Abstract
Background
On occasion, advanced invasive procedures in pre-hospital care can be life saving. This study aimed to identify the contemporary use of these procedures on a regional doctor-led air ambulance unit, and to define the need, skill set and training requirements for a regional pre-hospital team in the UK.
Methods
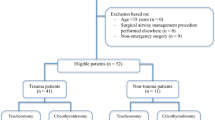
Mission data were recorded prospectively and the database reviewed to identify invasive procedures over a 76-month period. These cases were reviewed with indications, mechanism of injury, presence of cardiac arrest at any time point (±return of spontaneous circulation) and procedural failure or morbidity.
Results
Two hundred and thirty-five procedures were performed: 16 for injuries affecting the airway, 111 for breathing and 108 for circulation. Almost a third of patients in cardiac arrest regained spontaneous circulation. Procedures performed increased fivefold from 2003 to 2009, with a marked increase in the use of thoracostomy and intra-osseous access. Procedural failure or inadequacy was high with needle cricothyroidotomy, needle chest decompression and early intra-osseous access experience.
Conclusions
A steady increase in the number of procedures was observed over time. Less invasive methods of airway and breathing support were frequently inadequate, though definitive surgical airway or chest decompression was effective each time it was performed. Thoracotomy was performed infrequently. There are implications for the training of pre-hospital doctors who work in the majority of the UK.




Similar content being viewed by others
References
Joint Royal Colleges Ambulance Liaison Committee (JRCALC); The Ambulance Service Association (ASA). UK Ambulance Service National Clinical Guidelines (2006). http://www2.warwick.ac.uk/fac/med/research/hsri/emergencycare/prehospitalcare/jrcalcstakeholderwebsite/guidelines/clinical_guidelines_2006.pdf. Accessed 19 Nov 2009.
Roberts K, Bleetman A. An email audit of prehospital doctor activity in an area of the West Midlands. Emerg Med J. 2002;19(4):341–4.
Fullerton JN, Roberts KJ, Wyse M. Should non-anaesthetists perform pre-hospital rapid sequence induction? an observational study. Emerg Med J. 2011;28(5):428–31.
Huber-Wagner S, Lefering R, Qvick M, Kay MV, Paffrath T, Mutschler W, Kanz KG; Working Group on Polytrauma of the German Trauma Society (DGU). Outcome in 757 severely injured patients with traumatic cardiorespiratory arrest. Resuscitation. 2007;75:276–85.
Mistry N, Bleetman A, Roberts K. Chest decompression during the resuscitation of patients in prehospital traumatic cardiac arrest. Emerg Med J. 2009;26:738–40.
Sunde GA, Heradstveit BE, Vikenes BH, Heltne JK. Emergency intraosseous access in a helicopter emergency medical service: a retrospective study. Scand J Trauma Resusc Emerg Med. 2010;18:52.
Hartholt KA, van Lieshout EM, Thies WC, Patka P, Schipper IB. Intraosseous devices: a randomized controlled trial comparing three intraosseous devices. Prehosp Emerg Care. 2010;14(1):6–13.
Scrase I, Woollard M. Needle vs surgical cricothyroidotomy: a short cut to effective ventilation. Anaesthesia. 2006;61(10):962–74.
Flint NJ, Russell WC, Thompson JP. Comparison of different methods of ventilation via cannula cricothyroidotomy in a trachea–lung model. Br J Anaesth. 2009;103(6):891–5.
Mariappa V, Stachowski E, Balik M, Clark P, Nayyar V. Cricothyroidotomy: comparison of three different techniques on a porcine airway. Anaesth Intensive Care. 2009;37(6):961–7.
Dimitriadis JC, Paoloni R. Emergency cricothyroidotomy: a randomised crossover study of four methods. Anaesthesia. 2008;63(11):1204–8.
