Abstract
Aim/hypothesis
In people with type 2 diabetes, exercise improves glucose control (as reflected in HbA1c) and physical fitness, but it is not clear to what extent these exercise-induced improvements are correlated with one another. We hypothesised that reductions in HbA1c would be related: (1) to increases in aerobic fitness and strength respectively in patients performing aerobic training or resistance training; and (2) to changes in strength and aerobic fitness in patients performing aerobic and resistance training.
Methods
We randomly allocated 251 type 2 diabetes patients to aerobic, resistance, or aerobic plus resistance training, or to a sedentary control group. Peak oxygen consumption (\( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \)), workload, treadmill time and ventilatory threshold measurements from maximal treadmill exercise testing were measured at baseline and 6 months. Muscular strength was measured as the maximum weight that could be lifted eight times on the leg press, bench press and seated row exercises.
Results
With aerobic training, significant associations were found between changes in both \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) (p = 0.040) and workload (p = 0.022), and changes in HbA1c. With combined training, improvements in \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) (p = 0.008), workload (p = 0.034) and ventilatory threshold (p = 0.003) were significantly associated with changes in HbA1c. Increases in strength on the seated row (p = 0.006) and in mid-thigh muscle cross-sectional area (p = 0.030) were significantly associated with changes in HbA1c after resistance exercise, whereas the association between increases in muscle cross-sectional area and HbA1c in participants doing aerobic plus resistance exercise (p = 0.059) was of borderline significance.
Conclusions/interpretation
There appears to be a link between changes in fitness and HbA1c. The improvements in cardiorespiratory fitness with aerobic training may be a better predictor of changes in HbA1c than improvements in strength.
Similar content being viewed by others
Introduction
Numerous small studies have shown that aerobic exercise training [1–5] and resistance exercise training [2, 6–9] each cause important improvements in blood glucose control, reflected in reductions in HbA1c in patients with type 2 diabetes. Aerobic training increases cardiorespiratory fitness [2–5] and resistance training increases muscular strength [2, 7, 8] in adults with type 2 diabetes, while higher cardiorespiratory fitness [10, 11] and muscular fitness [12] are associated with reduced overall mortality rates. The Diabetes Aerobic and Resistance Exercise (DARE) Trial (ClinicalTrials.gov registration no. NCT00195884) [13] was a randomised controlled trial to determine the effects of aerobic exercise training, resistance exercise training and their combination on glycaemic control in previously inactive type 2 diabetes patients aged 39 to 70 years. Both aerobic and resistance exercise training improved glycaemic control, and a combination of both was superior to either type of exercise training alone [13]. Moreover, when performed separately, aerobic exercise training resulted in significant improvements in maximal and submaximal aerobic fitness, whereas resistance exercise training led to considerable improvements in muscular strength [14]. When performed in combination, aerobic and resistance exercise improved aerobic fitness and muscle strength [14].
There is empirical evidence that improvements in peak oxygen consumption (\( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \)) are associated with improvements in glycaemic control. A meta-analysis by Boulé et al. [15] found a significant correlation across studies (r = 0.72, p = 0.04) between increases in \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) following aerobic exercise training and decreases in HbA1c. However, these results were obtained by pooling summary data from small studies and driven to a large extent by those of a single study [4], in which exercise intensity and change in HbA1c were much greater than in the other studies [16–19]. Also, few studies have looked at improvements in submaximal aerobic capacity in individuals with type 2 diabetes [14, 16]. Submaximal exercise is often recommended for sedentary individuals, to overcome many of the limitations of using higher training intensities, notably the risk of injuries and low adherence to exercise programmes [20]. An important indicator of submaximal aerobic performance is the ventilatory threshold, which represents the highest oxygen consumption that can be maintained without a continuous increase in blood lactate [21]. Currently, it is unclear if an association exists between improvements in ventilatory threshold and change in HbA1c. In addition, although significant improvements in strength and HbA1c through exercise training have been reported in the past, to our knowledge no studies have reported an association between strength gains and reductions in HbA1c and no study has compared the relationship between improvements in fitness and HbA1c with aerobic and resistance training separately as well as in combination. In view of the strong evidence demonstrating that higher levels of fitness [10, 15] and good glycaemic control [22] are each associated with reduced morbidity and mortality rates in type 2 diabetes, advancing our understanding of the possible relationship between these health outcomes is important.
In the present study, we examined the associations between changes in fitness and HbA1c changes induced by aerobic, resistance and combined aerobic and resistance exercise training in the DARE clinical trial [13]. We hypothesised that increases in cardiorespiratory fitness in participants undergoing aerobic training only and increases in strength in participants undergoing resistance training would each be associated with decreases in HbA1c. We also hypothesised that changes in HbA1c induced by combined exercise training would be correlated with improvements in aerobic and muscular fitness.
