Abstract
Aim
The aim of this study was to use a simulation model developed for the scientific evaluation of methodology in disaster medicine to test surge capacity (SC) in a major hospital responding to a simulated major incident with a scenario copied from a real incident.
Methods
The tested hospital was illustrated on a system of magnetic boards, where available resources, staff, and patients treated in the hospital at the time of the test were illustrated. Casualties were illustrated with simulation cards supplying all data required to determine procedures for diagnosis and treatment, which all were connected to real consumption of time and resources.
Results
The first capacity-limiting factor was the number of resuscitation teams that could work parallel in the emergency department (ED). This made it necessary to refer severely injured to other hospitals. At this time, surgery (OR) and intensive care (ICU) had considerable remaining capacity. Thus, the reception of casualties could be restarted when the ED had been cleared. The next limiting factor was lack of ventilators in the ICU, which permanently set the limit for SC. At this time, there was still residual OR capacity. With access to more ventilators, the full surgical capacity of the hospital could have been utilized.
Conclusions
The tested model was evaluated as an accurate tool to determine SC. The results illustrate that SC cannot be determined by testing one single function in the hospital, since all functions interact with each other and different functions can be identified as limiting factors at different times during the response.
Similar content being viewed by others
Introduction
Parallel to a continuously increasing risk for major incidents and disasters as a consequence of the development in the world [1, 2], the vulnerability of hospitals for such incidents has increased [3]. This paradox is considered to be a consequence of the technical development, making it possible to do more advanced procedures, which in combination with an increase of the aging population has raised the expenses of health care and led to increasing demands of efficiency. Every hospital facility has to be optimally utilized, thereby giving little or no reserve-capacity for sudden and unexpected extra loads of injured or critically ill patients [3–5].
As a consequence of this, the previous philosophy that “as soon as all patients are in hospital, the problem is over” is no longer valid. Referring patients that need urgent surgery, or a ventilator, to a hospital where this resource is not available, may lead to a lost patient. Distribution of casualties between hospitals therefore must be done with a proper attention to the current situation in the hospitals [6]. This creates the need of assessing the hospitals surge capacity, defined as the ability to obtain adequate staff, supplies and equipment, structures and systems to provide sufficient care to meet immediate needs of an influx of patients following a large scale incident or disaster [7].
The aim of the present study was to use a scientifically validated simulation model developed for interactive training of medical staff of different categories, supplying information detailed enough to run a training session with real consumption of time and resources, to test the surge capacity and preparedness of a major hospital. This model made it possible to also illustrate the interaction between the different components of the response, which is important to give a more accurate picture of the surge capacity.
Methods
Simulation system used for the test
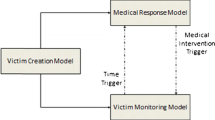
The mass-casualty simulation (MACSIM) system used in this study was originally developed for the scientific evaluation of methodology in the response to major incidents and disasters [8]. It was further developed for interactive training in the international MRMI courses, covering the whole chain of response, where it so far has been used for training of more than 550 responders of different categories and been thoroughly evaluated and validated with regard to accuracy [9, 10].
The main component of the system was the casualty card (Fig. 1). Along the sides of the card, the patient’s condition was illustrated by physiologic parameters according to the ATLS® [11] concept. To each casualty card was connected information on the definitive and complete diagnosis, including trauma score, findings on X-ray, and during surgery, times within certain treatments had to be done to avoid preventable mortality and complications and potential need of ventilator. To the cards could be attached movable priority tags and also tags indicating performed investigations and treatments, all connected to the consumption of time and adjusted to available resources. The simulation system has been previously described [9].
MACSIM casualty simulation card. Along the edges of the card the physiological parameters illustrating the patient’s present condition are indicated (airway, breathing, circulation, disability). In the center of the card (“exposure”), the different injuries are illustrated with a system of simple symbols. Movable markers can be attached to the card, illustrating priority and different treatment and investigations, connected to real time. Photo: Allan Larsson, Medicinsk Bild, Karolinska University Hospital with permission
Design of the test
One week prior to the test, on the same day of the week and on the same time of the day, a thorough inventory of the hospital was made with regard to:
-
Numbers and diagnoses of patients treated in the emergency departments (ED), all different operating theatres (OR), the postoperative units, the intensive care units (ICU), and the wards. In the OR:s, the calculated residual times to complete surgery were recorded. In the intensive care units, estimations were made if, and if so when, the patients could be transferred to other wards.
-
Numbers and categories of all available staffs serving in the hospital, as well as their position in the hospital.
-
Staff in key positions, and in specialties involved in the management of trauma patients, not being on duty in the hospital was asked to give the times when they could be available.
-
Stores of supplies of all kinds expected to be needed when dealing with a large inflow of casualties.
Based on this information, the hospital was illustrated on magnetic whiteboards, including all facilities that potentially could be needed in a major incident:
-
Casualty receiving zone with primary triage.
-
Emergency departments with trauma resuscitation rooms.
-
All surgical theatres.
-
All postoperative units.
-
All intensive care units.
-
X-ray departments.
-
Emergency wards and wards within potentially involved specialties.
All patients in the emergency departments, operation theatres, postoperative units, and intensive care units were illustrated by magnetic cards giving the data collected as above (see Fig. 2a–d) and placed in the position they had at the preceding inventory.
Cards visualizing “normal” patients already being in the hospital when the incidents occurred, or arriving there parallel to the victims from the incidents. Examples of a ambulatory patients, b patients in wards, c patients under surgery, and d patients in the intensive care units. These patients were based on an inventory on a corresponding time and day of the week as the simulated incident
All staff potentially involved in the incident, except staff in wards, was illustrated by magnetic symbols, and also placed at their position at the preceding inventory.
