Care 17:557–560
Celermajer DS, Sorensen KE, Spiegelhalter DJ, Georgakopoulos D, Robinson J, Deanfield JE (1994) Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women. J Am Coll Cardiol 24:471–476
Crawford F, Inkster M, Kleijnen J, Fahey T (2007) Predicting foot ulcers in patients with diabetes: a systematic review and meta-analysis. QJM 100:65–86
Roustit M, Cracowski JL (2013) Assessment of endothelial and neurovascular function in human skin microcirculation. Trends Pharmacol Sci 34:373–384
Holowatz LA, Thompson-Torgerson CS, Kenney WL (2008) The human cutaneous circulation as a model of generalized microvascular function. J Appl Physiol (1985)105:370–372
de Jongh RT, Serne EH, Ijzerman RG, de Vries G, Stehouwer CD (2004) Impaired microvascular function in obesity: implications for obesity-associated microangiopathy, hypertension, and insulin resistance. Circulation 109:2529–2535
Levy BI, Schiffrin EL, Mourad JJ et al (2008) Impaired tissue perfusion: a pathology common to hypertension, obesity, and diabetes mellitus. Circulation 118:968–976
Karvestedt L, Martensson E, Grill V et al (2009) Peripheral sensory neuropathy associates with micro- or macroangiopathy: results from a population-based study of type 2 diabetic patients in Sweden. Diabetes Care 32:317–322
Tesfaye S, Selvarajah D (2012) Advances in the epidemiology, pathogenesis and management of diabetic peripheral neuropathy. Diabetes Metab Res Rev 28(Suppl 1):8–14
Mori TA, Watts GF, Burke V, Hilme E, Puddey IB, Beilin LJ (2000) Differential effects of eicosapentaenoic acid and docosahexaenoic acid on vascular reactivity of the forearm microcirculation in hyperlipidemic, overweight men. Circulation 102:1264–1269
Coste TC, Gerbi A, Vague P, Pieroni G, Raccah D (2003) Neuroprotective effect of docosahexaenoic acid-enriched phospholipids in experimental diabetic neuropathy. Diabetes 52:2578–2585
Okuda Y, Mizutani M, Ogawa M et al (1996) Long-term effects of eicosapentaenoic acid on diabetic peripheral neuropathy and serum lipids in patients with type II diabetes mellitus. J Diabetes Complicat 10:280–287
Ghoreishi Z, Esfahani A, Djazayeri A et al (2012) Omega-3 fatty acids are protective against paclitaxel-induced peripheral neuropathy: a randomized double-blind placebo controlled trial. BMC Cancer 12:355
Targher G, Byrne CD (2013) Clinical review: nonalcoholic fatty liver disease: a novel cardiometabolic risk factor for type 2 diabetes and its complications. J Clin Endocrinol Metab 98:483–495
Bhatia LS, Curzen NP, Calder PC, Byrne CD (2012) Non-alcoholic fatty liver disease: a new and important cardiovascular risk factor? Eur Heart J 33:1190–1200
Pinarbasi B, Demir K, Oflaz H et al (2012) Measurement of the coronary flow velocity reserve in patients with non-alcoholic fatty liver disease. Turk J Gastroenterol 23:720–726
Lv WS, Sun RX, Gao YY et al (2013) Nonalcoholic fatty liver disease and microvascular complications in type 2 diabetes. World J Gastroenterol 19:3134–3142
Scorletti E, Bhatia L, McCormick KG et al (2014) Design and rationale of the WELCOME trial: a randomised, placebo controlled study to test the efficacy of purified long chain omega-3 fatty treatment in non-alcoholic fatty liver disease. Contemp Clin Trials 37:301–311
Scorletti E, Bhatia L, McCormick KG et al (2014) Effects of purified eicosapentaenoic and docosahexaenoic acids in nonalcoholic fatty liver disease: results from the Welcome* study. Hepatology 60:1211–1221
Spruce MC, Bowling FL (2012) Diabetic foot screening: new technology versus 10g monofilament. Int J Low Extrem Wounds 11:43–48
Gu C, Griffin MJ (2013) Spatial summation of vibrotactile sensations at the foot. Med Eng Phys 35:1221–1227
Gu C, Griffin MJ (2011) Vibrotactile thresholds at the sole of the foot: effect of vibration frequency and contact location. Somatosens Mot Res 28:86–93
Clough GF, Turzyniecka M, Walter L et al (2009) Muscle microvascular dysfunction in central obesity is related to muscle insulin insensitivity but is not reversed by high-dose statin treatment. Diabetes 58:1185–1191
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Angulo P, Hui JM, Marchesini G et al (2007) The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 45:846–854
Guha IN, Parkes J, Roderick P et al (2008) Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: validating the European Liver Fibrosis Panel and exploring simple markers. Hepatology 47:455–460
Polak JF, Pencina MJ, O'Leary DH, D'Agostino RB (2011) Common carotid artery intima-media thickness progression as a predictor of stroke in multi-ethnic study of atherosclerosis. Stroke 42:3017–3021
Simon A, Megnien JL, Chironi G (2010) The value of carotid intima-media thickness for predicting cardiovascular risk. Arterioscler Thromb Vasc Biol 30:182–185
Karaca U, Schram MT, Houben AJ, Muris DM, Stehouwer CD (2014) Microvascular dysfunction as a link between obesity, insulin resistance and hypertension. Diabetes Res Clin Pract 103:382–387
Clough GF, L'esperance V, Turzyniecka M et al (2011) Functional dilator capacity is independently associated with insulin sensitivity and age in central obesity and is not improved by high dose statin treatment. Microcirculation 18:74–84