Methods
Design
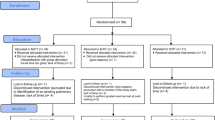
This project is a sub-study of the DARE clinical trial, which has been described elsewhere [13]. The DARE trial was a single-centre, randomised controlled trial with parallel group design that examined the effects of aerobic and resistance exercise training as well as a combination of both on HbA1c in patients with type 2 diabetes. The trial included a 4-week run-in phase, followed by a 22-week intervention phase. This study was approved by the Ottawa Hospital Research Ethics Board and written informed consent was obtained from all participants.
Participants
Previously sedentary type 2 diabetic patients between the ages of 39 and 70 years were recruited through advertising, physicians and word of mouth. Inclusion criteria for the DARE trial included type 2 diabetes for at least 6 months and baseline HbA1c between 6.6% and 9.9% (normal 4–6%). Exclusion criteria are described elsewhere [13]. The participants’ baseline characteristics are presented in Table 1.
Exercise intervention
Run-in phase
Participants exercised at community-based facilities, supervised by personal trainers. Prior to randomisation, participants entered a 4-week run-in period to assess compliance. Participants performed 15 to 20 min of aerobic exercise at moderate intensity (60% \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \)) three times a week and one to two sets of seven resistance exercises at a moderate intensity twice a week with supervision. Only participants attending ≥ 10 of the scheduled 12 run-in sessions were eligible for randomisation. Randomisation was stratified by age (39 to 54 years and 55 to 70 years) and sex.
Aerobic exercise training
During the intervention phase (weeks 5 to 26), aerobic training duration and intensity increased on a weekly basis to a maximum of 45 min per session at 75% of maximal heart rate. Heart rate monitors (Polar Electro; Oy, Kempele, Finland) were used to standardise exercise intensity. Target heart rates were based on maximum heart rate achieved during the maximal treadmill exercise test performed at baseline. All aerobic activities were performed three times per week on a treadmill or cycle ergometer. Participants were free to vary the machine used from one session to the next. Details of the exercise training programme are available online (http://annals.org/content/147/6/357.full#app-1, accessed 13 August, 2010)
Resistance exercise training
Throughout the resistance training programme, participants alternated between two groups of seven exercises targeting all major muscle groups. These were as follows: Group A: abdominal crunch, seated row, biceps curl, bench press, leg press, shoulder press and leg extension; Group B: abdominal crunch, lateral pulldown, triceps pushdown, chest press, leg press, upright row and leg curl. All resistance training exercises were performed on weight machines. During the intervention phase (weeks 5–26) the frequency of resistance training increased from 2 to 3 days per week, the number of sets performed for each exercise increased from two to three sets and the amount of weight lifted for a given exercise also increased, whereas the number of repetitions decreased to a maximum of eight repetitions. Completion of each set of a single exercise took 30 to 60 s and participants were encouraged to rest 2 to 3 min between sets to allow for maximal muscle recovery. The amount of time spent on active exercise during a 45 min resistance exercise session was generally 15 to 20 min, excluding time spent resting between sets. When the participant could perform more than eight repetitions while maintaining proper form, the weight or the resistance of the exercise was increased by 2.3 to 4.5 kg.
Combined exercise training
The participants in the combined training group performed the full aerobic training programme plus the full resistance training programme to assure an adequate dose of each type of exercise.
Control group
Subsequent to the run-in phase, participants assigned to the control group were asked to revert to their level of activity at baseline and to maintain this level for the remainder of the study.
Supervision
Direct supervision by trainers occurred with equal frequency in all exercising groups. Individual exercise supervision was provided weekly for the first 4 weeks and biweekly thereafter. Attendance was verified through direct observation, exercise logs and electronic scanning of membership cards.
Outcomes and measurements
All participants were assessed at baseline (before the beginning of the run-in phase) and at 6 months (at the end of the intervention). HbA1c was measured using turbidimetric immunoinhibition on an analyser (LX20; Beckman Instruments, Brea, CA, USA). Cardiorespiratory (aerobic) fitness (\( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \)) was determined during a maximal treadmill exercise stress test at the University of Ottawa Heart Institute. The test followed a ramp treadmill protocol with continuous time and 12-lead electrocardiogram monitoring (v.4.03; GE Marquette Medical Systems, Milwaukee, WI, USA) as well as breath-by-breath analysis of oxygen consumption and carbon dioxide production (CPX-D Metabolic Cart; MedGraphics, St Paul, MN, USA). As older adults often do not reach a plateau in oxygen consumption, \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) was measured as the highest minute rate of oxygen consumption achieved during the last 30 s of the test to volitional fatigue. Each participant performed the same ramp protocol during baseline and post intervention testing. We also used workload (W) and treadmill time (min) measurements obtained from stress testing to assess the association between physical fitness and HbA1c.