Staff normally working at all the positions involved was recruited to function at all stations on the boards as described above. They were all given an introduction and training on how to use the simulation system prior to the test.
The tested hospital
The tested hospital was Karolinska University Hospital in Solna, a 712-bed hospital located on a distance between 2 and 17, 7 km from the multiple sites of the simulated incident (see below). This hospital is the Level 1 trauma center of Stockholm and incorporates all specialties involved in trauma care. A separate children’s hospital (Astrid Lindgren’s hospital) is located within the same hospital complex.
According to a proposed modification of the regional disaster plan, this hospital was intended to receive all severely injured patients from a major incident in the city. This modification was based on the principle of “normality” assuming that in a major incident, the trauma center should continue to receive all severely injured until its maximal capacity was reached. That was the experience from the Utøya terrorist shootings and bombing in Norway 2011, where all severely injured were successfully concentrated to the Ullevål trauma center in Oslo [12]. This should be made possible by:
-
Referring all less severely injured (according to the triage on scene) patients to other hospitals in the city.
-
Referring all emergency patients not connected to the incident to other hospitals.
-
When needed, transfer of staff with documented trauma competence from one of the other major hospitals in the city to this hospital.
-
When needed, transfer of supplies from other hospitals in the city to this hospital through the regional medical coordination center.
The scenario
As model for the scenario, a real incident, the Madrid train bombings 2004 [13], was used. This was applied to commuter trains in the central city of Stockholm, a city with 2.2 million inhabitants. With short intervals, bomb explosions were indicated to occur in trains at four different positions in the city of Stockholm, in this case resulting in 400 casualties and a large number of fatalities. The injuries were of the same type and distribution as in the Madrid scenario. The Incident Officer on call in the Stockholm health care system was alerted by the Alarm Center according to a prepared protocol adding the prefix “exercise” to all messages.
The rescue and ambulance services decided the time schedule for extrication and transport to hospitals based on the information on the casualty cards, as well as the available transport facilities and distances at the time of the incident. An inventory was made at the ambulance dispatch center to register the actual positions of all available transport facilities, times for response, times for transport to the sites of the incidents, and transport times from the sites to the tested hospital. Triage and treatment—to the extent that was estimated to be realistic and accurate in this situation—was indicated on the cards with the priority and treatment symbols. An initial spontaneous evacuation of mainly less severely injured to the nearest (=the tested) hospital also occurred. During the preceding inventory, also, available transport resources as well as the traffic situation in the city were assessed.
Running of the test
The test was run on a regular day during office hours. Shortly after 10.00 a.m., the first alert from the alarm center reached the incident officer on call at the Stockholm regional medical coordination center who declared a “major incident” and alerted the tested hospital. At this time of the day, most operating theatres were occupied with elective or emergency procedures. Within the following 12 min, three additional alarms came from the alarm center, informing about explosions in commuter trains on three additional locations in the city, resulting in 400 injured with the same type and distribution of injuries as in the Madrid scenario. Evacuation and transport were done with real time based on available rescue and transport resources at the time for the incident and the distance to hospitals.
The primary task of the tested staff at the time of alert was to reorganize the hospital according to the disaster plan. This work was, as in reality, coordinated and led by the hospital incident command group which was activated at the primary alert and was in continuous communication with the regional medical command center and the ambulance service.
The tested staff also had to evacuate the emergency departments, make an inventory of the intensive care units as well as wards with regard to patients possible to evacuate elsewhere. In addition, an inventory of ongoing surgical procedures was necessary to decide on the actual surgical capability and capacity. This work ran parallel with the reception of the first patients from the incident.
All casualties given red priority according to Triage Sort [14] were transferred to the tested hospital. This was an intentional overload to identify the critical limiting factors.
The casualty cards were delivered to the receiving units (“Triage zones”) in the hospital at the times given by the ambulance service. They were registered on arrival by secretarial staff. ED triage was done by a highly experienced team, distributing the casualties between available resuscitation teams or directly transferring them to OR or ICU. Some cases with lower priority were directed to a waiting area.
The staff at all positions then had to examine the patients (=read the casualty cards), make decisions with regard to re-triage, diagnostic procedures, and continued resuscitation and treatment, and indicate those procedures and transfer the patients to the next position in the chain of management.
Experienced observers served as supervisors at every station (Fig. 3) with the tasks to:
Experienced staff supervised the work controlling that the time requested for treatments and transfer of patients was kept, and no treatments were done without appropriate staff and consumption of resources. Protocols were filled in on each position, recording the patient flow through the hospital. Photo: Allan Larsson, Medicinsk Bild, Karolinska University Hospital with permission
-
Make sure that the actions and procedures decided consumed the time and resources actually needed, with attention to the number and qualifications of the attending staff represented by the staff symbols.
-
Indicate worsening (or improvement) of the patient’s condition on the cards according to time passed after injury and treatments done/not done.
-
Declare patients dead when given time limits for certain treatments were exceeded.
-
Make sure that in-hospital transport times corresponded to the preceding inventory.
X-ray (plain X-ray, computed tomography) or ultrasonography could be performed in the ED or in the X-ray department, depending on access to available machines and staff. Radiologists had X-ray pictures available for all positive findings on every patient to give the responsible clinician an answer and also view the images as base for their decision-making.
For patients transferred to surgery, schematic drawings of the findings were presented to the surgeon when the procedure had started. Based on these, they had to decide on surgical strategy. The observers then set the time needed to finish the chosen procedure taking into account the number and qualifications of the surgical team. Times for anesthesia and preparation, closure, and cleaning of theatres were added. A short surgical report was attached to the casualty cards after surgery was finished.