Difficult Airway Society (DAS). Failed intubation, increasing hypoxaemia and difficult ventilation in the paralysed anaesthetised patient: Rescue techniques for the “can’t intubate, can’t ventilate” situation. 2004. http://www.das.uk.com/files/cvci-Jul04-A4.pdf. Accessed 19 Nov 2009.
Price RJ, Laird C. A survey of surgical airway experiences and equipment among immediate care doctors. Emerg Med J. 2009;26(6):438–41.
Davies GE, Lockey DJ. Thirteen survivors of prehospital thoracotomy for penetrating trauma: a prehospital physician-performed resuscitation procedure that can yield good results. J Trauma. 2011;70(5):E75–8.
Lockey DJ, Davies G. Pre-hospital thoracotomy: a radical resuscitation intervention come of age? Resuscitation. 2007;75(3):394–5.
Stiell IG, Nesbitt LP, Pickett W, Munkley D, Spaite DW, Banek J, Field B, Luinstra-Toohey L, Maloney J, Dreyer J, Lyver M, Campeau T, Wells GA; OPALS Study Group. The OPALS major trauma study: impact of advanced life-support on survival and morbidity. CMAJ. 2008;178(9):1141–52.
Stiell IG, Wells GA, Field B, Spaite DW, Nesbitt LP, De Maio VJ, Nichol G, Cousineau D, Blackburn J, Munkley D, Luinstra-Toohey L, Campeau T, Dagnone E, Lyver M; Ontario Prehospital Advanced Life Support Study Group. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):647–56.
Gräsner J-T, Wnent J, Seewald S, Meybohm P, Fischer M, Paffrath T, Wafaisade A, Bein B, Lefering R; German Resuscitation Registry Working Group, Trauma Registry of the German Society for Trauma Surgery (DGU). Cardiopulmonary resuscitation traumatic cardiac arrest—there are survivors. An analysis of two national emergency registries. Crit Care. 2011;15(6):R276.
Smith RM, Conn AKT. Prehospital care—scoop and run or stay and play? Injury. 2009;40(Suppl 4):S23–6.
van der Velden MWA, Ringburg AN, Bergs EA, Steyerberg EW, Patka P, Schipper IB. Prehospital interventions: time wasted or time saved? An observational cohort study of management in initial trauma care. Emerg Med J. 2008;25(7):444–9.
Ringburg AN, Polinder S, Meulman TJ, Steyerberg EW, van Lieshout EM, Patka P, van Beeck EF, Schipper IB. Cost-effectiveness and quality-of-life analysis of physician-staffed helicopter emergency medical services. Br J Surg. 2009;96(11):1365–70.
Conflict of interest
All authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Essential and desirable criteria for doctors seeking to work on WNAA
Essential Criteria
-
Full GMC registration
-
Registrar level or equivalent
-
18 months experience with acutely ill patients (which must include a substantive post in Emergency Medicine)
-
Regular (weekly) on going exposure to acutely/critically ill patients (A&E, Acute medicine, Acute surgery, Anaesthetics/ICU, Pre-hospital Medicine)
-
Pre-hospital Medicine experience on a regular basis
-
RSI competency
-
ALS or equivalent
-
DipIMC (within 5 years) or ATLS/ BATLS/ PHTLS or equivalent
-
APLS/ PHPLS or equivalent
Desirable
-
Experience with critically ill patients within the last 5 years
-
Emergency Medicine within the last 5 years
-
Weekly Pre-hospital Medicine experience
-
MIMMS
-
DipIMC within 5 years
-
PHEC
-
Competent in scene management
-
Competent in Extrication techniques
-
Completion of RTC course
-
Completion of advanced driving course
-
Completion of Moreton fire college training or equivalent
-
Competent in Pre-hospital acute trauma management Competent in Pre-hospital acute medical management
Rights and permissions
About this article
Cite this article
Shapey, I.M., Kumar, D.S. & Roberts, K. Invasive and surgical procedures in pre-hospital care: what is the need?. Eur J Trauma Emerg Surg 38, 633–639 (2012). https://doi.org/10.1007/s00068-012-0207-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-012-0207-9