In addition to determining whether maximal exercise responses were associated with improvements in HbA1c, we examined the relationship between improvements in submaximal aerobic performance and HbA1c. Maximal aerobic capacity was defined as the maximal amount of physiological work that can be performed and is typically measured by maximal oxygen consumption. Submaximal aerobic capacity refers to performance of aerobic activities at a percentage of maximal aerobic capacity. As mentioned previously, ventilatory threshold is an important indicator of submaximal aerobic performance. Ventilatory threshold was determined from maximal exercise stress tests using two criteria: (1) the point where ventilation (\( {\mathop V\limits^ \cdot }_{{\text{E}}} \)) increased disproportionately relative to \( \mathop {V}\limits^\cdot {{\text{O}}_2} \) [23]; and (2) the point of dislinear rise in carbon dioxide production (\( \mathop {V}\limits^\cdot {{\text{O}}_{2\;{\text{peak}}}} \)) relative to \( \mathop {V}\limits^\cdot {{\text{O}}_2} \) (V-slope method) [24]. These techniques have been shown to be sensitive and non-invasive measures for evaluating cardiorespiratory performance [23, 25] and \( {\mathop V\limits^ \cdot }_{{\text{E}}} /{\mathop V\limits^ \cdot }O_{2} \) has been shown to be the best single index for detecting ventilatory threshold when using ventilation and/or gas exchange indices [26]. However, using a dual criterion provides a more specific determination of the ventilatory threshold [23]. In the present study, both criteria were met for most participants, but in a few cases, the rise in \( {\mathop {\text{V}}\limits^\bullet_{\text{E}}} \) relative to \( \mathop {V}\limits^\cdot {{\text{O}}_2} \) was easier to recognise and was used to determine the ventilatory threshold. One evaluator determined the ventilatory threshold for all participants at 0 and 6 months. The same evaluator repeated the assessment of all ventilatory thresholds no less than 2 weeks after the last ventilatory threshold had been determined to assure consistency in the results [27]. Intraobserver reproducibility of ventilatory thresholds between the first and second readings was high. For the few participants where ventilatory threshold differed between the first and second reading, a third reading was performed no less than 2 weeks after the previous reading to confirm the ventilatory threshold.
Muscular strength was determined for the leg press, bench press and seated row on a multi-station gym (EXM-2000S; Body Solid, Forest Park, IL, USA). Strength was measured as the maximum weight that could be lifted eight times following an eight repetition maximum protocol. Proper lifting and breathing techniques were demonstrated by an exercise specialist prior to each exercise. Mid-thigh muscle cross-sectional area was measured by computed tomography scan midway between the inguinal crease and the proximal border of the patella [28]. The images were downloaded as digital files and analysed by Slice-O-Matic software, version 4 (Tomovision, Montreal, QC, Canada), as described elsewhere [29].
Statistical analysis
We used linear mixed models with repeated measures for analyses of changes over time, as described previously [13]. This method uses all available data and does not require imputation of missing values. To determine whether there was an association between changes in measures of physical fitness and changes in HbA1c among the exercise groups, measures of fitness including \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) (ml kg−1 min−1), workload (W), treadmill time (min), \( \mathop {V}\limits^\cdot {{\text{O}}_2} \) (in ml kg−1 min−1) at ventilatory threshold, seated row (kg), leg press (kg), bench press (kg) and muscle cross-sectional area by computed tomography scan (cm2) were each tested as independent variables within an interaction term by time and group (aerobic training, resistance training, combined training and control), in individual models for HbA1c. These models were run with and without adjustment for changes in weight as well as changes in hypoglycaemic medication. To understand the effect of baseline HbA1c on the results, a subgroup analysis was done for participants with baseline HbA1c at or above the median of 7.5%, as well as for those with baseline values below the median. Within the mixed models, 95% CIs and p values for change in HbA1c between baseline and 6 months were estimated within each group.
Scatter plots with regression estimates were also used to explore the relationship between both cardiorespiratory fitness and strength indicators, and HbA1c. A p value of less than 0.05 was considered statistically significant. We used SAS version 9.1 (SAS, Cary, NC, USA) for all analyses.