Turzyniecka M, Wild SH, Krentz AJ et al (2009) Skeletal muscle microvascular exchange capacity is associated with hyperglycaemia in subjects with central obesity. Diabet Med 26:1112–1119
De Jongh RT, Serne EH, IJzerman RG, Jorstad HT, Stehouwer CD (2008) Impaired local microvascular vasodilatory effects of insulin and reduced skin microvascular vasomotion in obese women. Microvasc Res 75:256–262
de Boer MP, Meijer RI, Wijnstok NJ et al (2012) Microvascular dysfunction: a potential mechanism in the pathogenesis of obesity-associated insulin resistance and hypertension. Microcirculation 19:5–18
Tesfaye S, Boulton AJ, Dyck PJ et al (2010) Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 33:2285–2293
Young LH, Wackers FJ, Chyun DA et al (2009) Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA 301:1547–1555
Oni ET, Agatston AS, Blaha MJ et al (2013) A systematic review: burden and severity of subclinical cardiovascular disease among those with nonalcoholic fatty liver; should we care? Atherosclerosis 230:258–267
Villanova N, Moscatiello S, Ramilli S et al (2005) Endothelial dysfunction and cardiovascular risk profile in nonalcoholic fatty liver disease. Hepatology 42:473–480
Yokoyama H, Yokota Y, Tada J, Kanno S (2007) Diabetic neuropathy is closely associated with arterial stiffening and thickness in type 2 diabetes. Diabet Med 24:1329–1335
Seah SA, Griffin MJ (2008) Normal values for thermotactile and vibrotactile thresholds in males and females. Int Arch Occup Environ Health 81:535–543
Shun CT, Chang YC, Wu HP et al (2004) Skin denervation in type 2 diabetes: correlations with diabetic duration and functional impairments. Brain 127:1593–1605
Sumner CJ, Sheth S, Griffin JW, Cornblath DR, Polydefkis M (2003) The spectrum of neuropathy in diabetes and impaired glucose tolerance. Neurology 60:108–111
Sveen KA, Karime B, Jorum E et al (2013) Small- and large-fiber neuropathy after 40 years of type 1 diabetes: associations with glycemic control and advanced protein glycation: the Oslo Study. Diabetes Care 36:3712–3717
Byrne CD (2010) Fatty liver: role of inflammation and fatty acid nutrition. Prostaglandins Leukot Essent Fat Acids 82:265–271
Im S, Kim SR, Park JH, Kim YS, Park GY (2012) Assessment of the medial dorsal cutaneous, dorsal sural, and medial plantar nerves in impaired glucose tolerance and diabetic patients with normal sural and superficial peroneal nerve responses. Diabetes Care 35:834–839
Callaghan BC, Cheng HT, Stables CL, Smith AL, Feldman EL (2012) Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol 11:521–534
Corretti MC, Anderson TJ, Benjamin EJ et al (2002) Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 39:257–265
Acknowledgements
The authors thank G. Wise, S. Triggs and B. Clancy (research nurses, National Institute for Health Research Southampton Biomedical Research Centre, Southampton, UK) for their support with the trial, L. England (Human Development and Health Academic Unit, Faculty of Medicine, University of Southampton, Southampton, UK) for research governance administration, and C. Gu and Y. Ye (postgraduate researchers, Institute of Sound and Vibration Research, University of Southampton, Southampton, UK) for the VPT protocol.
These findings were presented as an abstract at the Diabetes UK Professional Conference, London, UK, 11 March 2015. Some of the preliminary data were also presented as abstracts at the 61st British Microcirculation Society Meeting, London, UK, 18–19 April 2011, the 62nd British Microcirculation Society Meeting, Oxford, UK, 4–6 July 2012 and the Diabetes UK Annual Professional Conference, London, UK, 30 March–1 April 2011.
Funding
Omacor and placebo were provided by Pronova Biopharma through Abbott Laboratories, Southampton, UK. This work was supported by a National Institute for Health Research (NIHR) Southampton Biomedical Research Unit grant and by a Diabetes UK allied health research training fellowship awarded to KGM (Diabetes UK. BDA 09/0003937). CDB, PCC and ES are supported in part by the NIHR Southampton Biomedical Research Centre.
Duality of interest
PCC serves on the Clinical Advisory Board of Pronova Biopharma and has acted as a consultant to Amarin. All other authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
All named authors fulfil all three International Committee of Medical Journal Editors uniform requirements for authorship of this manuscript. KGM, CDB, GFC and MJG made a substantial contribution to the study conception and design; KGM, ES and LB made a substantial contribution to data acquisition; CDB, GFC, KGM, PCC and MJG conducted the data analysis and interpretation; CDB and GFC drafted the manuscript; and PCC, MJG, KGM, ES, and LB helped to revise it critically for important intellectual content. All authors approved the final version to be published. CDB is responsible for the integrity of the work as a whole and is the guarantor of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McCormick, K.G., Scorletti, E., Bhatia, L. et al. Impact of high dose n-3 polyunsaturated fatty acid treatment on measures of microvascular function and vibration perception in non-alcoholic fatty liver disease: results from the randomised WELCOME trial. Diabetologia 58, 1916–1925 (2015). https://doi.org/10.1007/s00125-015-3628-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-015-3628-2