Recording of data
Observers at every station filled in prepared protocols, recording:
-
Times for every patient´s arrival.
-
Time for start and end of treatment.
-
Time and destination for departure.
All tags for treatments/investigations and all surgical reports were left on the casualty cards after the exercise. This made it possible to record all measures taken and also the type and amount of consumed material for these measures, including surgery.
All data from the protocols and casualty cards were put together in an Excel document. With this document as a base, the patient flow and the casualty load on different positions related to time from the alert could be determined. By comparing the casualty load with the simultaneously available capacity, the limiting factors for surge capacity at different time intervals could be identified. The analysis of the document with regard to surge capacity was made by an external expert group to avoid bias.
The test model was evaluated by a combination of oral and written evaluations by all individuals involved. The hospital staff also filled in a questionnaire with regard to their opinion of the disaster plan and proposals for corrections/improvements based on the test. The disaster committee of the hospital collected these recordings as a base for revision of the disaster plan.
Statistics
Distribution of the answers in the evaluation form was processed in SPSS Version 22 (IBM, New York, NY, USA) and presented as medians (MD), interquartile ranges (IQR), and minimum–maximum (min–max).
Results
Total load of casualties
The first alert reached the hospital shortly after 10 a.m. on a regular day during office hours. The first patients were casualties with less severe injuries, spontaneously evacuating the incident sites. Thirty-eight such patients arrived between 15 and 30 min after the incident, before the rescue and ambulance services had the scene under control. This category of patients should have been distributed to other hospitals if the evacuation had been under control of the ambulance service. Two of these casualties (arriving 10.20 and given red priority on arrival to the hospital) appeared to be severely injured and required urgent treatment.
The first ambulance transport arrived to the hospital 10.32. Because of short distances to the different incident scenes and good access to ambulances, severely injured patients then arrived in a rapid sequence with very short intervals (Figs. 4, 5, and 6). From 10.20 until the test was stopped at 12.40 p.m., the hospital was flooded with a total of 113 casualties with red priority. Of these, 98 were brought to the emergency department for adults and 15 to the emergency department for children (<15 years of age).
Patient flow on the Emergency Department (ED) for adults. With 16 parallel teams staffed and equipped for resuscitation of severely injured (red priority) patients, it was possible to handle 16 patients simultaneously (=T max in the figure) but not more, since this category of patients had to be taken care of by the teams without delay. With real consumption of time for all treatments decided by the teams, the capacity reached the limit 90 min after the incident when waiting times begun to reach dangerous levels. This point (1 first red triangle) was registered as the primary capacity limit for this ED. Thirty-two severely injured had at that time been received. However, after having cleared the ED, it was possible to restart the receiving casualties (2 green triangle) additional patients until the lack of ventilators in the hospital set the definite limit for the surge capacity (3 second red triangle). Between (1) and (2), 16 severely injured had to be referred to other hospitals (=A) and after the second break (3) 19 patients (=B), i.e., in total 35 of the 98 severely injured (=red priority) adult patients in the test
Casualty load on the total 49 surgical theatres in the seven different surgical specialty sections of the hospital. Blue color surgical procedures already started when the incident occurred, some of them time-consuming extensive procedures that not could be interrupted. Green color available and staffed theatres. Red color procedures on casualties from the incident. The total surgical capacity of the hospital was very well utilized thanks to a very efficient coordinating team and the surgical capacity was not fully utilized in spite of the heavy load of casualties in this incident
Casualty load on ventilator beds in the six different intensive care units (ICU) of the hospital. Blue color beds used for patients already being under treatment, of which some could be transferred to the wards earlier than planned. Green color beds at disposal, or made available for receiving casualties. Red color beds used for treatment of casualties from the incident. Four hours after the incident, the available ICU capacity was fully occupied by the casualties from the incidents, including ventilator beds kept for patients still undergoing surgery but with need of ventilator. This, however, reflects an unusually favorable ICU situation in the hospital when the incident occurred (see further the text)
Emergency departments
In the emergency department (ED) for adults, 16 resuscitation teams could be mobilized within the first 30 min after the alert. The prerequisites for these teams were that:
-
They were staffed by minimum of two physicians and two nurses, at least one of each category with postgraduate training in trauma management.
-
They had a prepared room or surface to work in, with necessary equipment and facilities for primary management of severe trauma.
This was the maximal number of such teams that could work in parallel in this department according to preceding inventory.
Between 10.32 and 11.30 a.m., all severely injured patients (=red priority) could be taken care of by the resuscitation teams with only minor or no waiting times (Fig. 4). After that time point and with the continuous inflow of patients, the waiting times for access to resuscitation teams started to increase rapidly. At 11.30 and after receiving 32 severely injured patients, the capacity of this department to take care of severely injured patients with acceptable waiting times was exceeded (Fig. 4). At this time, there was still remaining capacity for surgery and intensive care.
Since the aim of the test was to “overload” the hospital, the arrival of patients was not stopped at the time when the capacity of the emergency department was exceeded. This exposed a number of casualties to the risk of not being provided with the medical care they needed. To avoid this situation, it had been necessary to stop the inflow at that point (1 = first red triangle in Fig. 4). After another 30 min, the ED was “cleared” of casualties arriving before 11.30 and could restart receiving casualties (2 = green triangle in Fig. 4), since the capacity for surgery and intensive care was still not exceeded at this point.
At 12.40 (160 min after the incident), the inflow of casualties had to be stopped because of lack of ventilator beds in the ICU (3 = second red triangle in Fig. 4). At that time, it would have been possible to receive additional 31 casualties without exceeding the capacity of the ED.