Results
The results for changes in HbA1c and body composition have been reported elsewhere [13]. To summarise, both aerobic and resistance exercise training alone led to significant reductions in HbA1c (−0.51, p = 0.007 and −0.38, p = 0.037, respectively) in comparison to the control group. In the combined training group, HbA1c changed by an additional −0.46 percentage points (p = 0.014) compared with the aerobic training group and by an additional −0.59 percentage points (p = 0.001) compared with the resistance training group. Body weight significantly decreased with aerobic exercise training in comparison to the control group (−2.6 vs −0.3 kg, p = 0.008); the change in weight with combined exercise training did not differ from that in the aerobic training group. The improvements in fitness in the DARE trial have also been reported elsewhere [14]. In short, after aerobic and combined exercise training, \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) increased by 1.73 (6%) and 1.93 (7%) ml kg−1 min−1, and treadmill time increased by 1.19 (12%) and 1.14 (13%) min, respectively, compared with the control group (p < 0.05). Significant increases in strength were measured following aerobic, combined and resistance exercise training on the leg press (aerobic 39 kg [42%], combined 49 kg [48%], resistance 56 kg [65%]), bench press (aerobic 6 kg [24%], combined 12 kg [38%], resistance 13 kg [57%]) and seated row (aerobic 7 kg [21%], combined 13 kg [33%], resistance 14 kg [41%]) exercises (p < 0.05).
The results from regression analyses are displayed in Table 2. Our results showed significant associations between changes in \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) (p = 0.008), maximal workload (p = 0.034) and ventilatory threshold (p = 0.003), as well as a trend towards a significant association between changes in treadmill time (p = 0.057) and changes in HbA1c with combined exercise training (Fig. 1). With aerobic training only, there were significant associations between increments both in \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) (p = 0.040) and maximal workload (p = 0.022) and HbA1c whereas the association between changes in ventilatory threshold and reductions in HbA1c (p = 0.058) was of borderline significance (Fig. 2). The association between changes in cardiorespiratory fitness and HbA1c in the aerobic exercise training and combined exercise training groups remained significant after adjusting for changes in weight as well as changes in hypoglycaemic medication. The association between changes both in ventilatory threshold in the aerobic group and in treadmill time in the combined group and HbA1c reached statistical significance after adjusting for changes in weight (p = 0.040 and p = 0.044, respectively). We found a significant association between changes in seated row performance and changes in HbA1c with resistance exercise training only (p = 0.006), as well as a trend towards an association with improvements in leg press performance (p = 0.060). No significant associations were found between changes in strength and HbA1c with combined exercise training (leg press p = 0.134; bench press p = 0.894; seated row p = 0.539). Changes in mid-thigh muscle cross-sectional area were significantly associated with changes in HbA1c with resistance training only (p = 0.030) (Fig. 3), while in the combined exercise group the association fell just short of statistical significance (p = 0.059) (Fig. 4). The association between change in muscle cross-sectional area and HbA1c was unchanged after adjusting for change in hypoglycaemic medication, but was no longer significant in the resistance group after adjusting for change in weight.
Associations between changes both in cardiorespiratory fitness and HbA1c and combined exercise training between baseline and 6 months. a \( \mathop {V}\limits^\cdot {{\text{O}}_{2\;{\text{peak}}}} \) (β = −0.034, p = 0.008), b treadmill time (β = −0.045, p = 0.057), c ventilatory threshold (β = −0.076, p = 0.003) and d maximal workload (β = −0.047, p = 0.034). Adjusted β estimates are presented
Associations between changes both in cardiorespiratory fitness and HbA1c and aerobic exercise training between baseline and 6 months. a \( \mathop {V}\limits^\cdot {{\text{O}}_{2\;{\text{peak}}}} \) (β = −0.028, p = 0.040), b treadmill time (β = −0.010, p = 0.668), c ventilatory threshold (β = −0.055, p = 0.058) and d maximal workload (β = −0.068, p = 0.022). Adjusted β estimates are presented
Associations between changes both in muscular strength and HbA1c and resistance exercise training between baseline and 6 months. a Seated row (β = −0.312, p = 0.006), b bench press (β = −0.092, p = 0.391), c leg press (β = −0.266, p = 0.060) and d mid-thigh muscle cross-sectional area (β = −0.027, p = 0.030). Adjusted β estimates are presented
Associations between changes both in muscular strength and HbA1c and combined exercise training between baseline and 6 months. a Seated row (β = −0.092, p = 0.340), b bench press (β = −0.019, p = 0.823), c leg press (β = −0.140, p = 0.260) and d mid-thigh muscle cross-sectional area (β = −0.020, p = 0.059). Adjusted β estimates are presented
When we ran the models separately for participants with baseline HbA1c levels below the median of 7.5%, changes in fitness were no longer significantly associated with changes in HbA1c in any of the intervention groups. In participants with baseline HbA1c levels at or above the median, changes in workload, treadmill time, \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) and ventilatory threshold were significantly associated with changes in HbA1c in the combined training group, whereas in the aerobic training group only changes in workload were associated with improvements in glucose control.
Discussion
The present study examined for the first time the relationship between changes in physical fitness and changes in HbA1c in individuals with type 2 diabetes undergoing exercise training. Our results demonstrate that improvements in maximal aerobic fitness (\( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) and maximal workload) were significantly associated with improvements in HbA1c with aerobic training only and with combined aerobic and resistance training. Furthermore, increases in submaximal aerobic fitness, reflected by improvements in ventilatory threshold, were also associated with improvements in HbA1c with combined exercise training. Increments in strength on the seated row exercise, as well as changes in mid-thigh muscle cross-sectional area were significantly associated with reductions in HbA1c with resistance exercise training only.
The present study was a randomised controlled trial using a large sample of individuals with type 2 diabetes, who underwent 6 months of exercise training. Aerobic exercise training resulted in improvements in \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) in addition to other markers of maximal and submaximal aerobic capacity. Our results underscore the notion that improvements in cardiorespiratory fitness are associated with reductions in HbA1c with aerobic exercise training. Boulé et al. [15] previously reported a significant correlation across studies between post-intervention mean difference in \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2max}}} \) and changes in HbA1c (r = 0.72, p = 0.04). Moreover, Vanninen et al. [16] found that \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2max}}} \) was inversely correlated with HbA1c value (%) at the end of a 12-month intervention (r = −0.28, p < 0.01) in men with type 2 diabetes. In contrast to previous studies focusing primarily on changes in maximal aerobic performance, we show here that increasing submaximal and/or maximal aerobic fitness can lead to important improvements in cardiorespiratory fitness and metabolic health among individuals with type 2 diabetes. It is, however, possible that further improvements in aerobic fitness (which can be achieved with higher training intensities) could result in further improvements in glycaemic control. For example, Boulé et al. [15] found that the study using the highest training intensity (≥75% \( \mathop {V}\limits^\cdot {{\text{O}}_{2\;{\text{peak}}}} \)) [4] had larger improvements in \( \mathop {V}\limits^\cdot {{\hbox{O}}_{2\;{\rm{peak}}}} \) and HbA1c than studies using moderate training intensities.
In addition to finding a significant association between improvements in aerobic fitness and HbA1c with aerobic training only, this study demonstrates that improvements in cardiorespiratory fitness, notably increases in \( \mathop {V}\limits^\cdot {{\text{O}}_{2\;{\text{peak}}}} \), maximal workload and ventilatory threshold, were significantly associated with changes in HbA1c with combined exercise training. Maximal oxygen consumption is largely dependent on the amount of oxygen available to exercising tissues. Generally, individuals with type 2 diabetes have above-normal levels of HbA1c, which could negatively affect tissue oxygenation [30]. This may in part result from the addition of a glucose molecule at the N-terminal valine of ß chains, which is thought to interfere with the binding of 2,3-diphosphoglycerate (2,3 DPG), an important physiological regulator of haemoglobin function [31, 32]. For this reason, it is conceivable that improving glucose disposal with exercise training, which in turn reduces HbA1c levels, could enable 2,3 DPG to bind normally with haemoglobin. This would allow 2,3 DPG to carry out its role in reducing haemoglobin affinity for oxygen, thus making oxygen readily available to exercising tissues. This may, however, be true only for individuals with higher baseline levels of HbA1c. The DARE trial [13] showed that participants with baseline HbA1c levels above the median of 7.5% had much greater reductions in HbA1c post intervention than those with baseline values below the median. This was true for participants in the aerobic training group (>7.5–0.83%, p < 0.001 vs <7.5–0.10%, p = 0.50), the resistance training group (>7.5–0.49%, p = 0.013 vs <7.5–0.08%, p = 0.59) and the combined training group (>7.5–1.42%, p < 0.001 vs <7.5–0.46%, p = 0.002). Accordingly, the results from the present analysis revealed that the relationship between changes in markers of cardiorespiratory fitness and HbA1c were only significant among participants with higher levels of HbA1c at baseline, a relationship that was more prevalent with combined exercise training than with aerobic training only. It is therefore plausible that reducing HbA1c levels may have a positive effect on cardiorespiratory fitness. However, this study did not measure the specific physiological mechanisms responsible for improving fitness and glucose control simultaneously.