During the time period of exceeding the ED capacity (11.30–12.00), 16 severely injured would have been necessary to direct to other hospitals (=A, Fig. 4). When the ventilator capacity was exceeded, an additional 19 of the total 98 patients would have been necessary to direct to other hospitals (=B, Fig. 4).
The time the resuscitation teams spent with the patients (blue columns, Fig. 4) was in average 23.3 min (range 7–50). In addition, the teams spent in average 11.2 min for transfer of the patient to the next position in the hospital (blue interrupted lines, Fig. 4). These times varied from none (when the patient could be transferred directly to the emergency wards near the ED) to very long times for transport to distant departments, in some cases passing X-ray on the way because of congestions to the equipment in the ED.
Almost half of the arriving casualties could be taken care of by the teams without any waiting time (red lines, Fig. 4). The rest experienced mostly very short waiting times. Only two patients (just before the capacity was considered as exceeded at 11.30) experienced waiting times exceeding 20 min.
The mean injury severity score of the red-triaged patients was 34.3 (range 4–75) and the mean age 28 years (range 15–80).
In the ED for children, the surge capacity was never exceeded, since the need of simultaneously working resuscitation teams did not exceed the number of available teams with required facilities for primary management of severely injured children.
The total number of casualties received in the ED for children was 15. The mean age of these patients was 10 years, range 4–15. The ISS was in average 22.2, range 5–38.
X-ray
In total, 22 pulmonary X-rays and 4 skeletal X-rays were performed in the ED. The rest of the pulmonary and skeletal X-rays were planned either at the patient´s next destination (ward, preoperative unit, ICU). This was unfortunately not recorded because of lack of serving staff. The relatively low number of investigations was due to the fact that there were not enough equipment available in the ED to supply all parallel working teams with X-ray service.
The same was true for ultrasonography (USG) with only 11 investigations performed in the ED. According to the routines in this hospital, USG was performed by X-ray staff and not by surgeons or emergency medicine physicians.
Thirty-eight computer tomographies (CT) were registered during the primary management. A minority of these was done at the ED, but because of only one available scanner in this department, most patients were transferred to the X-ray department. This consumed considerable transport times for the accompanying resuscitation teams (also illustrated in Fig. 4). CT was not done in circulatory unstable patients.
Retrospective analysis of the total need of X-ray investigations in these patients indicated that all needed X-rays could have been possible to perform without exceeding available capacity.
Surgical procedures
A total of 59 surgical procedures were performed or started during the test period, distributed according to Table 1. Only life- and limb-saving procedures were done during this primary phase after the incident.
The number and distribution of surgical procedures were proportionally almost identical to the corresponding figures in the Madrid scenario, indicating that similar indications and priorities for surgery were applied (the acting staff in Stockholm had no access to these figures from Madrid during the test).
During this test, all surgical activities were coordinated by one single team, having to their disposal in total 49 theatres located in seven different surgical departments of the hospital. Teams and equipment could be moved between the different surgical sections, making it possible to perform surgical procedures also in theatres normally not used for that specific procedure.
The casualty load on the surgical theatres is shown in Fig. 5. Since the incident occurred during office hours, the majority of the theatres were occupied by planned surgical procedures. These were not possible to immediately interrupt at the time of alert. However, at that time, all non-started (and not immediately urgent) surgical procedures were cancelled. As a consequence, an increasing number of theatres were rapidly made available for casualties.
The highest load on the surgical theatres was recorded 2 h after the incident when 41 of the total 49 theatres were occupied, 28 of them by victims from the incident. When the test was stopped, the hospital had good residual capacity for additional surgeries. At that time, many patients in wards, and also ICU, were scheduled to have planned surgical procedures within the nearest hours or days. In none of these cases, the calculated waiting time was considered to involve a risk for life or health.
The need of surgical sets or disposables for these procedures exceeded available supplies only with regard to sets for external fixation of fractures. This was solved during the test by transferring such sets from other hospitals in the region.
Postoperative care
The seven postoperative wards with a total of 54 beds were used both as preoperative care for patients referred to urgent surgery as well as for postoperative care. Because the incident occurred early in the day, there were plenty of beds available and the surge capacity for these units was never exceeded. If more ventilators had been available, this area could also have been used for prolonged postoperative care to some extent releasing the heavy pressure on the intensive care units (see below).
Intensive care
In total, 42 patients were admitted to the six intensive care units of the hospital according to the distribution given in Table 2. All these patients were considered to need ventilator treatment.
When the inventory was done, the capacity for the intensive care was unusually favorable. Thirty-one of the total 68 ventilator beds in the ICU departments were immediately available, and another 10 beds could be made available within 2 h by transferring patients to the wards (Fig. 6). Six ICU-requiring severely burned patients from the incident could be transferred to a burn unit in another hospital.
Despite the favorable situation at the onset of the incident, the available ICU capacity was not enough for this load of patients. At 14.00 (2 p.m.), all ICU ventilators would have been occupied, including those booked for patients undergoing surgery with need of postoperative intensive care with ventilator. There were also additional patients under surgery with such a potential need. This set the final limit for the surge capacity of the hospital at the incident (Fig. 6).
Wards
Thirty-five of the casualties from the incident were directly transferred to wards, according to the distribution illustrated in Table 3. In addition, some of the wards received patients from the ICU units earlier than planned to release beds for patients from the incident. No “regular” patients had to be dismissed from the wards earlier than planned.
Need of supplies
Calculated need of supplies based on the information from the treatment tags attached to the casualty cards is illustrated in Table 4. Material needed for X-ray and laboratory procedures were not registered in this test.