Alternatively, the physiological adaptations of the cardiovascular system to aerobic exercise training that lead to improvements in aerobic fitness seem to help improve blood glucose transport, delivery and diffusion into muscle cells [33–35]. When combined with a resistance training programme, which increases muscle mass and therefore glucose storage capacity [36–39], a combined exercise programme, not surprisingly, would lead to much greater reductions in HbA1c than either aerobic or resistance training alone. As reducing HbA1c would not affect changes in strength, it is more feasible to assume that the improvements in HbA1c were mediated at least to some extent by improvements in cardiorespiratory fitness and the increases in glucose storage capacity associated with increases in strength.
The results from this study showed that strength gains and HbA1c improvements were significantly associated with a resistance exercise training programme. Improvements in muscular strength with resistance exercise training are largely affected by baseline strength levels. Consequently, untrained individuals normally have rapid improvements in strength during the initial phases of a training programme, which are predominantly attributed to a learning effect as well as to neuromuscular adaptations [39]. Neuromuscular adaptations reflect increases in neural drive, muscle recruitment and firing rate, as well as greater and more synchronised discharge of motor units [37, 39], which ultimately do not affect glucose metabolism. As DARE participants were sedentary individuals at the onset of the trial, we assume that a large proportion of strength gains over the 6 month training period was due to neuromuscular adaptations. Conversely, the largest proportion of glucose uptake takes place within skeletal muscles. Since strength increments are generally accompanied by enlarged muscle size [37–39], we expected a relationship between improvements in strength and changes in HbA1c. Small but significant improvements in mid-thigh muscle cross-sectional area were found following resistance exercise training (+8.0 cm2) and combined exercise training (+7.0 cm2) in comparison to the control group (p < 0.001) [13]. Accordingly, the association between changes in muscle cross-sectional area and HbA1c was significant only with resistance training, falling just short of statistical significance with combined exercise training. Thus although it could be argued that significant strength improvements can be achieved with lower numbers of sets and/or training sessions per week [40–42], it may be necessary for people with type 2 diabetes to perform a greater work volume (i.e. up to three sessions per week of resistance exercise training) to achieve significant improvements in HbA1c.
Limitations
The present study has limitations, mainly attributed to the fact that our trial analyses were not originally designed to assess the relationship between changes in HbA1c and fitness. Additionally, it is possible that the significant associations between the changes in HbA1c and fitness in the combined exercise group were influenced by the greater work volume performed by participants in this group. However, the physiological adaptations to aerobic training are different from those to resistance training, so we cannot assume that our results simply reflect greater work volume. Moreover, Boulé et al. [15] previously reported that work volume was not significantly correlated with changes in HbA1c when expressed as the total metabolic cost of an activity per hour (r = −0.12, p = 0.8) or the total metabolic cost of an activity per hour per week (r = −0.46, p = 0.26).
Significance
The present study underlines the importance of including some form of exercise in treatment strategies for type 2 diabetes. Although other treatments for type 2 diabetes, including the use of oral hypoglycaemic medication and dieting, are also successful in reducing blood glucose, these methods do not improve physical fitness. Improving physical fitness in its own right is crucial for individuals with type 2 diabetes, as the majority are sedentary and have low exercise tolerance. We have shown that aerobic exercise training leads to important improvements in cardiorespiratory fitness and that resistance training improves muscular strength [14]. We have also reported that glucose control is improved with aerobic and resistance training whether performed alone or in combination [13]. The results from this study show that, to some extent, improving cardiorespiratory fitness and/or muscular strength is related to improvements in glucose control. However, the link between fitness and glucose control does not appear to be very strong, suggesting that changes in glucose control during exercise training are not entirely dependent on improvements in fitness. Hence, regardless of whether an exercise programme improves physical fitness, glucose control or both, the physical activity involved offers health benefits and improves quality of life in a way that other treatments for type 2 diabetes cannot on their own. In addition, the present study provides further support for the notion that: (1) combined exercise training is the most beneficial exercise programme for individuals with type 2 diabetes; and (2) improvements in fitness related to physiological adaptations to aerobic and resistance training are associated with improved glucose control. However, it would be interesting to see the effects of different exercise interventions and higher training intensities on improvements in fitness and HbA1c, as well as the association between these two measures. Moreover, future research should investigate the specific mechanisms associated with improvements in fitness and HbA1c, and how these mechanisms could be linked to one another.
In summary, we have shown that increases in cardiorespiratory fitness were associated with reduced HbA1c in combined exercise training and aerobic training only. To a lesser extent, changes in muscular strength were also associated with changes in HbA1c with resistance training only. Hence, both aerobic and resistance exercise training alone cause clinically important improvements in physical fitness and glycaemic control. However, the association between changes in physical fitness and glycaemic control may be more pronounced with combined exercise training due to improvements in aerobic fitness and in muscular strength.
Abbreviations
- DARE:
-
Diabetes Aerobic and Resistance Exercise
- 2,3 DPG:
-
2,3-Diphosphoglycerate
- \( {\mathop V\limits^ \cdot }_{E} \) :
-
Ventilation
- \( \mathop {V}\limits^\cdot {{\text{O}}_{\text{2 peak}}} \) :
-
Peak oxygen consumption
References
Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ (2001) Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 286:1218–1227
Cauza E, Hanusch-Enserer U, Strasser B et al (2005) The relative benefits of endurance and strength training on the metabolic factors and muscle function of people with type 2 diabetes mellitus. Arch Phys Med Rehabil 86:1527–1533
Kadogloua N, Iliadisa F, Angelopouloub N et al (2007) The anti-inflammatory effects of exercise training in patients with type 2 diabetes mellitus. Eur J Cardiov Prev R 14:837–843
Mourier A, Gautier JF, de Kerviler E et al (1997) Mobilization of visceral adipose tissue related to the improvement in insulin sensitivity in response to physical training in NIDDM. Effects of branched-chain amino acid supplements. Diabetes Care 20:385–391
Toledo F, Menshikova EV, Ritov VB et al (2007) Effects of physical activity and weight loss on skeletal muscle mitochondria and relationship with glucose control in type 2 diabetes. Diabetes 56:2142–2147
Baldi JC, Snowling N (2003) Resistance training improves glycaemic control in obese type 2 diabetic men. Int J Sports Med 24:419–423
Castaneda C, Layne JE, Munoz-Orians L et al (2002) A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Diabetes Care 25:2335–2341
Dunstan DW, Daly RM, Owen N et al (2002) High-intensity resistance training improves glycemic control in older patients with type 2 diabetes. Diabetes Care 25:1729–1736
Durak EP, Jovanovic-Peterson L, Peterson CM (1990) Randomized crossover study of effect of resistance training on glycemic control, muscular strength, and cholesterol in type I diabetic men. Diabetes Care 13:1039–1043
Wei M, Gibbons LW, Kampert JB, Nichaman MZ, Blair SN (2000) Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Ann Intern Med 132:605–611
Church TS, Cheng YJ, Earnest CP et al (2004) Exercise capacity and body composition as predictors of mortality among men with diabetes. Diabetes Care 27:83–88
Ruiz JR, Sui X, Lobelo F et al (2008) Association between muscular strength and mortality in men: prospective cohort study. BMJ 337:a439
Sigal RJ, Kenny GP, Boulé NG et al (2007) Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med 147:357–369
Larose J, Sigal RJ, Boulé NG et al (2010) The effect of exercise training on physical fitness in type 2 diabetes mellitus. Med Sci Sports 42:1439–1447
Boulé NG, Kenny GP, Haddad E, Wells GA, Sigal RJ (2003) Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in type 2 diabetes mellitus. Diabetologia 46:1071–1081
Vanninen E, Uusitupa M, Siitonen O, Laitinen J, Lansimies E (1992) Habitual physical activity, aerobic capacity and metabolic control in patients with newly-diagnosed type 2 (non-insulin-dependent) diabetes mellitus: effect of 1-year diet and exercise intervention. Diabetologia 35:340–346
Tessier D, Menard J, Fulop T et al (2000) Effects of aerobic physical exercise in the elderly with type 2 diabetes mellitus. Arch Gerontol Geriatr 31:121–132
Raz I, Hauser E, Bursztyn M (1994) Moderate exercise improves glucose metabolism in uncontrolled elderly patients with non-insulin-dependent diabetes mellitus. Isr J Med Sci 30:766–770
Ronnemaa T, Mattila K, Lehtonen A, Kallio V (1986) A controlled randomized study on the effect of long-term physical exercise on the metabolic control in type 2 diabetic patients. Acta Med Scand 220:219–224
Noonan V, Dean E (2000) Submaximal exercise testing: clinical application and interpretation. Phys Ther 80:78–807
Pollock ML, Gaesser GA, Butcher JD et al (1998) ACSM Position Stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc 30:975–991
Stratton IM, Adler AI, Neil AW et al (2000) Association of glycemia with macrovascular and microvascular complications of type 2 diabetes: prospective observational study. BMJ 321:405–412
Wasserman K, Whipp BJ, Koyl SN, Beaver WL (1973) Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol 35:236–243
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60:2020–2027
Reybrouck T, Weymans M, Stijns H, Knops J, van der Hauwaert L (1985) Ventilatory anaerobic threshold in healthy children. Eur J Appl Physiol Occup Physiol 54:278–284