The tested hospital could require additional supplies from other hospitals in the city. The only supplies requested were sets for external fixation of fractures, blood, and intravenous fluids. However, much of the disposables were close to running out during the end of the test period.
Assessment of the hospital preparedness
Assessment of the hospital preparedness to respond to a major incident was done based on experiences from the test combined with the evaluation forms from the participating staff.
It could be concluded that the participating staff in general was well familiar with the disaster plan. Parts of the plan had been trained, as the hospital command function, but not the whole plan before this test was done. Several observations were reported with regard to details in the alert and response procedures that could benefit from improvement.
Two things were specially emphasized:
-
The plan for preparing the emergency department for several parallel working teams with accurate space and equipment needed to be clearer and better structured.
-
The very successful model for coordination of the surgical theatres, which was used in the test, but was not included in the plan, needed to be formalized in the disaster plan with definitions with regard to staffing, authorizations, and action cards.
The command function of the hospital was specially evaluated during the test and was found to function very well as well as the communication and coordination with the regional command center.
Evaluation of the simulation model
The evaluation of the accuracy of the simulation model used for the test is illustrated in Table 5. The number participating clinical staff was 34. A written evaluation form was sent out after the test, and the return rate for clinical staff was 28/34 = 82 %. On a floating scale 1–10, the median ranking of the accuracy of the simulation model was 8 (IQR 1), as well as the ranking of the value of the test for quality assurance of preparedness. The median ranking of the staff with regard to how much their participation in the test had increased their ability to respond to major incident in their present position was 8 (IQR 3).
Around half of the participants would have preferred more than the given time (one training session of 1 h) to prepare themselves. All of them who had read the written information sent out in advance considered the information relevant.
Discussion
Methods to determine surge capacity
It has been shown that hospital’s self-reported evaluations of surge capacity are un-reliable [15], this is why there is a need of objective methods for this purpose. Many attempts have been made to develop such methods, using computerized models [16, 17], virtual reality systems [18, 19], theoretical mathematical models [20, 21], and live exercises with casualty actors [22]. All these models have their limitations. Most of them deal only with only one of the hospital components, usually the emergency department. However, the surge capacity is dependent on all components of the hospital and how they interact with each other. Live full-scale exercises with casualty actors would be very expensive and resource consuming if they should give sufficient information to evaluate the capacity of all these components. In summary, there is so far no standardized and widely accepted model available for determining the overall surge capacity of a hospital.
Surge capacity at different phases of the response
The result of this test, including all the components with impact on the hospitals capacity to receive an unexpected heavy load of casualties, illustrates the hazard in defining the surge capacity based only on single components of the chain of management. The capacity was first exceeded in the ED and the time when the inflow had to be stopped could be defined (Fig. 4, first red triangle). However, the capacity for surgery and intensive care was at that time far from exceeded. If the inflow of patients had been permanently stopped at this time, these important assets would not have been utilized to their full extent. It could also be clearly illustrated that the overloading of the ED was temporary and it was possible after an interval to restart receiving casualties (Fig. 4, green triangle). During that interval, it would have been necessary to refer severely injured patients to other hospitals. Thus, the proposed change of the regional disaster plan for Stockholm, sending all red patients to the single trauma center would have failed with this scenario.
Before the ED capacity again reached its limits, the lack of ventilators became the next limiting factor. This made it necessary to permanently stop the inflow and set the final limit for the hospital’s surge capacity during this test (Fig. 4, second red triangle). However, at that time, the capacity for surgery was still not exceeded. With access to a reserve supply of ventilators, the surge capacity could have been extended to the time when the OR capacity was fully used.
Thus, with the use of this model, it was possible to illustrate;
-
How the different components in the chain of management interacted with each other.
-
That different components became limiting factors at different time intervals during the alert.
-
How measures to fully utilize the capacity of the hospital could be identified.
The validity of the test
It has to be emphasized that the result of this simulation—as for all tests of this kind—is valid only for the corresponding time with regard to the activity in the hospital. This test was done during office hours with all functions in the hospital fully staffed, but also fully occupied with normal health care. If the incident had occurred during non-office hours with only teams on duty available in the hospital, the situation would have been different. The number of resuscitation teams possible to mobilize within the time period and needed to cope with the rapid inflow of patients would have been greatly reduced. In a city with short distances to hospital and good access to transport resources, the inflow of casualties starts very fast and rises to high levels very quickly. At the Madrid bombings, from which this scenario was taken, the nearest hospital received the first patients within minutes and then a total of 272 patients in 2.5 h [13].
On the other hand, during non-office hours, it would probably have gone faster to mobilize surgical theatres, presumed that the hospital had a good disaster plan with a prepared organization to call in staff off duty. In summary, to draw conclusions about surge capacity on a 24-h base requires tests both during office- and non-office hours.
Was the capacity of this hospital to receive 63 severely injured casualties during 2.5 h realistic? The authors serving as external observers had not expected such a high capacity, and it is also high related to other reports on hospital surge capacity. However, it has to be stressed that the results from this test cannot be directly applied to other hospitals or regions without taking into consideration the special conditions valid for this hospital:
-
It is a large university hospital with all surgical specialties, including 49 surgical theatres in seven surgical departments and in total 68 ICU-beds with ventilators.
-
It was intended to receive only severely injured (red priority on scene according to Triage Sort [14]). All less severely injured and other emergencies were during the incident referred to other hospitals.
-
It could request both staff and supplies from other hospitals in the city during the response.
-
It had facilities for 16 resuscitation teams for major trauma working in parallel, which is unusual even for a large hospital.