Caiozzo VJ, Davis JA, Ellis JF et al (1982) A comparison of gas exchange indices used to detect the anaerobic threshold. J Appl Physiol 53:1184–1189
Prud’homme D, Bouchard C, Leblance C, Landry F, Lortie G, Boulay MR (1984) Reliability of assessments of ventilatory thresholds. J Sport Sci 2:13–24
Goodpaster BH, Thaete FL, Simoneau JA, de Kelley (1997) Subcutaneous abdominal fat and thigh muscle composition predict insulin sensitivity independently of visceral fat. Diabetes 46:1579–1585
Cuff DJ, Meneilly GS, Martin A, Ignaszewski A, Tildesley HD, Frohlich JJ (2003) Effective exercise modality to reduce insulin resistance in women with type 2 diabetes. Diabetes Care 26:2977–2982
Brownlee M, Cerami A (1981) The biochemistry of the complications of diabetes mellitus. Ann Rev Biochem 50:385–432
Bunn H, Gabbay K (1978) The glycosylation of hemoglobin: relevance to diabetes mellitus. AAAS 200:21–27
McDonald J, Davis J (1979) Glycosylated hemoglobins and diabetes mellitus. Hum Pathol 10:279–291
Hollozy JO (1973) Biochemical adaptations to exercise: aerobic metabolism. Exerc Sport Sci Rev 1:45–72
Kraemer WJ (1994) General adaptations to resistance and endurance training programs. In: Baechle TR (ed) Essentials of strength training and conditioning. Human Kinetics, Windsor, pp 127–150
Wilmore JH, Costill DL, Kenney WL (2004) Physiology of sport and exercise. Human Kinetics, Windsor
Frontera WR, Meredith CN, O’Reilly KP, Knuttgen HG, Evans WJ (1988) Strength conditioning in older men: skeletal muscle hypertrophy and improved function. J Appl Physiol 64:1038–1044
Robergs R, Keteyian SJ (2003) Special topics: performance and health. In: Fundamentals of exercise physiology for fitness. McGraw-Hill, New York, pp 338–366
Staron RS, Karapondo DL, Kraemer WJ et al (1994) Skeletal muscle adaptations during early phase of heavy-resistance training in men and women. J Appl Physiol 76:1247–1255
Staron RS, Leonardi MJ, Karapondo DL et al (1991) Strength and skeletal muscle adaptations in heavy-resistance trained women after detraining and retraining. J Appl Physiol 70:631–640
Honkola A, Forsén T, Eriksson J (1997) Resistance training improves the metabolic profile in individuals with type 2 diabetes. Acta Diabetol 34:245–248
Ibanez J, Izquierdo M, Arguelles I et al (2005) Twice-weekly progressive resistance training decreases abdominal fat and improves insulin sensitivity in older men with type 2 diabetes. Diabetes Care 28:662–667
Morganti CM, Nelson ME, Fiatarone MA et al (1994) Strength improvements with 1 yr of progressive resistance training in older women. Med Sci Sports Exerc 27:906–912
Acknowledgements
This study was supported by grants from the Canadian Institutes of Health Research (grant MCT-44155), the Canadian Diabetes Association (The Lillian Hollefriend Grant) and the Interfaculty Grant programme of the University of Ottawa. The DARE trial investigators include principal investigators R. J. Sigal and G. P. Kenny, co-investigators R. D. Reid, M. Fortier, D. Prud'homme, G. A. Wells, D. Coyle, N. G. Boulé and H. Tulloch, and research coordinator P. Phillips. R. J. Sigal is a Health Senior Scholar of the Alberta Heritage Foundation for Medical Research; he was supported by a New Investigator Award from the Canadian Institutes of Health Research and the Ottawa Health Research Institute Lifestyle Research Chair during the DARE trial. G. P. Kenny was supported by a Career Scientist Award from the Ontario Ministry of Health and Long Term Care. N. G. Boulé was supported by a Postgraduate Scholarship from the National Sciences and Engineering Research Council of Canada. We are indebted to the DARE study participants, and to D. Pepin, K. Fetch, R, Attema, K. Dittmann, K. Phillips, P. Healey, K. Holland, J. Murrin, N. McInnis, J. Fetch and T. Leech, as well as to students in the School of Human Kinetics, University of Ottawa and to the Ottawa-Carleton Regional YMCA/YWCA and Nautilus Plus of Gatineau for their contributions to study coordination, exercise training and evaluation of study participants.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Larose, J., Sigal, R.J., Khandwala, F. et al. Associations between physical fitness and HbA1c in type 2 diabetes mellitus. Diabetologia 54, 93–102 (2011). https://doi.org/10.1007/s00125-010-1941-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-1941-3