Furthermore, reports from similar incidents have demonstrated that the load of severely injured casualties of this magnitude during this time interval may occur and has to be planned for [23].
The hypothesis behind this study was that the tested hospital could serve as the only receiving hospital for severely injured in a major incident, according to the model successfully used at the recent terror attack in the neighboring country, Norway [12]. The results from this study illustrates that such a recommendation cannot be generalized. Even if this load of casualties was very high, it is based on an incident that actually has happened. This implies that even if the trauma center should be used as much as possible, there must be a back-up plan to involve other hospitals when the capacity limit—even if temporarily—is exceeded.
With regard to the last point, this test was done during the construction of a new hospital to replace the old one. A test is planned to study the surge capacity of this facility and possibly make some adjustments to improve the hospital’s role as the major receiving hospital in the case of a major incident. The possibility to use it at the planning stage further increases the value to this test model.
The realism of the scenario
This incident was a copy of the Madrid bombings [13] and the type and distribution of injuries taken from that scenario. The difference was that the number of casualties was reduced. This was based on the information given by the commuter train company on the normal number of travellers on the involved commuter trains at that time of the day. The number of casualties must be related to the number of passengers. The rapid flow of patients was in accordance with available transport facilities and distances, and also in accordance with Madrid.
The almost identical proportion of numbers and types of surgical procedures in this test as in the original scenario in Madrid illustrated the capability of the simulation system to mediate information about the casualties of sufficient accuracy to serve as base for decisions with regard to surgical priority and strategy.
A similar scenario was very close to occurring in Stockholm. In December 2010, a suicide bomber was on his way to detonate a bomb in a large storehouse in the center of the city, during the peak of the Christmas shopping. By mistake, he released the bomb before entering the storehouse, killing only himself. If the bomb had—as supposively intended—detonated indoors in the middle of hundreds of crowded people, it could have resulted in a scenario rather similar to the one in the test.
Even if the strategy in Stockholm was to refer all, and only, severely injured to the tested hospital, spontaneous evacuation is unavoidable. This was simulated also in this test—the hospital received around 40 spontaneously evacuated patients with minor injuries only a few minutes after the incident. According to experiences from similar incidents [13, 24, 25] that number probably had been even bigger in reality. However, it filled the function to visualize the problem, and these patients have a minor influence on the surge capacity of the hospital, since treatment can be delayed and they can even be referred elsewhere for treatment. It is also an indication that trauma centers do need preparedness to also receive the less severely injured or so-called “walking wounded”.
Capacity-limiting functions of the hospital
The triage in the emergency department was in the test led by a team with extensive experience of disaster medicine and with the aim to reduce the time in ED to a minimum. Some patients were labeled to be transferred directly to OR (preoperative unit) or ICU, but they still had to pass the resuscitation teams who had to bring them there. That required at least a quick survey of the patient, and it required transport time.
The 16 parallel teams in the ED received a total of 63 patients, which meant in average 4 patients per team during 3.5 h (the teams continued to be busy after the inflow was stopped 12.40, Fig. 4). With the median time for survey and resuscitation/treatment in the ED of 23 min, this should be fully possible also in consideration of the sometimes rather long time for transfer of patients (in average 11 min) and the time needed to reset the equipment between patients.
The times for survey, resuscitation, and decision making were in accordance with the generally recommended maximum times for severely injured in the trauma room: 30 min for circulatory stable and 15 min for unstable patients [26]. More than half of these patients filled the criteria of being unstable at arrival. A faster rotation should of course have been desirable with this heavy casualty load. However, the hospital has rather long internal transport distances and these patients required attention during transport. One very time-consuming measure could be identified: bringing the patient to a CT in another department when the only scanner in the ED was occupied. This emphasizes the need of restriction with such investigations in these situations. According to the evaluation, the use of CT in this test could have been more limited, even if it never was done in unstable patients.
Patients referred to surgery were first sent to the postoperative unit for preparation, deciding priority for surgery and distribution between available surgical theatres. The fact that this was done by one single team, having control of all theatres, made the utilization of theatres very efficient. At the time for the test, this was not included in the disaster plan but is now being considered, based on the positive experiences from the test.
The fact that the incident occurred during office hours caused in this test no significant delay in access to theatres. At the time of alert, the first operation for the day was just finished in some of the theatres and all further elective surgery was immediately cancelled. This provided operating rooms for the most urgent procedures. The delay between arrivals of casualties until they were ready for surgery then showed to be just long enough to avoid waiting times for surgery above critical limits (Fig. 5). At the time of the test was stopped, the hospital had still capacity for additional urgent surgical procedures. However, many patients were at that time waiting for planned, less urgent procedures.
Many of the surgeons in this hospital had international training in trauma surgery and were familiar with the concept of damage control surgery. This influenced the choice of surgical strategy, which kept procedure times low and thus contributed to keep the surgical capacity on a high level.
Looking at the distribution of surgical procedures (Table 1), the number of laparotomies was surprisingly high compared with reports from major incidents of similar kind. Three negative laparotomies raise the suspicion on too wide indications for surgery. These were all done due to multiple penetrating fragments from the explosions. Although studies have shown that a number of penetrating injuries to the abdomen in the civilian setting may only need observation. The strategy in mass-casualty situations is controversial, because non-operative treatment is also resource consuming, requiring close surveillance [27, 28].
The available capacity at the intensive care units of the hospital was surprisingly good at the inventory. Of the total 68 ICU beds with ventilator in the hospital, 31 were immediately available. Another 10 could be made available after 2 h from the alert by transferring patients to the wards. Based on experience from this hospital as well as other hospitals in Europe, such access to ICU-beds is very uncommon. In the daily routine, it is often difficult to find one single available ICU-bed, even in a large hospital.
However, the test illustrated measures that can be taken to increase access to ICU-facilities. The disaster plan of the hospital included plans to alert and call in staff off duty also in wards. Increased quantity of staff in the wards makes it possible to transfer patients from the ICU to wards on the borderline to need intensive care. A number of such patients could be identified during the preceding inventory.
The final limiting factor for the ICU was the number of ventilators. The use of OR ventilators as a temporary solution has been discussed in the literature. This is controversial, and a decision in this hospital was not to use them outside the OR. The access to ventilators was also limited in the nearest hospitals after transfer of patients. A supply of extra ventilators would have increased the capacity, since staff and space were available in the postoperative units.
The access to beds in the wards never became even close to be a limiting factor (Table 3). If the casualty load had included also moderately or less severely injured, the pressure of the wards would probably have been higher. However, experiences from recent incidents of the same magnitude show that the need of hospital beds almost always is overestimated [13, 24, 25, 29]. In the London Bombings 2005, the hospitals were criticized for sending home patients to release beds that were never needed [24]. In the Tsunami disaster in the South East Asia 2004, the six hospitals in the Phuket and Phang Na provinces in Thailand with a total of 1500 beds received more than 3000 patient needing in-hospital care during the first 3 days. This was dealt with using all available space and reserve supplies, providing beds by putting mattresses on the floor [29]. Even if this was an extreme situation, it shows that lack of beds can be coped with, presumed that a sufficient number of staff and supplies can be mobilized.
In summary, this illustrates that (1) efforts to make an inventory of available beds after an alert can be delayed, as it is unlikely to have any influence on the surge capacity and (2) sending home patients from wards should not be started until the need is certified.
Accuracy and potential development of the simulation model
The accuracy of this test is of course dependent on the accuracy of the simulation system used for test. This system is based on real scenarios which secures that the casualty load and also the type and distribution of injuries is realistic.
The clinical staff participating in the test, many with extensive clinical experience, evaluated this model as accurate for its purpose (Table 5) and also considered the test as an important and efficient training. It also gave a good picture of the hospital’s disaster plan. The test served as base for improvement and adjustments of the plan. In this way, the test also served as quality assurance of disaster preparedness, a field where disaster medicine so far has been far behind other specialties in medicine.
Even if a simulation model like this includes involvement of a lot of staff, it is still much less expensive than a test with live casualty actors brought into the hospital [30]. In addition, it can be done with minimal disturbance of the normal activity in the hospital. Once the training system is set up, it can be preserved on magnetic film sheets in rolls [9], ready to reset very quickly. This creates continuous access to a system both for training, quality assurance, and evaluation of modifications of the organization.
Limitations of the study
It has again to be emphasized that no general conclusion with regard to the surge capacity of a large hospital can be drawn from this test. What is presented in this study is a methodology based on a simulation system with a very high level of detail regarding clinical data. This methodology can be used to test any hospital or unit, but every such test has to be based on the specific conditions valid for the tested hospital.
In addition, conclusions with regard to surge capacity of a hospital cannot be drawn from one single test. Defining surge capacity, regardless of method, requires more than one test, and testing should be done both during office hours and non-office hours.
This was the first time this simulation system was used for a test of this kind, covering all functions of a large hospital. A natural consequence of this is a potential for improvement. The number of acting staff in the wards was too small in this test. In this situation, investigations, treatments, and continuous surveys have to be done on the wards to a higher extent than in routine health care. We underestimated this since we did not consider the wards as capacity-limiting factors. As a result of this, a number of ordered investigations (for example, CT) were not done in a proper time. Increasing the number of participating staff would still make the test costeffective with regard to the amount of information gained from it.
Conclusions
-
The used method, based on a real scenario and run with real consumption of time and resources for all involved functions, gave the information required to define the surge capacity of this major hospital and was by the participating staff evaluated as accurate for this purpose.
-
The results illustrate that surge capacity cannot be determined by testing one single function in the hospital, since all functions interact with each other and different functions can be identified as limiting factors at different times during the response.
-
The used methodology was also evaluated as an efficient method to train participating staff and to make an assessment of the hospitals disaster plan.
References
Smith E, Waisak J, Sen A, et al. Three decades of disasters—a review of disaster specific literature from 1777–2009. Prehosp Disaster Med. 2009;24:306–11.
United nations General Assembly, Implementation of the International Strategy for Disaster Reduction, Report of the Secretary-General. A/64/280. http://www.unisdr.org/we/inform/resolutions-reports. Accessed 16 Jan 2016
Altevogt BM, Stroud C, Nadig L et al. Medical surge capacity workshop summary. Washington DC: Institute of Medicine of the National Academies, The National Academic Press; 2010. http://www.nap.edu/openbook.php?record_id=12798&page=1. Accessed 16 Jan 2016.
Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605–11.
The National Academies Press. medical surge capacity workshop summary. Washington DC: The National Academic Press; 2010. http://www.nap.edu/openbook.php?record_id=12798&page=99. Accessed 16 Jan 16 2016.
Lennquist S. The hospital response. In: Lennquist S, editor. Medical response to major incidents and disasters—a practical guide for all medical staff. Berlin: Springer; 2012.
Adams LM. Exploring the concept of surge capacity. Online J Issues Nurs. 2009; 14(2). doi:10.3912/OJIN.Vol14No02PPT03.
Lennquist Montán K, Örtenwall P, Khorram Manesh A, et al. Comparative study of physiological and anatomical triage in major incidents using a new simulation model. Am J Disaster Med. 2011;6(5):289–98.
Lennquist Montán K, Hreckovski B, Dobson B, et al. Development and evaluation of a new simulation model for interactive training of the medical response to major incidents and disasters. Eur J Trauma Emerg Surg. 2014;40(4):429–43.
LennquistMontán K, Örtenwall P, Lennquist S. Assessment of the accuracy of the MRMI-course for interactive training of the response to major incidents. Am J Disaster Med. 2015;10(2):93–107.
American College of Surgeons Committee on Trauma: advanced trauma life support program for doctors. 8th ed. Chicago; 2008.
Englund L, Michel PO, Riddez L et al. The bomb attack in Oslo and the shootings at Utøya, 2011. Kamedo report 97. Socialstyrelsen; 2012. http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18925/2012-12-23.pdf. Accessed 16 Jan 2016.
Turégano-Fuentes F, Pérez-Díaz D, Sanz-Sánchez M, et al. Overall assessment of the response to terrorist bombings in trains in Madrid March 11 2004. Eur J Trauma Emerg Med. 2008;34(5):433–41.
Champion HR, Sacco WJ, Copes WS, et al. A revision of the trauma score. J Trauma. 1989;29(5):623–9.
Valesky W, Roblin P, Patel B, et al. Assessing hospital preparedness: comparison of an on-site survey with a self-reported, internet-based, long-distance tabletop drill. Prehosp Disaster Med. 2013;28(5):441–4.
Franc-Law JM, Bullard MJ, Della Corte F. Accuracy of computer simulation to predict patient flow during mass-casualty incidents. Prehosp Disaster Med. 2008;23(4):354–60.
Abir M, Davis MM, Sankar P, et al. Design of a model to predict surge capacity bottlenecks for burn mass casualties at a large academic medical center. Prehosp Disaster Med. 2013;28(1):23–32.
Greci LS, Ramloll R, Hurst S, et al. vTrain: a novel curriculum for patient surge training in a multi-user virtual environment (MUVE). Prehosp Disaster Med. 2013;28(3):215–22.
Franc-Law JM, Bullard M, Della Corte F. Simulation of a hospital disaster plan: a virtual, live exercise. Prehosp Disaster Med. 2008;23(4):346–53.
Bayram JD, Zuabi S. Disaster metrics: quantification of acute medical disasters in trauma-related multiple casualty events through modeling of the acute medical severity index. Prehosp Disaster Med. 2012;27(2):130–5.
Franc JM, Ingrassia PL, Verde M, et al. A simple graphical method for quantification of disaster management surge capacity using computer simulation and process-control tools. Prehosp Disaster Med. 2015;30(1):9–15.
Kleber C, Cwojdzinski D, Strehl M, et al. Results of in-hospital triage in 17 mass-casualty trainings: underestimation of life-threatening injuries and need for re-triage. Am J Disast Med. 2013;8(1):5–11.
Einav S, Feigenberg Z, Weissman C, et al. Evacuation priorities in mass casualty terror-related events: implications for contingency planning. Ann Surg. 2004;239(39):304–10.
Aylwin CJ, König TC, Brennan NW, et al. Reduction in mortality in urban mass-casualty incidents—analysis of triage, surgery, and resources use after the London bombings on July 7, 2005. Lancet. 2006;368:2219–25.
Pryor JP. The 2001 world trade center disaster summary and evaluation of experiences. Eur J Trauma Emerg Surg. 2009;35(3):212–24.
Boffard K, editor. Manual of definitive surgical trauma care. 3rd ed. London: Hodder Arnold; 2011.
Demetriades D, Hadjuzacharia P, Constantinou C, et al. Selective nonoperative management of penetrating abdominal solid organ injuries. Ann Surg. 2006;244(4):620–8.
Velmahos GC, Constantinou C, Tillou A, et al. Abdominal computed tomography scan for patients with gunshot wounds to the abdomen, selected for non operative treatment. J Trauma. 2005;59:1155–60.
Lennquist S, Hodgetts T. Evaluation of the response of the Swedish health care system to the tsunami disaster in South East Asia. Eur J Trauma Emerg Surg. 2008;34(5):465–85.
McLean CR, Lee YT, Jain S. Integration of incident management simulation-based training applications. Proceedings of the 2007 fall simulation interoperability workshop (SIW), Orlando; 2007. http://www.nist.gov/customcf/get_pdf.cfm?pub_id=822749. Accessed 16 Jan 2016.
Acknowledgments
The authors want to express their gratitude to the Management of the Karolinska University Hospital for providing resources for the preparation and performance of this test. We also want to thank all participating staff of the hospital for invaluable support in the preparatory work, professional performance during the test and valuable feedback on the methodology. This study was supported by the Stockholm County Council, Sweden and the Laerdal foundation, Norway (Grant 2908).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors state compliance with the ethical guidelines in the creating of this manuscript. The preceding inventory of the hospital was done with complete removal of all data connected to individual patients. All staff participated voluntarily.
Conflict of interest
Kristina Lennquist Montán, Louis Riddez, Anna Carin Olsberg, Håkan Lindberg, Dan Gryth and Per Örtenwall declare that they have no conflict of interest. One of the authors, Sten Lennquist, has the copyright for the MACSIM simulation system, developed for scientific and educational purpose. The evaluation of the hospitals capacity and function was done by external observers, also participating as supervisors during the test.
Rights and permissions
About this article
Cite this article
Lennquist Montán, K., Riddez, L., Lennquist, S. et al. Assessment of hospital surge capacity using the MACSIM simulation system: a pilot study. Eur J Trauma Emerg Surg 43, 525–539 (2017). https://doi.org/10.1007/s00068-016-0686-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-016-0686-1